Transposition Flaps
Introduction
Transposition flaps can be designed in a number of different configurations; however, their linear dimension is always longer than their width. Common configurations of transposition flaps are listed in Table 8-1. The majority of facial cutaneous defects are repaired with transposition flaps designed as a rectangle, parabola, or rhombus. A rhombic flap and its modifications are transferred to the recipient site by advancement as well as by pivoting. However, I discuss them here because their major method of movement is pivotal, and like pure pivotal flaps, they develop a single standing cutaneous deformity at their base. Z-plasty and bilobe flaps represent the use of two transposition flaps concomitantly. In the case of Z-plasty, diagonally opposing triangle-shaped flaps trade locations after transposition. A bilobe flap represents two transposition flaps designed on a common base. However, each lobe has an independent pivotal point, and each lobe develops an independent standing cutaneous deformity.
Because transposition flaps are pivotal flaps, the greater the arc of pivotal movement, the greater will be the size of the standing cutaneous deformity and the less will be the effective length of the flap. Pivoting a transposition flap 45° from its in situ position reduces the effective length 5%. A 90° and 180° pivot reduces length by 15% and 40%, respectively (see discussion in Chapter 6).1 The reduction in effective length must be accounted for when transposition flaps are designed, so that greater pivoting requires a longer design of the flap. The most common error in using transposition flaps of any kind is to design the flap too short because of a poor understanding of this concept. As transposition flaps turn in an arc around their relatively fixed pivotal point, a standing cutaneous deformity forms. Similar to the relationship between the arc of flap movement and effective length, there is a direct and positive association between the degree of pivoting and the size of the standing cutaneous deformity. The greater the pivot of the flap, the larger is the deformity that develops from the pivotal movement. Thus, increasing the flap’s pivot will shorten the effective length, increase wound closure tension (if it is not designed sufficiently long), and change the flap’s shape as a result of forming a standing cutaneous deformity. To limit these restricting factors, whenever possible, transposition flaps should be designed not to pivot more than 90°.
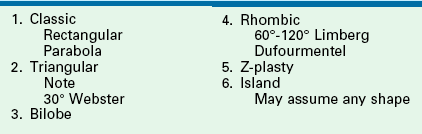
In the majority of cases, standing cutaneous deformities resulting from transposing flaps can be resected at the time of the initial flap transfer to the recipient site. Excision should always be in a vector that diverges from the base of the flap so vascularity is not unduly impaired (Fig. 8-1). For scalp and large transposition flaps of the face, it may be prudent to delay excision of the deformity for 4 to 6 weeks to allow revascularization of the distal flap.
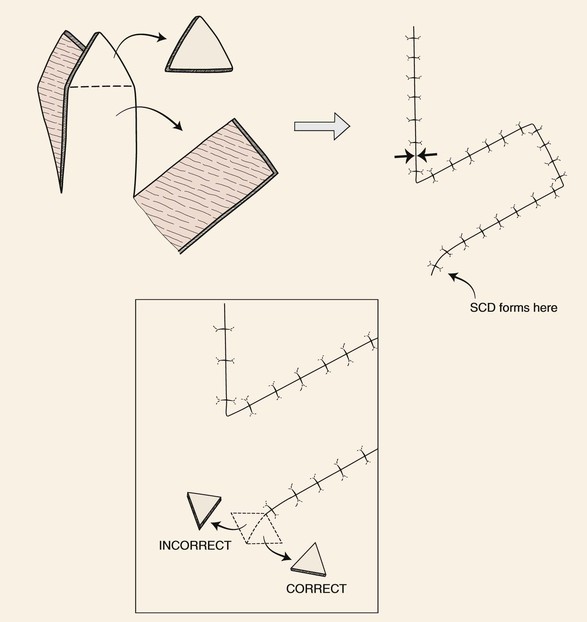
FIGURE 8-1 Transposition flaps are pivotal flaps that form single standing cutaneous deformities (SCD) at base of flap. Only base of flap must be contiguous with defect. Excision of SCD should always be in vector that diverges from base of flap to minimize impairment of blood supply. Opposing arrows indicate area of greatest wound closure tension.
A disadvantage of transposition flaps is the potential for development of a trap-door deformity.2,3 The deformity is present when the flap appears bulky, protruding above the surface of the surrounding skin and giving the appearance of a pincushion. This complication tends to occur a few weeks after transfer. Trap-door deformity occurs most often when curvilinear incisions are made at the distal border of flaps. Concentric contraction of the resulting scar presumably causes the curvilinear arc of the scar to contract toward its center, which in turn forces the skin to protrude outward above the surface of the surrounding skin. Creating straight rather than curved incisions and designing the distal border of the flap with an angle instead of an arc prevents curvilinear scars. Trap-door deformity may also develop because adjacent tissue surrounding the recipient site is not sufficiently undermined at the time of transposition. The sheet of scar that forms between the undersurface of the flap and the depth of the defect contracts in a concentric fashion. Contraction of the scar beneath the flap causes the flap to bulge outward. Fortunately, trap-door deformity usually resolves with time. Trap-door deformities can be minimized or prevented by wide subdermal undermining of the margins of the primary defect and using a flap with the same thickness as the depth of the recipient site. For defects located in skin with sebaceous gland hypertrophy, it is helpful to maintain the bevel of the defect resulting from micrographic surgery or to create one and counterbevel the edge of the flap. This creates a diagonally sloping scar beneath the epidermis that may reduce concentric scar contraction. As noted, concentric scars are a common cause of trap-door deformity.
Applications
Classic Design
The rectangle- or parabola-shaped transposition flap is commonly used for repair of cutaneous defects of the medial and lateral cheek, temple, and glabellar area (Fig. 8-2). A linear closure of cutaneous defects of the temple often results in elevation of the lateral brow or webbing of the lateral canthus. The use of transposition flaps frequently can avoid these problems. Small flaps of this design can also be used to repair defects of the dorsum and sidewall of the nose, chin, and upper and lower lips. Transfer of skin or of skin and muscle from the upper to the lower eyelid to repair anterior lamellar defects may readily be accomplished by using either medially or laterally based cutaneous or musculocutaneous (containing orbicularis muscle) transposition flaps.
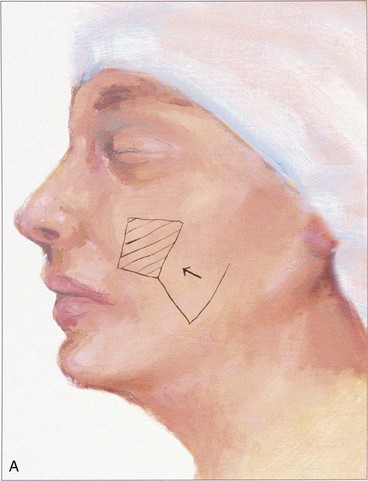
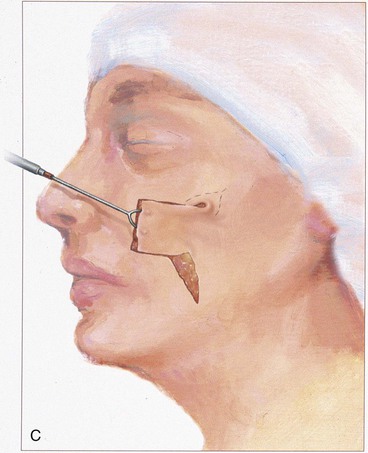
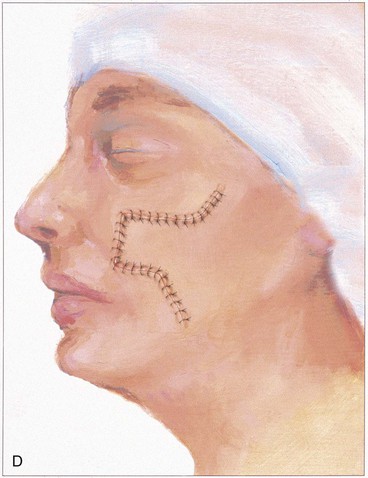
FIGURE 8-2 A-D, Rectangle-shaped transposition flaps most frequently used for repair of cutaneous defects of medial and lateral cheek.
Island Transposition Flaps
Most transposition flaps used on the face have a cutaneous pedicle and a random blood supply. However, island transposition flaps based on an axial blood supply can be harvested from the region of the forehead and medial cheek. In the forehead, the flap is transferred with the supratrochlear artery and vein. Such flaps have limited use for facial reconstruction but can be used to repair defects located on the upper nasal dorsum or medial canthus. Park and colleagues have shown that the superior labial artery gives rise to an artery to the nasal septum that divides into a superficial and deep branch and a second independent artery to the nasal ala.4 The deep division of the septal artery can be used to nourish a sizeable mucosal island axial transposition flap harvested from the inner aspect of the upper lip. This flap can be used to reconstruct large defects of the vermilion. Similarly, a sizeable island transposition flap harvested with the skin and subcutaneous tissue of the upper melolabial fold can be transferred as an axial flap based on the alar artery, which arises from the facial artery just before the vessel gives rise to the superior labial artery. Common examples of island transposition flaps used in the head and scalp are flaps from the forehead transferred to the upper nose, temporal hair-bearing scalp flaps transferred to the anterior scalp to treat male pattern baldness, and palatal mucoperiosteal flaps transferred to the nasal surface of the velum.
