A broad range of complications of cosmetic upper and lower blepharoplasty is summarized in
Table 3.1.
Table 3.2 lists specific complications encountered by the author in an oculoplastic referral practice (
1).
Table 3.2 divides complications into those that tend to occur in the upper lid and those that occur in the lower lid. Complications may be categorized as “functional” or “cosmetic.” Functional unfavorable results require repair in order to maintain proper eyelid function, whereas cosmetic unfavorable results do not meet the patient’s expectations but eyelid function is not compromised. The broad range of complications is discussed here.
Eyelid and Deep Orbital Bleeding with Possible Loss of Vision
Measures taken to avoid bleeding are discussed in
Chapter 1 and reemphasized here. Nonsteroidal antiinflammatory agents such as Motrin and Advil should be stopped 5 days prior to surgery. Aspirin products and vitamin E ideally should be stopped 3 weeks prior to surgery. Clopidogrel (Plavix) is stopped for 1 week (see
Chapter 1). The prescribing physician is consulted before discontinuing any medications. Herbs such as gingko biloba, ginger, garlic, ginseng, and fish oils, and certain Asian foods, including mushrooms, affect platelet function and therefore may interfere with the normal blood clotting. All such herbs ideally should be stopped 3 weeks prior to surgery. Of prime importance is a previous history of bleeding after other surgeries, including dental surgery. Hypertension should be controlled prior to elective cosmetic surgery. During surgery, monitored sedation reduces the risk of intraoperative bleeding and possibly postoperative bruising and edema. Herbs including Arnica montana, bromelain (found in pineapples), and papaya appear to significantly improve bruising and edema. Unfortunately,
no controlled study has yet demonstrated the efficacy of such herbs in cosmetic eyelid or even facial surgery. Rarely, vitamin C deficiency undetected prior to surgery and corroborated by serum ascorbic levels was found in postoperative patients with bleeding (
2). Administration of vitamin C in such patients resulted in immediate reversal of the bleeding problem (
2). A dietary history may help detect such deficiencies.
Deep orbital hemorrhage has been estimated to occur in 1 of 25,000 cases of blepharoplasty (
3). In two cases of unilateral permanent visual loss following foureyelid blepharoplasty due to orbital hemorrhage, electrophysiologic tests as well as computed tomography and clinical examination demonstrated that optic nerve dysfunction rather than retinal ischemia was the main cause of vision loss (
4). Appropriately timed orbital decompression is crucial to management. This mechanism has been found in other cases (
5,
6), although central retinal artery occlusion also has been reported (
7). In any event, proptosis, with limited motility, and a fixed dilated pupil require emergency treatment, including topical Timoptic 0.5% ophthalmic drops to reduce intraocular pressure, intravenous mannitol and acetazolamide, head elevation, ice compresses, and systemic corticosteroids administered every 12 hours. At the same time, the systemic blood pressure must be monitored and controlled. Hematologic studies including serum prothrombin time (PT), partial thromboplastin time (PTT), and platelet count are obtained. The surgical wounds are opened and hematoma evacuated. Any bleeding points are cauterized. Immediate canthotomy and orbital decompression should be considered. Orbital computed tomography may delineate a localized hematoma. The orbital decompression is crucial. Ideally such complications are initially managed in a hospital emergency room.
Infection
The signs and symptoms of infection usually start gradually 3 to 4 days after surgery. Allergy to topical medication may be confused with infection, but allergy often starts after only a few doses of the topical medication and the predominant symptom of allergy is generally itching. Edema and redness of the skin may accompany allergy or infection. Allergy may occur in response to the topical ophthalmic antibiotic itself or to the preservative. A follicular tarsal conjunctival reaction may be evident on slit lamp examination. Similarly, severe dry eye resulting from exposure keratitis may be associated with conjunctival injection and mistaken for infection or allergy. Most commonly, such patients do not blink because of discomfort; therefore, signs and symptoms generally start as the swelling decreases 3 to 7 days after surgery. Conjunctival injection tends to be limited to the exposed palpebral fissure. Infection may be heralded by decreased vision due to tearing and mucous discharge, pain, swelling, and erythema. However, any inflammatory condition, including allergy or dry eye, may be associated with mucous discharge, tearing, and blurred vision. Typically, dry eye signs and symptoms improve with increased frequency of blinking.
A rare cause of fulminant apparent cellulitis accompanied by diffuse tense edema, “ruptured violaceous bulla” with overlying focal area of necrosis, and anesthesia suggest group A β-hemolytic streptococcal infection. Such infections have occurred after cosmetic blepharoplasty in healthy patients (
8,
9 and
10). Medical stabilization of the patient, prompt hospitalization and administration of systemic antibiotics, appropriate debridement, and consideration of hyperbaric oxygen (2.4 atm for 100 minutes per day) can be lifesaving.
Delayed infection with erythematous raised eyelid nodules, particularly when a foreign body is implanted weeks after periocular surgery, should arouse suspicion of an atypical mycobacterial infection. The median time onset of infection in 13 periocular cases was 3 months (
11). Eight cases occurred after cosmetic blepharoplasty (
11). Such infections may mimic a chalazion, develop along the incision, or occur without any inflammatory signs. Orbital abscess formation may occur in the setting of transconjunctival blepharoplasty. Cultures for acid-fast bacilli and excisional biopsy of nodules with performance of acid-fast stains are necessary for diagnosis and may be sufficient for treatment. The infection in one patient resolved after local excision of eyelid lesions. Needle biopsy of the lesion confirmed the diagnosis in one patient (
11). In most cases, prolonged treatment with oral clarithromycin eradicates infections. Appropriate antibiotic treatment is guided by culture results and clinical response. Consultation with an infectious disease specialist may be advisable. One patient developed recurrent infection after 4 weeks of antibiotic treatment. Sequelae of infection may include eyelid scarring with ectropion and retraction and enophthalmos (
11).
Wound Dehiscence
Wound dehiscence is an uncommon event in the author’s experience, even with the use of absorbable sutures of the 6-0 caliber. A small dehiscence should heal by secondary intention without sequelae.
Undercorrection, Overcorrection, and Lagophthalmos
Other risks of blepharoplasty include undercorrection or removal of too little skin and protruding fat. Consideration for additional revisional surgery can only be
made when the swelling has decreased and healing has occurred sufficiently, usually a minimum of 6 months after surgery. Early surgical intervention may only worsen the condition.
In the case of overcorrection, excision of too much upper eyelid skin may cause lagophthalmos or inability to close the eyelids. A full-thickness skin graft harvested from the retroauricular skin is implanted in the upper eyelid after conservative treatment with topical lubricants has failed. Such treatment rarely is necessary except when there is a severe shortage of upper eyelid tissue. The graft should be positioned so that its inferior edge is sutured to the eyelid crease and the bulk of the graft is camouflaged in the superior sulcus. Generally, exposure symptoms gradually resolve over weeks to months after surgery. Such skin grafting may be cosmetically unacceptable and should be delayed for at least 6 months unless corneal breakdown necessitates earlier intervention.
Removal of too much fat may leave the individual with a hollow, skeletonized, unhealthy aged appearance. Again, any correction should be delayed for at least 6 months to 1 year after the initial surgery. Surgery should always avoid overcorrection because it is easier to take additional tissue away at a later date than to replace excised tissue. This subject is addressed in detail by Dr. Shorr and colleagues in
Chapter 5.2A.
Complications of Concomitant Blepharoptosis Repair
Postoperative blepharoptosis may result from (a) insufficient correction of a recognized upper lid blepharoptosis, (b) failure to diagnosis or treat a preexisting ptosis or unusual cause of ptosis such as myasthenia gravis, or (c) inadvertent surgical violation of the levator aponeurosis with resultant iatrogenic levator dehiscence. The demands of the patient who has blepharoptosis and undergoes concomitant cosmetic upper and lower eyelid blepharoplasty may be greater than those of the patient with functional blepharoptosis because the lid position and contour must be corrected but also upper eyelid crease and fold must be symmetric.
Undercorrection
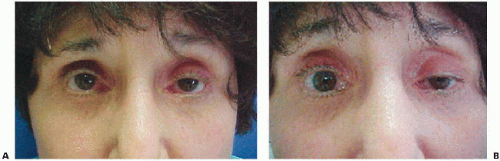
Old photographs are extremely useful, as demonstrated in a case presentation of a 70-year-old woman who underwent ptosis surgery and cosmetic lower blepharoplasty (
Fig. 3.1). Ten days after surgery, the patient and her husband were extremely unhappy. The right upper lid position was approximately 1 mm lower than the left upper lid, but the patient indicated that the tarsal plate was more exposed on the right undercorrected than the left upper eyelid. Review of old photographs demonstrated the lower upper eyelid creases in youth compared to the
high creases due to bilateral upper lid levator dehiscence. A high eyelid crease was unacceptable and a cosmetically important concern of this patient. The right upper eyelid from a functional standpoint was acceptable.
After a careful discussion of the risks and benefits with the patient and her husband, who was a practicing attorney, a revision of the undercorrected right upper lid was performed. The patient had full knowledge of the remote possibility of the final result being jeopardized and worse than the initial result. The patient was well aware that the surgeon believed the present eyelid position was functionally acceptable. Some residual asymmetry was evident, but the patient was extremely happy with the result. Due to underlying dry eye, excessive upper eyelid elevation is limited. Moreover, a brow lift would only have accentuated the hollow in the supratarsal fold and may have contributed to dry eye.
Overcorrection
Corneal exposure and, if significant, cornea breakdown and possible infection may result from overcorrection. In some patients, eyelid retraction results in a purely cosmetic problem with few, if any, symptoms of exposure keratitis.
Case Report
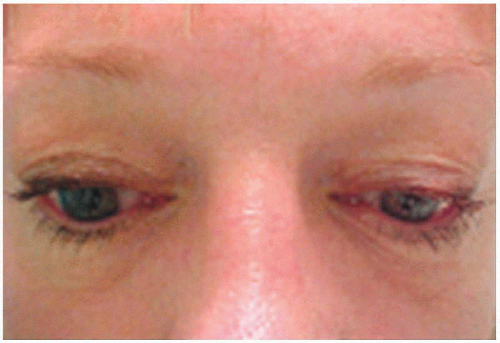
A 55-year-old woman underwent four-lid cosmetic blepharoplasty right upper lid ptosis repair and face lift (
Fig. 3.2). Upon examination 1 year after surgery, the marginal
reflex distance was 6.5 OD (right eye) and 3.5 OS (left eye) with moderate lid lag on downgaze. An adequate tear film was evident on slit lamp examination and confirmed on Schirmer testing. Eyebrow to upper lid margin distance was 27 OD and 29 OS. Levator function was 18 mm OU (each eye). The patient underwent a large levator recession without insertion of a spacer graft with an excellent result.
Ptosis revisions, whether to repair overcorrections or undercorrections, ideally are performed within 2 weeks of surgery to avoid late surgery and scarring that accompanies multiple surgeries. In some cases, excessive postoperative edema may not allow for appropriate judgment of the eyelid position and revisional surgery within the 2-week period. Such patients may require later revision. In the author’s experience, revision after 14 days may be difficult due to scarring and the consequent need for sharp dissection.
Dry Eye, Conjunctival Chemosis, Reflex Tearing, and Keratopathy
After cosmetic eyelid surgery in which there is temporary eyelid dysfunction, transient dry eye is common, especially in patients with a history of dry eye. As stated earlier, transient dry eye is common after blepharoptosis repair. The thickened edematous eyelid does not blink normally and may result in a poor blink or even transient lagophthalmos. In addition, increased evaporation of tears due to greater surface exposure after blepharoptosis repair results in symptoms of temporary dry eye and lagophthalmos after surgery.
Two weeks after surgery, blinking is decreased by tightness of the scar tissue. The evolution of a scar is extremely slow. Myofibroblasts or contractile elements within fibroblasts generally relax by 3 to 4 months (
14). This tightness rarely may take 1 year to completely decrease. In patients with borderline dry eye, the blink may decrease so that more of the ocular surface is exposed and dries with resultant irritative tearing.
Once healing is complete, Flowers (
15) has estimated that between 26 to 30 mm of skin between the eyebrow and upper eyelid margin is required for normal eyelid contour invagination at the eyelid crease and normal closure once the eyelid crease is firmly established by his anchor technique. Such measurements allow a minimum of 1 cm for the eyelid crease and fold or “invagination process,” and
12 mm from the edge of the eyelid fold to the brow as well as 3 to 6 mm of visible pretarsal skin (
15). Although these numbers are helpful guidelines, clinical evaluation of factors including adequacy of the tear film and the number and completeness of blinks is equally important.
