15 Treatment of crow’s feet
Summary and Key Features
• Treatment of crow’s feet with botulinum toxin is safe and effective, with predictable cosmetic results
• Preoperative assessment of the periocular region, including analysis of dynamic and static rhytides, lower lid laxity, and upper lid ptosis, can improve the precision and safety of treatments
• A snap-test can be useful for measuring lower lid laxity
• Stretching the skin and side lighting can help avoid injection into superficial vessels and resultant ecchymoses
• Superficial injections into the dermis, combined with frequent needle changes, may reduce injection discomfort, ecchymoses, and / or spread into nearby lip elevators
• Adjunctive non-invasive procedures of the periocular region, including laser resurfacing, pigment laser treatments, and soft tissue augmentation, may be combined with crow’s feet injections for more comprehensive periorbital rejuvenation
Anatomy of ‘crow’s feet’ lateral orbital rhytides
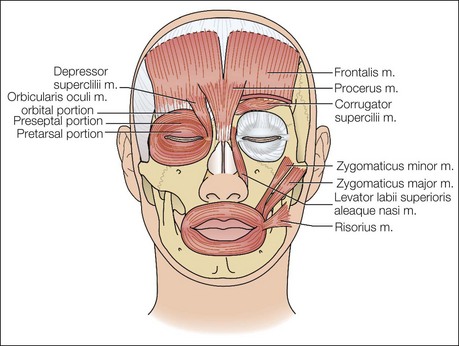
In addition, rhytides develop in the setting of hyperkinetic muscle contractions of the orbicularis oculi, an elliptical muscle that functions in closing the eyelids and protecting the globe by acting as the sphincter of the eye. The orbicularis oculi encircles the eye, with a predominantly vertical orientation at the lateral canthus, and has three distinct subparts: the orbital, palpebral, and lacrimal portions. The lacrimal portion of the muscle runs deep to the lacrimal sac and inserts on the upper and lower eyelids at the tarsal plates. Contraction of this part of the muscle draws the eyelids against the globe and compresses the lacrimal sac, thus assisting tear flow. The palpebral portion is the innermost aspect of the muscle and passes into the eyelid superficial to the septum from the bifurcation of the medial palpebral ligament to the lateral palpebral raphe. The palpebral portion is subdivided into preseptal and pretarsal components, and each portion is superficial to the corresponding named portion of the eyelid. Contraction of the palpebral portion of the orbicularis oculi provides less forceful involuntary closure of the eyelid, as with blinking. The orbital portion represents the outermost aspect of the muscle overlying the bony orbit, with origins at the nasal process of the frontal bone, frontal process of the maxilla, and the medial palpebral ligament. This portion of the muscle blends into surrounding musculature, interdigitating at its superior aspect with the frontalis muscle, corrugator supercilii, depressor supercilii, and procerus muscles, and at its inferior margins with the levator labii superioris alaeque nasi, levator labii superioris, and zygomaticus minor and major muscles (Fig. 15.1). By providing forceful eye closure and eyebrow depression, this outer aspect of the muscle pulls on overlying skin and contributes most to the formation of lateral orbital rhytides. The outer orbicularis is typically treated with botulinum toxin, although the preseptal aspect of the inferior palpebral portion of the orbicularis oculi can be treated in some situations as well. The zygomaticus muscles, both major and minor, can also contribute to inferior periorbital rhytides, as contraction of this muscle elevates skin superiorly into the periocular region. The zygomaticus major originates deep to the orbicularis oculi muscle at the zygomatic bone just anterior to the zygomaticotemporal suture line and courses diagonally where it inserts into the modiolus, lifting the corner of the mouth. The zygomaticus minor muscle courses from the zygomatic bone and inserts into the upper lip, where it causes upward and lateral elevation of the oral commissure. The risorius muscle originates from the connective tissue and fascia overlying the parotid gland, platysma, and runs horizontally towards the oral commissure, where it inserts into the modiolus. Contraction of this muscle pulls the mouth laterally, retracting the corners of the mouth.
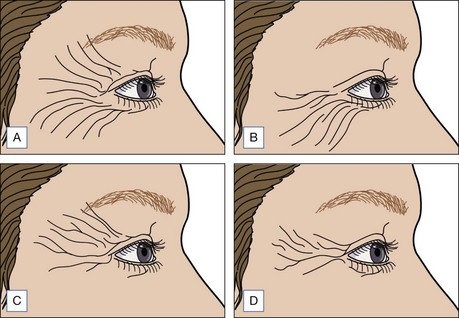
In an article by Kane et al, four lateral canthal rhytid patterns were identified, reflecting divergent muscle contraction patterns: (1) full-fan distribution of rhytides from the upper eyelid to the upper cheek, (2) rhytides of the lower lid / upper cheek, (3) rhytides of the upper eyelid skin down to the lateral canthus, and (4) central zone of rhytides at the lateral canthus only (Fig. 15.2). Although standard injection points can be helpful for beginner injectors, treatment should be individualized to take into account this diversity in lateral canthal rhytides, which may deviate from published patterns and require care and attention to understand, document, and address specifically. Some patients may exhibit right–left differences in the distribution and size of lateral canthal rhytides. Lateral canthal rhytides are generally classified as static, dynamic, or a combination of the two. Dynamic rhytides develop secondary to repeated muscle contractions, and remit during relaxation, and hence are most immediately amenable to treatment with botulinum toxin. Static rhytides, which are present in the absence of muscle contractions, may best be treated with soft tissue fillers or resurfacing procedures, and will be addressed later in this chapter. Alternatively, ongoing and repeated treatments with botulinum toxin may soften static rhytides over long time intervals, as reduction of coincident dynamic creases reduces the incidence of repeated microtrauma to the underlying collagen and elastin. Botulinum toxin treatments may also prevent the extension or deepening of static creases through a similar mechanism.
Preoperative assessment
Pre-existing ocular conditions such as persistent or intermittent tearing, dry eyes, or previous LASIK surgery may be associated with increased risk of dry eyes after botulinum toxin treatment. As patients may not volunteer the use of over-the-counter medications, it may be informative to question them specifically regarding the use of eye drops for dry eyes. If there is a concern that decreased tear production may exist before treatment, a Schirmer’s test can measure tear production using calibrated strips of filter paper placed within the lower eyelid, or a rose bengal test can employ a dye to detect corneal scratches associated with dry eye. Injection treatments around the eye may be modified in the context of systemic conditions with ocular manifestations, including Graves’ disease, Hashimoto’s thyroiditis, Sjögren’s syndrome, and other collagen vascular diseases. A lower eyelid ‘snap-test’ can estimate the risk for development of ectropion or scleral show after infraorbital toxin injections. The snap is assessed by pulling gently downward and outward on the lower eyelid and then quickly releasing; a rapid return to the rest position without requiring an eyelid blink suggests a fully functional orbicularis muscle and a low risk of excessive eye rounding after botulinum toxin injections (Fig. 15.3). A positive test is defined as a slow return to baseline, with the eyelid staying in a distracted position until the patient blinks, or until several seconds elapse and the lid very slowly resumes its normal apposition against the globe.
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree