The Ulthera system is a facial application of intense focused ultrasound developed for improving noninvasive rejuvenation results. This article describes the Ulthera device, its mechanism of action, the indications and limitations of the device, and the details of treatment. We also review the literature and our personal results, discuss future trends, and conclude with advice for the early user.
- •
For most nonsurgical methods of facial rejuvenation, improvement is dependent on a robust wound healing response consisting of increased expression of reparative mediators and neocollagen deposition.
- •
The ideal patient has mild to moderate skin laxity and mild lipoptosis. A younger patient typically has a more vibrant wound healing response and an inherent skin elasticity, which leads to better results.
- •
Limitations of the procedure include patients with extensive skin ptosis/laxity, heavy lipoptosis with jowling, and marked platysmal banding. These patients are better served with surgical interventions.
- •
Relative contraindications include treatment directly over keloids, implants, and fillers because it may cause further scarring, malfunction, or volume loss, respectively. Judgment should be exercised in patients at risk for bleeding complications, poor wound healing, infection, or exacerbation of an autoimmune disorder.
![]() V ideo of U lthera T echnique accompanies this article at http://www.facialplastic.theclinics.com/ .
V ideo of U lthera T echnique accompanies this article at http://www.facialplastic.theclinics.com/ .
Emergence of Ulthera
The demand for facial rejuvenation has increased as patients from the baby boomer generation continue to age and subsequent generations find further societal acceptance of such interventions. Traditional surgical techniques and ablative skin resurfacing remain the gold standard for substantial, predicable improvement for those with extensive neck and facial skin laxity, deep rhytids, jowling, platysmal banding, and lipoptosis. Once shrouded in secrecy, master techniques are now readily shared and have become further refined to improve safety and outcomes. However, not all patients present with such extensive aging changes and some cannot accommodate a lengthy downtime in their schedules. In response, a multitude of alternative noninvasive treatment options have evolved to meet the demand of these patients.
These noninvasive treatment modalities include injectable neurotoxins and dermal fillers (hyaluronic acid, calcium hydroxyapatite, and poly- l lactic acid), intense pulsed light, nonablative lasers (infrared 1100–1800 nm, midinfrared 1320-nm neodymium-doped yttrium aluminum garnet, and pulsed dye), and radiofrequency bulk heating (monopolar and bipolar capacitive). Of these treatments, neurotoxins and fillers are the most frequently used and continue to see an exponential growth because of their ability to treat dynamic rhytids and the volume losses of aging, respectively. However, their role in facial tissue tightening and skin rejuvenation is minimal. Common to the other treatment modalities is an attempt to induce this effect through thermal heating of the dermis without injury to the overlying epidermis. This technique largely avoids the negative aspects of the traditional methods (ablative lasers, dermabrasion, and chemical peels), including pigment changes, scarring, infection, and the delay in return of normal activities during reepithelialization. Pain relief is not necessarily eliminated. For instance, early radiofrequency devices were noted to be painful. Later modifications to decrease pain resulted in reduced efficacy and the need for repetitive treatments. As is frequently the case, invasiveness and efficacy are directly related. With nonsurgical methods, improvement is dependent on a robust wound healing response consisting of increased expression of reparative mediators and neocollagen deposition. Quantitative studies have shown that traditional methods can achieve a 1000-fold increase in these factors, whereas noninvasive modalities result in only a fraction of the response. This finding partially explains the more modest results with these noninvasive modalities. The options for nonablative treatments need to continually improve to meet the desires of consumers seeking a low-risk, minimal-downtime procedure with results that closer mimic traditional methods. To this end, a facial application of intense focused ultrasound (IFUS), the Ulthera system (Ulthera, Mesa, AZ, USA), has recently been developed for the goal of improved noninvasive rejuvenation results.
Ultrasound as a Therapeutic Modality
Although more familiar as a diagnostic imaging modality, ultrasonography has been investigated as a therapeutic modality for more than 60 years. Early studies, conducted by Fry and colleagues, focused on the biologic effects and neurologic applications of ultrasonography. This early work failed to find clinical usefulness, but in recent decades ultrasonography is finding an emerging role in the treatment of both benign and malignant solid tumors. In 2004, the US Food and Drug Administration (FDA) approved a magnetic resonance imaging-guided focused ultrasonography device for the treatment of uterine fibroids. Clinical trials are active for the management of benign prostate hypertrophy and malignancies of the breast, liver, kidneys, prostate, and brain. In addition, nonablative ultrasonography modalities are being investigated for targeted drug delivery and gene therapy. In contrast to the applications for high-intensity ultrasonography that accomplish tissue disruption through thermal effects and the cavitation process, IFUS uses heat alone. This situation is the result of shorter pulse durations of 50 to 200 milliseconds, a higher frequency of 4 to 7 MHz, and a decreased energy quantity of 0.5 to 10 J administered through the transducer. As a result, more precise energy delivery is achieved with the Ulthera IFUS device during the aesthetic improvement of facial tissues.
In 2004, Ulthera began preclinical trials with a prototype device, followed shortly thereafter by several clinical trials. White and colleagues reported the first aesthetic use of focused ultrasonography and its ability to specifically target the superficial muscular aponeurotic system (SMAS). By 2009, the significant results of these studies led to an FDA approval for a browlift indication. This approval has fostered the further development of the device as a noninvasive tool for full facial rejuvenation. Moreover, it has created an enthusiastic community of practitioners investing in the device both in the domestic and in the global markets. Therefore, in this article, we further describe the device and mechanism of action, give our impression of its indications and limitations, detail the treatment, review the literature and our results, discuss future trends, and conclude with the pearls and pitfalls we have identified that might help the early user.
Device Details and Mechanism of Action
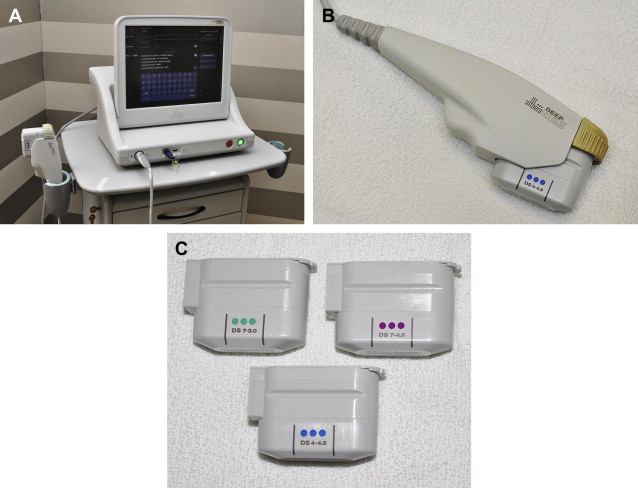
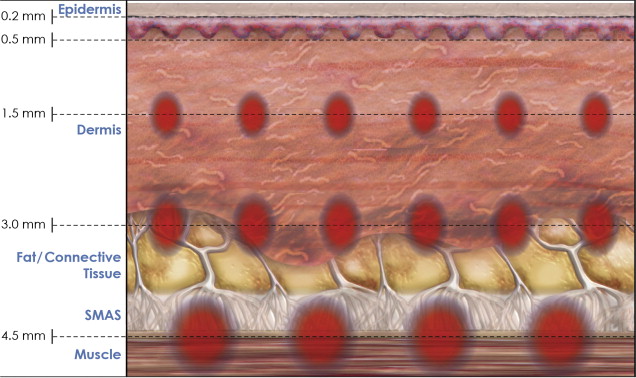
The Ulthera system is composed of a power unit, a central processor with monitor, and a handpiece with 4 interchangeable dual-functioning transducers ( Fig. 1 ). Each handpiece uses high-resolution diagnostic ultrasonography that is capable of clearly imaging the targeted facial anatomy, including the epidermal/dermal unit, subcutaneous fat, and SMAS, facial mimetic musculature, and the underlying osseous structures, up to a depth of 8 mm ( Fig. 2 ). This strategy also allows confirmation of coupling between the handpiece and the skin before treatment initiation. In addition, the handpiece hosts the IFUS transducer responsible for energy delivery. The transducer options include the 4-MHz, 4.5-mm focal depth (4-4.5), 7-MHz 4.5-mm focal depth (7-4.5), 7-MHz 3.0-mm focal depth (7-3.0), and the 7-MHz 3.0-mm focal depth narrow (7-3.0N). These options differ in their geometric focus and wavelength configurations, whereby the depth and quantity of energy delivered during treatment can be varied for a desired effect within the target tissue layer.
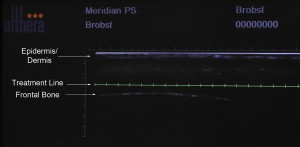
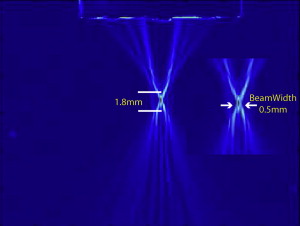
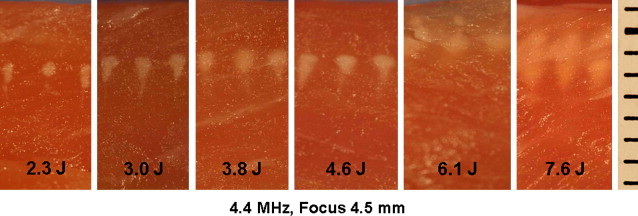
Each transducer delivers a highly directed, acoustic energy wave to a precise focal point ( Fig. 3 ). Energy absorption causes intermolecular vibration and heat production (greater than 60°C), sufficient for collagen denaturation. This situation creates a thermal injury zone (TIZ) or thermal coagulation point (TCP) of coagulated tissue at the target area. The unfocused acoustic energy surrounding this focal point creates insufficient heat for tissue disruption and therefore limits injury to an approximately 1-mm 3 to 1.5-mm 3 focus. Mathematical modeling and prototype studies agree that as energy is increased, there is deeper penetrance but circumferential enlargement remains minimal. Instead, wedge-shaped TIZs at the focal point elongate toward the epidermis as cigar-shaped lesions ( Fig. 4 ). However, even with energy transmission up to 8 J, the epidermis is spared thermal injury. The most powerful commercial Ulthera transducer, the 4-4.5, delivers only 1.2 J to its target focus at a depth of 4.5 mm, making epidermal injury unlikely. In addition, wavelength and tissue penetrance are directly related, thus giving the longer wavelength from the 4-MHz transducer, a more robust and deeper treatment depth than the alternative 7-MHz transducer at a 4.5-mm focus. This method allows targeted treatment to the deeper fibromuscular layer of the cheek and jawline, and should be avoided in more superficial tissues. Conversely, the 7-3.0 transducer delivers less energy at a more superficial depth and can be used around the thinner tissue of the eyes. With this knowledge, the handpieces can be selected to treat the fibromuscular SMAS or the deep dermis in a gridlike pattern ( Fig. 5 ). Each firing of the device creates a 25-mm linear array of TCPs on the full-sized transducers. The number of TCPs vary from 17 to 22 points per line, with spacing from 1.1 to 1.5 mm apart depending on the transducer. With parallel lines performed approximately 3 mm apart, a grid of TCPs with untreated intervening tissue is created. This pattern of injury has been related to the model of fractionated lasers. Similarly, the wound healing response is then elicited, leading to collagen remodeling and dermal thickening through inflammatory mediators.
Patient Selection
The ideal patient has mild to moderate skin laxity and mild lipoptosis. In addition, a younger patient typically has a more vibrant wound healing response and an inherent skin elasticity that leads to better results. Similarly, smoking and extensive photoaging decreases the skin quality and elasticity, resulting in less dramatic results when compared with patients with healthier skin.
Contraindications for Ulthera
Few absolute contraindications exist for the device. Patients with open wounds or severe cystic acne fall into this category. Relative contraindications include treatment directly over keloids, implants, and fillers because it may cause further scarring, malfunction, or volume loss, respectively. In addition, because this is a new device, testing has not been performed in many patient populations. Therefore, judgment should be exercised in patients at risk for bleeding complications, poor wound healing, infection, or an exacerbation of an autoimmune disorder or other comorbidity.