Persistent Eyelid and Conjunctival Edema
Canthoplasty whereby the upper and lower eyelids are surgically incised at the lateral canthus predisposes to conjunctival edema. In contrast, canthopexy serves to support and elevate the lateral canthus, but the upper and lower lids are not divided. Chemosis has not been more than a transient problem in the author’s experience unless a lateral canthoplasty and tarsal strip procedure are performed. In contrast, canthopexy rarely causes persistent conjunctival chemosis. Occasionally chemosis is evident 1 week after surgery, especially in elderly patients when significant dissection and resection are necessary. Primary blepharoplasty rarely requires a canthoplasty. Secondary revisional surgery for lower lid retraction often requires a canthoplasty. A laterally placed transmarginal lower lid traction suture and application of topical corticosteroids help prevent chronic conjunctival edema.
In most cases of chemosis, topical lubricating eye drops and sometimes topical steroids such as Tobradex (Alcon, Fort Worth, TX) four times per day for 5 to 7 days or fluorometholone (FML) (Allergan, Inc., Irvine, CA) for persistent cases are necessary for 1 to 2 weeks. Intraocular pressure must be monitored, especially in patients with a family or personal history of glaucoma because such patients may be more prone to intraocular pressure elevations. Massage twice a day for 2 to 3 minutes when the conjunctiva prolapses over the lower eyelid margin is helpful. Topical lubricants without preservative, along with patching, may enhance the massage effects, especially if an exposure element exists (
16,
17).
Recalcitrant chemosis unresponsive to appropriate topical corticosteroids, patching, and compresses may respond to refixation of the loose conjunctiva in the fornix. Incision of the conjunctiva across the lower cul-de-sac and insertion of double-armed 4-0 chromic sutures may help reconstitute the detached ligaments in the conjunctival fornix. The double-armed sutures are brought through the deep tissues just beneath the inferior conjunctival edge, then through the tissue just below the superior edge and finally through the wound at the same level. A temporary tarsorrhaphy may be necessary to augment the effect.
Exacerbated Blepharitis
Blepharitis is common with aging, especially in patients with concomitant dry eye, and may be exacerbated by eyelid surgery. Medical treatment of blepharitis includes commercially available eyelid scrubs, topical antibiotics, warm compresses, and over-the-counter artificial tear preparations.
Scarring of the Skin and Deeper Structures
Skin incisions made with carbon dioxide lasers sometimes cause permanent hypopigmentation of the skin or lightening of the skin due to decreased melanin pigment (the opposite of skin tanning). This problem is accentuated in African-Americans, Asians, and patients of Mediterranean descent; thus, laser skin incisions
should be avoided. This tendency accentuates the eyelid scar. For this reason, during laser blepharoplasty, skin incisions are performed with a cold blade. Deep scarring may affect the blink and result in transient dry eye.
Double Vision
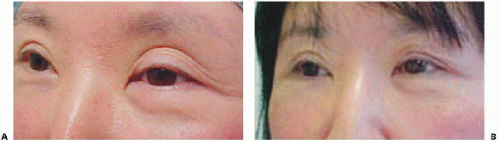
Double vision after any eyelid surgery is rare; if it occurs, it usually is transient. The muscle may become weak from inadvertent injection of anesthetic directly into the inferior oblique muscle. Excessive cautery in the nasal fat pad may cause damage to the superior oblique tendon. Other possible causes are direct injury with resultant hematoma and toxicity due to injection of local anesthetic. The nerve to the superior oblique cannot be damaged because it lies within the orbit. Injury to the inferior rectus muscle may result in hypotropia with restricted elevation (
Fig. 3.3). In a series of 12 patients, 7 patients demonstrated inferior rectus paresis after lower blepharoplasty, and the remaining 5 patients had superior oblique damage. In 1 of these 5 patients, an acquired Brown syndrome was noted such that the involved eye did not elevate in adduction. Inferior rectus injury was associated with scarring and fat adherence with restrictions to upgaze rotation as evidenced by positive forced duction testing. In such patients, a transconjunctival approach was used. An incision too close to the globe or bulbar conjunctiva rather than 3 to 4 mm below the inferior tarsal border may predispose to this complication due to the proximity of the inferior rectus (
18).
Lower eyelid fat repositioning has been associated with conjunctival chemosis and scarring of the transposed fat, as well as vertical diplopia due to ocular restriction (
19). In the two reported cases, the condition did not resolve after 6 weeks and the fibrous band was incised via a transconjunctival approach. In the second case, only 2 days after surgery, the vertical globe restriction was released by removal of the suture maintaining the repositioned fat and by lysing any scar tissue between the orbital fat and the orbital rim (
19).
Transient Numbness in the Upper Eyelid
Patients, especially women, often note decreased sensation in the upper lid when they put on makeup. This finding has always been transient but may take several months to dissipate (
20). In a study of 83 eyelids of 50 patients undergoing upper lid blepharoplasty or ptosis repair, a Cochet-Bonnet filament-type aesthesiometer was used to measure sensation at the 1-week, 1-month, and final (2-6 months) time periods after surgery. The degree and duration of sensory loss and the extent of recovery during the evaluation period were evaluated. All but 4 of the 68 eyelids tested at the 1-week postoperative time period had a measured loss of sensation. Of the 44 eyelids tested at the final time period, all but one had regained some or all of this sensory loss. The authors conclude that loss of skin sensation in the eyelid after upper eyelid crease incision blepharoplasty or blepharoptosis repair occurs in most patients and should be considered an expected outcome of the procedure. Partial to complete recovery of eyelid sensation over 2 to 6 months also should be expected. In rare instances, recovery does not occur.
Suture Cysts (Milia)
Milia usually form along suture lines and result from epithelialization of suture tracts that contain keratin debris. The cystlike contents of each milium can be expressed with a 30-gauge needle in the office. More persistent suture cysts may require electrocautery after use of topical dermal anesthetic with topical anesthetic cream or local infiltrative anesthesia.
Pyogenic Granulomas
Pyogenic granulomas that form at the conjunctival edge of the surgical wound are not uncommon. They may slough spontaneously, but occasionally they require excision after a trial of topical antibiotic steroid drops (
21,
22).
Poor Upper Lid Crease Formation with Asymmetric Upper Eyelid Folds
A poor eyelid crease may be improved by placing interrupted sutures that include bites of the wound’s skin edges with an intervening bite of the underlying levator aponeurosis. In order to further increase the depth of the scar, a deep 7-0 Vicryl (polyglactin) suture or nonabsorbable Prolene suture can be used to secure the edge of the orbicularis muscle to the lower portion of the wound to the fused septum
and levator aponeurosis (
Fig. 3.4). Alternatively, in the anchor-type formation of the crease as defined by Flowers (
15), a bite is taken through the partial-thickness superior tarsus, then through the edge of the levator aponeurosis and finally through the edge of the orbicularis muscle from the inferior skin muscle edge. In some patients, poor lid crease formation may produce lateral hooding of the upper eyelid fold over the lateral aspect of the eyelid crease. Because the eyebrows may be in excellent position, a brow lift will not completely correct the lateral hooding without a blepharoplasty and reformation of the eyelid crease. When the brow is elevated manually, the poorly formed lid crease is not corrected. Surgical elevation of the brow of sufficient height to diminish the redundant upper eyelid fold would only serve to possibly distort the eyebrow (see
Chapters 1 and
4.6).
Superior Sulcus Hollowing
A cosmetically unacceptable deep superior sulcus may be improved by dermis fat grafting (
23). The unpredictable absorption rate of implanted fat alone is compensated by the dermis fat graft. The dermis portion of the graft increases its survival. The dermis fat graft may be harvested from the skin just above the iliac crest. The area is mobile, non-weight bearing, and non-hair bearing. Some surgeons prefer the skin of the underside of the female breast where the breast tissue meets the skin of the chest wall.
In order to correct upper eyelid hollowing (see
Chapter 5.2), a horizontal ellipse measuring 3 to 4 cm × 1 to 2 cm is harvested from abdominal skin above the iliac crest. The donor site of the proposed graft is marked with a marking pen and incised with a no. 15 blade into the dermis. The epidermis and superficial dermis then are excised. The full-thickness dermis is penetrated and the abdominal fat is incised using a no. 12 blade. Three double-armed 6-0 polypropylene sutures are placed through the edge of the dermis of one side of the graft and then through the skin orbicularis oculi muscle layer well above the superior incision. In this manner, the dermis is surgically positioned directly against the posterior orbicularis muscle and the fat portion of the graft is pointing posteriorly against the levator aponeurosis and muscle (
Fig. 3.5). The wound is closed by skin-to-skin interrupted sutures that include deep bites of the inferior edge of the dermis-fat graft. In a
series of five patients, one developed ptosis due to the weight of implant, which was oversized in order to compensate for its later resorption (
24).