24. Treatment of Prominent Veins
Edward J. Ruane, Girish S. Munavalli
PROMINENT VEINS1
■ Can occur in the presence or absence of either symptoms or an underlying functional venous disorder2
■ Present in up to 50% of individuals
■ Risk factors include:
• Advancing age
• Family history
• Ligamentous laxity
• Prolonged standing
• Increased BMI
• Smoking
• Sedentary lifestyle
• History of trauma
• History of venous thrombosis
• Arteriovenous shunting
• High estrogen states, including pregnancy in women
■ Telangiectasias, often referred to as spider veins, are most common.
■ Varicose veins are dilated, elongated, tortuous, subcutaneous veins ≥3 mm.3
■ Goals of treatment
• Improvement of symptoms (including pain or aching, heaviness, swelling, dry and/or irritated skin, and tightness)
• Improvement of appearance
TREATMENT OPTIONS
CONSERVATIVE MANAGEMENT
■ Extremity elevation
■ Exercise
■ Compression therapy
SCLEROTHERAPY
Indications
■ Treatment of choice for most superficial leg veins
■ Appropriate for the treatment of telangiectasias, reticular veins, and small varicose veins4
Contraindications
■ Acute venous thrombosis or phlebitis
■ Pregnancy
■ Diabetes mellitus (relative)
■ Moderate to severe peripheral artery disease (relative)
■ Patent foramen ovale (relative)5
Preoperative Evaluation
■ For patients who are asymptomatic but find the cosmetic appearance of their veins distressing, sclerotherapy can be performed after physical examination without further diagnostic studies, because these patients are unlikely to have underlying venous reflux.
■ Symptomatic patients should undergo further evaluation with venous duplex imaging to identify the presence of superficial or deep venous insufficiency.
Informed Consent
■ Veins will lighten and become less noticeable but may not completely disappear.
■ Multiple treatments are typically required to achieve the desired effect.
■ Hyperpigmentation is a relatively common complication.
TIP: Veins are documented photographically before each treatment and reviewed with the patient periodically.
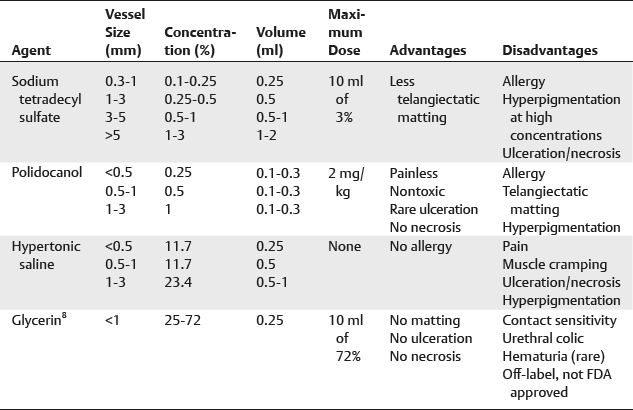
Equipment6–7 (Table 24-1)
Table 24-1 Common Sclerosing Agents for the Treatment of Prominent Veins
Technique
■ Sclerosants may be used in their liquid form or mixed with room air as a foam, to increase their surface area for the treatment of larger veins.
■ Tessari method involves using a three-way stopcock and two syringes, mixing air with liquid to create a foam.9
■ After the sclerosant liquid or foam (with or without lidocaine) is mixed into a syringe at the appropriate concentration, attach the syringe to a 27- or 30-gauge needle.
■ Place the patient in Trendelenburg position to discourage refilling of injected veins.
■ Apply alcohol to clean the area, introduce the needle into the vein, aspirate to ensure intraluminal position, and inject using a low pressure, a fixed amount of the sclerosant.
■ Withdraw the needle, apply compression, and massage the treated area to prevent refilling of the injected vein.
■ Secure a compressive dressing in place with tape while advancing to other treatment areas.
SENIOR AUTHOR TIP: The use of 2-way Baxa connectors are an easier, more rapid way to generate foam.
TIP: Larger underlying reticular veins should be obliterated before more superficial telangiectasias are treated.
Postoperative Care
■ Compressive stockings should be worn continuously for at least 24 hours and then daily for 2-3 weeks.10
■ Avoid strenuous exercise and sun exposure for 2-4 weeks.
■ Repeat injections are not performed for at least 4-6 weeks.
■ Clearance of 60%-80% of treated telangiectasias, reticular veins, and small varicose veins can be expected.11
SENIOR AUTHOR TIP: In the sclerotherapy consultation, inform patients that new spider veins will occur over time and annual maintenance treatments are encouraged.
Complications12
■ Minor
• Pain
• Ulceration
► Reported incidence: 1%-5% of patients treated
► Usually small and heal with local wound care in 4-6 weeks
• Telangiectatic matting
► Consists of multiple, fine dilated vessels in the area of the injection site
► Relatively common, occurring in 15%-24% of patients
► Usually resolves within 3-12 months13
► Check for the presence of local feeding vessels
► Consider treating using sclerotherapy with 72% glycerin
► Minimize incidence by using the minimum strength concentration of sclerosant to achieve effective treatment
• Hyperpigmentation
► Caused by deposition of hemosiderin in the skin
► Occurs in up to 30% of patients
► Resolves spontaneously in 80% of patients within 2 years
SENIOR AUTHOR TIP: Minimize incidence of matting and hyperpigmentation by using the minimum strength concentration of sclerosant to achieve effective treatment.
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree






