Trauma
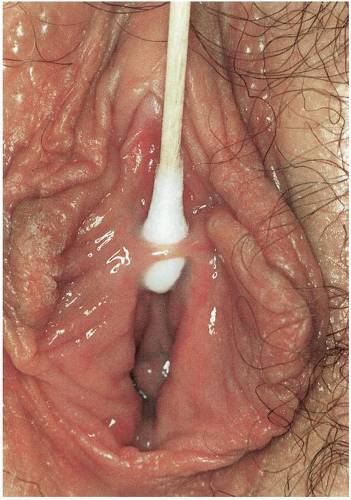
ADHESIONS (Figure 12.1.)
DEFINITION
Adhesions are bands of fibrous tissue that occur as a consequence of normal wound physiology when denuded areas of epithelium are apposed.
GENERAL FEATURES
Vulvar adhesions are rare in the adult population. They are most commonly noted to occur after a vaginal birth when vulvar lacerations are followed by apposition of denuded tissue planes. They may be seen in neonates as labial adhesions associated with inflammatory dermatoses and related to female circumcision.
CLINICAL PRESENTATION
The adult patient with vulvar adhesions may present with discomfort noted at the introitus. If the adhesions are strategically located and obstruct the normal urinary stream, spraying may be noted with micturition. Intercourse may be painful. Bands of fibrous tissue may be noted across the introitus.
MICROSCOPIC FINDINGS
Excised adhesions have microscopic features of scar with thinning of the epithelium and fibrosis of the underlying dermis with localized loss of skin appendages. Chronic inflammation may be present with recent or irritated adhesions.
ADJUNCTIVE STUDIES
No adjunctive studies are needed to evaluate the patient with vulvar adhesions, believed to be secondary to trauma of childbirth.
DIFFERENTIAL DIAGNOSIS
The diagnosis of vulvar adhesions secondary to trauma is self-evident. This condition is not to be confused with a partially perforate hymen because the bands are distal to the hymen and are primarily vestibular in location.
CLINICAL BEHAVIOR AND TREATMENT
Symptomatic adhesions may be lysed easily in the clinic. A small wheal of topical anesthetic may be injected at the base of each origin or insertion before incising and excising the adhesion. To prevent reformation it will be necessary for the patient to keep the tissue planes distinct from one another, not allowing apposition of the medial edges of the vestibule to prevent reformation of adhesions after lysis. There is no evidence to support a pharmacologic role of the estrogen in preventing adhesions.
The more likely mode of action is that daily application of the cream mechanically prevents apposition of tissue planes and allows healing to occur.
The more likely mode of action is that daily application of the cream mechanically prevents apposition of tissue planes and allows healing to occur.
PROGRESSIVE THERAPEUTIC OPTION
The progressive therapeutic option is as follows:
In the symptomatic patient, after appropriate topical anesthesia, the adhesions may be excised easily in the clinic. Excision should be followed by daily efforts on the part of the patient to keep the labia separated for varying periods of time to allow local healing without adherence of the labia or vestibule to the contralateral side. Estrogen cream may be applied topically to assist the patient in massaging the area to prevent apposition, although no pharmacologic role of the estrogen creams has been demonstrated.
ANOPERINEAL FISTULA (Figure 12.2.)
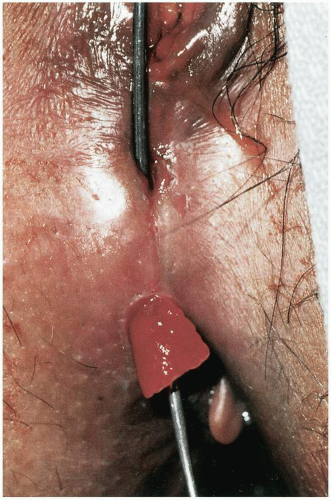 Figure 12.2. Postobstetric anoperineal fistula. Note exuberant granulation tissue. Sound demonstrates fistula tract. Tract was excised and closed primarily without recurrence. |
DEFINITION
An anoperineal fistula is a communication between the anus and the perineal body.
GENERAL FEATURES
A fistula involving the perineum or vestibule and communicating with the anus or rectum is almost invariably a consequence of a postobstetric event. Vaginal delivery may result in laceration of the anal sphincter and anal rectal mucosa. Although this is repaired, dehiscence of the repair will result in a fistula tract.
CLINICAL PRESENTATION
The patient will present complaining of feculent material passing through the perineum or vestibule. If the anal sphincter has been disrupted, fecal incontinence may be a significant symptom.
DIFFERENTIAL DIAGNOSIS
As noted, the differential diagnosis would include inflammatory bowel disease, which should be suspected in patients with appropriate symptoms or findings (friable anal and rectal mucosa). The appearance of a fistula in a patient who has not experienced a vaginal delivery should raise the suspicion of inflammatory bowel disease, lymphogranuloma venereum, and carcinoma. Fistulas observed with lymphogranuloma venereum are often multiple and are associated with edema of the external genitalia, resulting in the anogenital syndrome. Appropriate serologic studies for the precipitating chlamydial organisms should be obtained. If carcinoma is suspected, appropriate biopsies should be obtained.
MICROSCOPIC FEATURES
Fistulous tracts that communicate from the anal or bowel mucosa to the vulvar skin, vestibule, or vagina are often lined, in part, by squamous epithelium from the exterior epithelium. A marked acute and chronic inflammatory infiltrate is present in the tissue immediately adjacent to the fistula. In some cases, foreign body giant cells and polarized foreign material may be found
in the tract. On occasion, suture material or other foreign material may be within the tract or embedded in the tract wall.
in the tract. On occasion, suture material or other foreign material may be within the tract or embedded in the tract wall.
CLINICAL BEHAVIOR AND TREATMENT
Rarely, a minute fistula resulting from obstetric trauma may heal spontaneously. Usually, surgical repair will be necessary. This repair should be accomplished as soon as the incision is free of evidence of infection. Often the anal sphincter will be involved in the fistulous tract and it will be necessary to reapproximate the anal sphincter as well as the rectal walls. The fistula tract may be defined with a lacrimal problem or may be delineated with methylene blue injected into the tract before incision. The excision and repair should be accomplished in the operating room under appropriate anesthesia. A preoperative bowel preparation with GoLYTELY or colonic enemas should be accomplished. Broad-spectrum antibiotics should be administered before surgery to decrease colony counts within the surgical incision. The tract should be excised, and the rectal wall should be approximated with interrupted 3-0 polyglactin 910 or similar absorbable suture. A reinforcing second layer of 2-0 polyglactin 910 should be placed securely in the muscularis of the bowel wall in an interrupted fashion. The anal sphincter may be approximated with three or four interrupted stitches of 0 absorbable suture material that include muscle and capsule in the repair. With cephalic extension of the fistula, consideration should be given to approximating the levator ani muscles to reinforce the surgical repair and to augment the perineum. Perineal and vestibular skin may be approximated with running subcuticular 3-0 absorbable suture material. Postoperatively the patient may be managed as an outpatient with 7 to 10 days of an elemental diet, stool softeners, and sitz baths. The patient may benefit in the first 24 hours from an ice pack. Pain is usually controlled with oral analgesics.
PROGRESSIVE THERAPEUTIC OPTION
The progressive therapeutic option is as follows:
Excision and multilayer closure under broad-spectrum prophylactic agents and broad-spectrum antibiotics after appropriate bowel preparation with GoLYTELY or high-colonic enemas.
BULLET WOUND (Figure 12.3.)
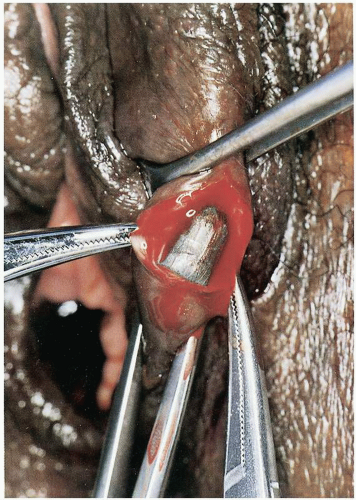 Figure 12.3. A .22-caliber projectile lodged in left labium majus after entering suprapubic region and transversing the space of Retzius without injuring the bladder or urethra. |
DEFINITION
A bullet wound is a consequence of penetration of vulvar tissue planes by a metal projectile delivered by an explosive charge.
GENERAL FEATURES
With the increasing prevalence of weapons in the population and accelerating levels of violence, bullet injuries to the female genitalia may be expected to increase in frequency.
CLINICAL PRESENTATION
Depending on the caliber of the weapon used and the trajectory of the projectile, vulvar findings may be minimal or massive. A small-caliber, handheld weapon fired tangentially into the lower abdomen may result in a trajectory that terminates in the vulva, with minimal vulvar damage. Conversely, a large-gauge, pelletcontaining weapon applied to the vulva before discharge will create massive, life-threatening injury.
ADJUNCTIVE STUDIES
Depending on the entry site and severity of damage, endoscopic studies of the bladder, urethra, and bowel and direct visualization of the peritoneal cavity to rule out visceral damage may be necessary.
MICROSCOPIC FINDINGS
There is a considerable body of forensic pathology literature describing and defining entry and exit bullet wounds, and the distinction is often of critical importance in criminal investigators. Entry wounds, if occurring in close proximity to the weapon, usually will show evidence of gun powder and bullet or clothing fragments embedded about the entry site. Small tears running parallel to the axis of the wound may be evident. The entry site often appears to have a relatively smooth margin appearing as a punched-out hole.
A bullet exit site may be highly variable, depending on the velocity and type of the bullet and whether or not the skin of the exit site was supported (i.e., against a fixed surface) or free. In general, the higher the velocity of the bullet, the larger and more disrupted the exit site. The edges of the wound may appear serrated and torn, giving the wound a stellate appearance.
CLINICAL BEHAVIOR AND TREATMENT
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree