Intraoperative and postoperative pain management in aesthetic plastic surgical procedures with limited use of narcotics is a major topic in both the surgery and anesthesia literature. The author describes the evolution of anesthesia and pain management in his 4 decades of practice. We’ve performed over 4000 cases of cosmetic surgery and mostly succeeded in limiting postoperative discomfort and narcotic usage. The article discusses the incorporation of new medications and techniques into practice and reviews the techniques of anesthetic blocks under ultrasonic guidance. Data that documents the improvements in patient care that ensued as these techniques were instituted is also provided.
Key points
- •
How to use enhance recovery after surgery (ERAS) protocols to provide a limited to narcotic free anesthetic for plastic surgical cases. Describe what medications are used and why.
- •
Describe each of the different ultrasound-guided blocks to provide pain relief during the procedure as well as into the postoperative period to limit narcotic usage.
- •
Describe the different types of anesthesia that can be used for outpatient plastic surgery and expand on what medications and techniques can be used.
- •
Describe the advantages of using a laryngeal mask anesthesia versus endotracheal intubation for plastic surgery procedures, specifically for head and neck surgeries.
- •
A discussion on the use of long-acting amide anesthetics such as Exparel (Pacira, Tampa, Fl) based on current literature and personal experience.
Introduction
This article describes my approach to the practical management of perioperative and postoperative anesthetic and pain management in patients undergoing common cosmetic surgical procedures.
I will discuss how my approach has evolved, both in conjunction with the evolution of my specialty and also because of my interaction with the aesthetic plastic surgeons with whom I have worked for the past 35 years. We have instituted ERAS protocols originally described for the hospital setting to avoid the potential for postoperative nausea and vomiting and narcotic abuse. When possible, we avoid endotracheal intubation, laryngeal mask anesthesia (LMA), and instead use total intravenous sedation for the majority of our aesthetic cases. Our approaches are described for some of the most common cosmetic procedures done at our center.
The author provides a summary of the types and techniques of ultrasound-guided blocks that he has personally performed, which have been transformative to our practice and to the cosmetic plastic surgeons with whom the author has worked at our center. These blocks are performed after the induction of anesthesia before the surgeon beginning their case. As a believer in pre-emptive anesthesia, the author believes that preventing the transmission of nerve impulses related to the surgery from the skin to the spinal cord to the brain and blocking the release of hormone-like substances that are released in response to surgery (such as prostaglandins), gives rise to less pain at the conclusion of the surgical procedure. Regional blocks enormously reduce postoperative discomfort. We suggest the possibility that these blocks could enjoy wider use in cosmetic surgical practice to reduce narcotic usage and to enhance patient satisfaction. They virtually eliminate the need for intraoperative and postoperative narcotics with their known incidence of postoperative nausea and vomiting as well as addiction. There is a learning curve to these techniques that can easily be mastered by most anesthetic providers.
Techniques of anesthetic blocks under ultrasonic guidance are reviewed and our protocols for many of the most commonly performed cosmetic procedures done at our surgical center is discussed. The author provides data that documents the improvements in patient care that ensued as these techniques were instituted.
Every anesthesiologist and every cosmetic surgeon will have preferences based on their training, their experience, new techniques and technologies as they emerge, and on the evolving medical literature. Herein described is our individual approach that has been instituted successfully. Where appropriate, we provide evidence-based literature that agrees with our approach. We also discuss approaches that are conflict with our approach and provide clinical experience to justify it.
Aesthetic surgical procedures include all facial and eye plastic surgical procedures, (including rhinoplasty, blepharoplasty and face and neck lift) and breast and body procedures (including breast augmentation, breast reduction, and mammoplasty, abdominoplasty brachioplasty, thigh lift, and various subcutaneous energy-based treatments).
We will describe our.
- 1.
Preop assessment for patients accepted at surgical center including a discussion of American Society of Anesthesiologist (ASA) risk assessment, marijuana use, glucagon-like peptide (GLP)-1 medications and obesity.
- 2.
ERAS protocols
- 3.
Our intraoperative measures for airway and anesthetic management that will discuss whether to use an oral airway, LMA, flex LMA, or endotracheal intubation. LMA inflation pressures/volumes will also be discussed.
- 4.
Our techniques of ultrasound guided blocks. Types of ultrasound machines available (standalone vs handheld).
- 5.
Our IV sedation protocols
Before instituting the changes to anesthesia practice in 2014, almost 100% of patients getting aesthetic surgery procedures received narcotic, whether in the operating room (OR), the postoperative anesthetic care unit (PACU), or at home. Since 2018 when we began tabulating our data, in over 4000 cosmetic surgical cases the use of narcotics has gone from 97% to 3% of patients, with widespread patient and surgeon acceptance.
Postoperative Pain Strategies
New nerve blocks, such as ultrasound-guided PECS blocks by Bianco [ ] in 2011 followed by other fascia plane blocks are used to limit narcotic use and aid in postoperative pain relief.
Preoperative assessment
All patients before coming to the surgical center do an online comprehensive assessment of their medical conditions, medications, allergies, and anesthetic history of problems. Specific questions about cannabis use and whether it is medical or recreational and frequency are also asked. These are usually done at least 5 days before surgery so that if any significant problems are noted they can be addressed. A preoperative nurse initially goes through the data and if any specific abnormalities are noted they have an anesthesiologist sign off on the case. If further information is required, it can then be done in a timely manner before the surgical date. Sometimes if the information is not received the surgeon is notified and the case may then be rescheduled for when the information becomes available. This has led to a very rare history of cancellation on the day of surgery.
As cannabis use has become more widespread, we noticed that these patients had more anesthetic complications than nonusers. These included difficulty in inducing an anesthetic state whether sedation or general anesthesia (GA), more propofol needed, some arrythmias, and respiratory difficulties due to hyperreactivity [ ]. Cannabis users may have difficulty with postoperative pain and a potential for higher pain scores and increased opioid requirements. We instituted a policy that required all cannabis users, some medical users excluded after discussion with the patient, to stop their usage 3 days before their surgery [ , ].
As GLP-1 medication usage has increased, especially for its use for weight loss, we saw instances of aspiration that required emergency intubation and transfer to the hospital. As these medications can cause a delay in gastric emptying [ ], we instituted a policy of a 2-day clear liquid diet to give an extra day for elimination of solids. On the day of surgery, an ultrasound of the stomach was performed if the anesthesiologist had that skill. If it was determined that the stomach was empty , the case was performed as though the patient was not on a GLP-1 medication. If the anesthesiologist was not skilled in performing ultrasound of the stomach, then many of these patients were performed under endotracheal intubation that would have otherwise been performed under sedation. This was left to the discretion of the anesthesiologist involved.
Obesity is an obvious problem in the United States. At the surgical center, we actually perform preop and postop bariatric surgical endoscopies. We have performed those in patients with body mass index (BMI) as high as 65. Most of our stretchers and OR tables can handle up to at least 750 pounds. All of the following procedures have been performed in obese patients at the center after a careful medical and anesthesia physical evaluation by the anesthesiologist taking care of the patient. In some of these patients who would typically be done with deep sedation an LMA is used instead. We do not use a specific cut off of BMI. All necessary difficult intubation equipment is available the same as at the main hospital.
Ambulatory enhanced recovery after surgery (ERAS) protocol
ERAS protocols ( Guidelines—ERAS Society [erassociety.org ]) for [ ] mainly inpatient procedures have been developed by the ERAS Society in order to reduce narcotic usage, decrease recovery time for patients, and allow for a better outcome. At the author’s outpatient surgical center, we modified these to virtually all the procedures done there.
The patients are encouraged to take 1000 mg acetaminophen at home before coming to the center. At the center, most are given 100 mg celecoxib po. For breast and abdominal plastic cases, 100 mg gabapentin po is also given. For the facial cosmetic cases, many of our surgeons prescribe gabapentin (Neurontin) in doses of 100 to 300 mg as well as Aprepitant 40 mg to be taken at home before coming to the center. Further specifics of the different cases will be discussed in the section under each procedure.
Anesthetic techniques
Over the 35+ years this author has been in practice, inhalation agents have evolved from Halothane R , Ethrane R , and Forane R to Sevofluorane R , which is now used primarily at our center. In 1989 propofol was introduced and replaced Sodium Thiopental as the primary agent used for sedation and for GA. The unique rapid on and off mechanism of propofol allowed its use from deep sedation to a form of general anesthesia without a breathing tube . With its introduction, cases needing anesthesia changed from a Versed-fentanyl or Versed-ketamine based anesthetic with the surgeon injecting local anesthesia to a propofol-fentanyl or propofol-ketamine combination.
We currently use ketamine preferentially over fentanyl because of its unique properties as a pain reliever and because, unlike fentanyl, it does not depress respirations. Initial IV dosing of 5 to 20 mg accompanied by propofol (dosing) prevents the dysphoric issues and hallucinations associated with the drug. This allows for the surgeon to inject the surgical field with local anesthetic without patient movement. For areas where local anesthetic may not be sufficient, ketamine supplemented with propofol or a small dose of dexmedetomidine (Dex) 5 mcg IV (see below) can be given to allow the surgery to proceed without patient movement.