Limitations of Ulthera Procedure
Limitations of the procedure include patients with extensive skin ptosis/laxity, heavy lipoptosis with jowling, and marked platysmal banding. These patients are better served with surgical interventions. Patients with mild and moderate findings are more likely to be successful, but appropriate counsel is necessary, because improvement is not seen in every patient. As treatment protocols continue to develop, benefits and limitations will become clearer.
Anesthesia
A degree of discomfort is expected with the Ulthera device, but this is variable in quantity. In the study by Alam and colleagues, which used topical anesthetic ointment before treatment, scores of 3 to 4 on a 10-point visual analogue pain scale were most commonly reported. The few patients with increased pain scores were those naive to previous facial cosmetic procedures. In our experience, brief periods of pain are frequently elicited with treatment adjacent to osseous structures such as the mandible, orbital rim, and malar eminence. Also, repetitive regional treatment significantly increases the discomfort level, and therefore changing locations temporarily can be helpful.
Many methods have been described, alone and in combination, to manage pain during the procedure. These methods include antiinflammatory medications, oral and intravenous analgesics, anxiolytics, topical and local anesthetics (infiltration or field blocks), conscious sedation, distraction techniques, and cold techniques. Infiltrative anesthetic should be used judiciously within the areas to be directly treated, because the fluid distortion may alter the cutaneous/subcutaneous level being treated. Our current protocol includes a combination of oral ketorolac 20 mg and diazepam 10 mg initiated before treatment, with distraction and cooling techniques during the procedure. In addition, facial field blocks are performed at the patient’s discretion. With this protocol, patient comfort has been significantly improved.
Technique
An Ulthera treatment is initiated by adequately cleaning the face and obtaining preprocedure standardized digital photographs ( Video 1 ). The patient is then placed in the supine position and the face is divided into the desired treatment areas ( Fig. 6 ). These areas include the neck, cheek, lateral orbit, infraorbital, and brow regions. The thyroid cartilage, inferior mandibular border, zygomatic arch, orbital rim, midpupillary line, and the location of superficial facial nerve branches serve as landmarks in this process. Next, each region is marked with a planning card to determine the number of treatment columns necessary to cover the area with minimal overlap ( Fig. 7 ). Then, within each column, the measured density is calculated to quantify the number of lines of treatment ( Fig. 8 ). These markings then serve as a guide during the procedure.
The Ulthera device is rapidly learned and is user friendly. Decisions during use are limited to the appropriate transducer selection and the number of lines desired during treatment. Ultrasound gel is first applied and the handpiece is placed perpendicular to the skin ( Fig. 9 ). Correct coupling and transducer depth are then verified through the ultrasound images on the monitor. Adjustments should be made before treatment because it can lead to incorrect targeting of energy. Unlike the prototype device in which the Joules, pulse duration, and TCP spacing were variable, selection of these variables is now largely irrelevant. Joules delivered is usually set at the default maximum levels, and a change in the energy setting is decided on only if the treatment is poorly tolerated. Treatment is then begun within the neck region and continued upward as each region is completed in a deep to superficial manner. Typically, treatments are performed at 2 depths with 1 pass of a 4.5-mm transducer and then re-treating the area with a superficial 3.0-mm transducer ( Fig. 10 ). The thin tissue of the infraorbital region is an exception, and is treated only at the superficial focal depth. The narrow transducer is also helpful in this location secondary to its small footprint. In the neck and cheeks, the initial pass is usually with the 4-4.5 transducer. This transducer delivers more energy (maximum 1.2 J/TCP) to the subcutaneous and SMAS layers than is possible with the 7-4.5 transducer (maximum 1.05 J/TCP). In the upper face, the 7-4.5 transducer is more frequently used for the first pass. The 7-3.0 transducer is then used to tighten the skin and completes the treatment in most protocols.