LMA has been a staple in our ambulatory surgery practice and is the preference for some of our cosmetic surgeons. While some anesthesiologists feel that LMA should only be used for cases under a certain number of hours, 2 to 3 [ ], there is no literature or studies to confirm this, we have not found that its use to be a deterrent even in cases that last as long as 8 hours. The advantages of LMA are numerous. It avoids risks to the vocal cords, has a lower incidence of laryngospasm during emergence, and doesn’t require visualization of the vocal cords on insertion. While LMA does have a greater incidence of coughing, and sore throat, these issues resolve quickly following surgery [ ]. Rarely, a patient may develop a more severe problem, but this is equally the case with endotracheal intubated patient. Care must be taken to properly inflate the LMA (30 mL air for a 3, 40 for a 4, and 50 for a 5) the same as an endotracheal tube (ETT). Problems tend to occur due to too high of a pressure in the cuffs against the tissue over the duration of the procedure. In appropriate patients, and with discussion with the surgeon, in some patients we will use the flexible LMA so that the surgeon can suture it to a tooth and drape it into the field so they can move it around during the case.
The risk of aspiration is theoretically described as a greater possibility with LMA and potentially worse in patients with gastroesophageal reflux disease (GERD). It is worthwhile to note that we have not seen aspiration in over 1600 cases since LMA was introduced into our practice. Our technique for placement of patients with a history of GERD is to elevate the back of the OR table 15–20° for the case. This will help prevent passive regurgitation in those that are prone to it such as the obese and morbidly obese.
Our Current Perioperative Local Sedation
The introduction of Dex in 1999 allowed us to avoid LMA and do many cases under deep sedation. This is accomplished with a bolus of propofol, 50 to 100 mg at a time, combined with ketamine 5-10 mg IV for the surgeon to inject the local. A continuous infusion of low dose propofol, dose varies with patient and placement of local. Also, an infusion of ketamine (0.25 to 1 mg/kg/hr.) is also started. If the patient does seem to respond despite the infusions, a 10 to 20 μg bolus of Dex is given, and the surgeon injects more local anesthesia into the field.
Many of these spontaneously breathing patients need an oral airway to avoid obstruction.
Typically, depending on the extent of the head and neck surgery, nasal canula delivery of oxygen at 3 to 5 L/min allows oxygenation in breast and body cases. Lower flows (2 L or less) in facial plastic surgery cases can be used. The anesthesia provider must communicate directly with the surgeon in these latter cases and potentially shut off O 2 flow when safe to allow for cautery or laser treatments such as for laser blepharoplasty or for laser resurfacing. In these latter cases, O 2 is turned off and a small 5 to 10 mg bolus of ketamine is given.
Another combination we have used successfully in practice involves continuous infusions of ketamine and Dex. Neither causes respiratory depression, and each has side effects opposite of the other, so they tend to cancel each other out. Ketamine can cause tachycardia, hypertension, and an increase in tracheal secretions, while Dex causes bradycardia, hypotension, and a decrease in secretions. We use this technique in patients where the surgeon wishes to avoid any breathing devices, including oral airway such as rhinoplasty or lip lifts. In these cases, the provider must watch the patient’s O 2 saturation to keep it above 90% when the oxygen dissociation curve starts its decline, so the surgeon can use the Bovie around the airway as well as laser to the face without a fire risk.
Ultrasound-guided blocks for aesthetic surgery cases: indications and techniques
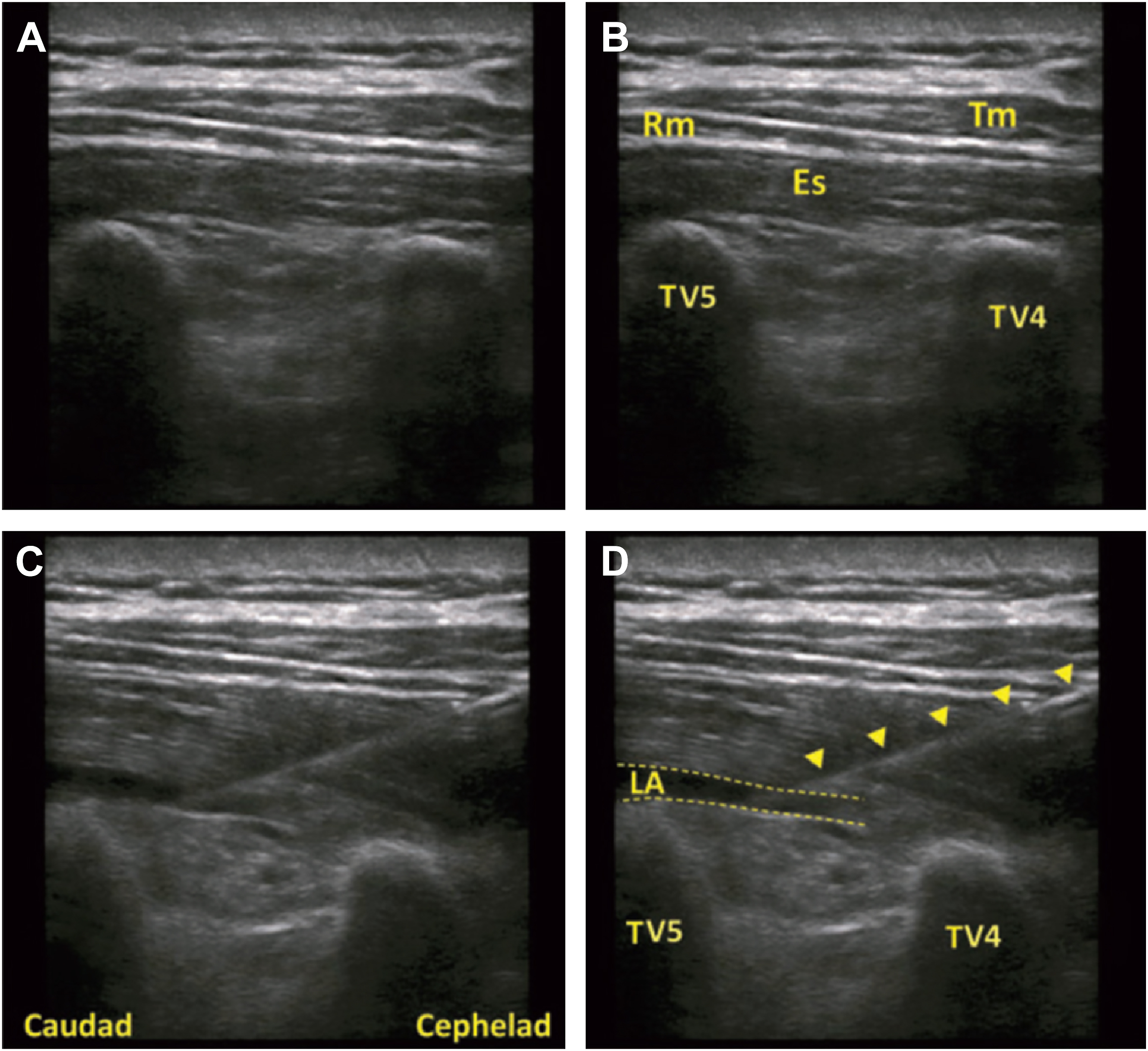
Since 2014, we have used ultrasound guided blocks to dimininsh postoperative discomfort successfully as an accompaniment to cases performed under local with sedation with the above-described techniques.
At our institution, we have come to prefer ropivacaine over bupivacaine for the local anesthetic for blocks due to its lesser cardiac toxicity. The concentration varies with the maximum based on the patient’s weight and other local the surgeon may inject and may vary from 0.2% to 0.5%. All blocks this author performs have dexmethasone added to them to prolong their duration [ ]. In addition, the erector spinae plane blocks used for the breast implant removal cases have Dex 10 mcg per 20 mL of local added to prolong the block of the larger spinal nerve segments.
Not all of my colleagues add adjuvants to their blocks. This author finds that steroids significantly add to the duration of block and patient satisfaction on postoperative phone calls done on days 1 to 3; before their use this author found less satisfaction and greater opioid use (unpublished data).
- •
Erector spinae plane (ESP)
- ○
Indications
- ▪
T2 (neck, shoulder, arm, clavicle)
- ▪
T4 (chest)
- ▪
T5 (breast implant removal) combined with PECS1
- ▪
T9 (abdomen)
- ▪
L2 (laminectomy, thigh lift, hip)
- ▪
L4 (hip, knee)
- ▪
- ○
Additives in solution
- ▪
Dexamethasone 4 mg per 20 mL local anesthetic (LA)
- ▪
Dex 10 mcg per 20 mL LA
- ▪
- ○
Volume/dose
- ▪
10 to 15 mL LA per side
- ▪
20 mL LA per side
- ▪
If doing a combined breast and abdomen procedure then 15 mL LA per needle
- ▪
- ○
Effectiveness
- ▪
Depending on what spinal area you are targeting, it spreads 5 to 6 segments around the injection site. As an example, if injection is done at T5 in a cephalad to caudad direction I would expect T3 to T7 or T8 distribution
- ▪
- ○
Complications
- ○