Note Flap
The note flap described by Walike and Larrabee is an angular transposition flap that, when designed, looks like a musical eighth note.5 This flap allows one to close a circular defect with a triangular transposition flap that maximizes the use of surrounding tissue (Fig. 8-3).6 The flap is designed by first drawing a tangent on either side of the circle parallel to relaxed skin tension lines (RSTLs). The tangent should have the length of 1.5 times the diameter of the circular defect. At the end of the tangent line, a 50° to 60° angled flap is designed, with the second side of the flap having a length approximately equal to the diameter of the circle.6 The flap is transposed into the defect, and the distal tip of the flap is trimmed so that there is no wound closure tension. As with rectangular and parabolic transposition flaps, the greatest wound closure tension is at the closure of the donor site. In the case of the note flap, the greatest wound closure tension is approximately perpendicular to the tangent line created when the flap is designed. The surface area of the note flap is designed so that it is 25% less than the area of the defect; thus clinical judgment is required when this flap is used. The flap is recommended primarily for small (2 cm or less) skin defects. Because the pivotal arc of the note flap is approximately 45°, a minimal standing cutaneous deformity develops that may not require excision. Standing cutaneous deformities of larger flaps will require subsequent surgical revision unless the deformities are removed at the time of flap transfer. I use the note flap primarily for defects on the cheek, temple, and lateral nasal sidewall. However, it may be used everywhere on the head and neck, including the lip.
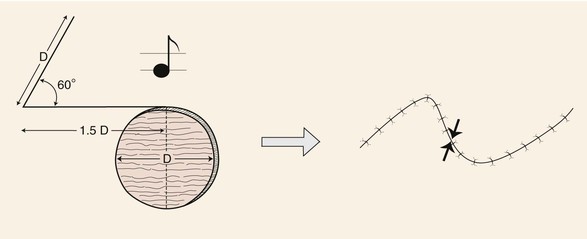
FIGURE 8-3 Note flap has configuration of musical eighth note. The note flap is used for repair of circular skin defects 2 cm or less in size. One side of flap drawn parallel to relaxed skin tension lines and tangent to defect has length of 1.5 times diameter (D) of defect. Second side of triangle-shaped flap forms 50° to 60° angle with first side and is length of diameter of defect. Point of greatest wound closure tension is indicated by opposing arrows.
Rhombic Flap
The rhombic flap is a common flap used by plastic surgeons. The flap is discussed in great detail in Chapter 11. Transfer of the flap involves advancement and pivotal tissue movement. A rhombus can be considered a square usually tilted toward one side. The greater the tilt of the rhombus, the greater is the discrepancy in length between the short and long diagonals of the rhombus. A rhombus may have right angles, in which case it is also a square; however, in addressing rhombic flaps, the rhombus-shaped defect is usually not square in configuration, so opposing interior angles are obtuse or acute. The classic rhombic flap described by Limberg is used to repair a defect that has a configuration of a rhombus with two opposing 60° and two opposing 120° interior angles (Fig. 8-4).7 The 60° to 120° rhombus can be thought of as two equilateral triangles placed base to base. This means the short diagonal of the rhombus is equal in length to the sides of the rhombus. The Limberg flap is designed to repair a defect of this configuration. The flap is designed by extending the line of the short diagonal a length equal to the diagonal, which is also the length of the side of the defect. This creates the first side of the flap. A second line is then drawn of equal length parallel to either adjacent side of the defect. Because there are two sides adjacent to the extended diagonal, two flaps can be designed. In addition, because the short diagonal can be extended in two directions from the rhombic defect, a total of four flaps can be designed around a rhombus-shaped defect. The majority of wound closure tension is at the donor site and has been calculated to be 20° to the short diagonal of the rhombus defect (see Fig. 8-4).8 Skin mobility and extensibility are important to consider in designing a rhombic flap, and an understanding of the resultant wound closure tension vector is critical to avoid distortion of surrounding facial structures.
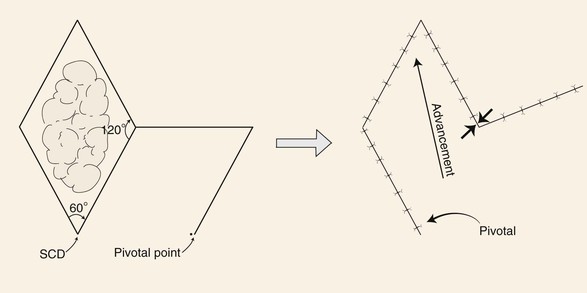
FIGURE 8-4 Limberg flap used for repair of skin defects that have configurations of a rhombus with two opposing 60° and two opposing 120° interior angles. Flap designed by extending line of short diagonal equal to diagonal length. Second line drawn of equal length parallel to either adjacent side of defect. Point of greatest wound closure tension is indicated by opposing arrows. Standing cutaneous deformity (SCD) forms at base of flap.
There are a number of variations in the design of rhombic flaps. A useful variation is a 30° rhombic flap. An M-plasty may be combined with transposition of the flap.9 The 30° rhombic flap has the advantage of minimizing the standing cutaneous deformity because there is less pivotal movement than with the classic Limberg flap. When it is used, the M-plasty reduces the length of excision necessary to remove the standing cutaneous deformity. The 30° rhombic flap can be designed by approximately halving an equilateral triangle.6 The length of the side of the triangle should be the length of a side of the defect (Fig. 8-5). The angle of the apex of the transposition flap is 30°. The width of the base of the flap is half the greatest width of the defect (see Fig. 8-5).6
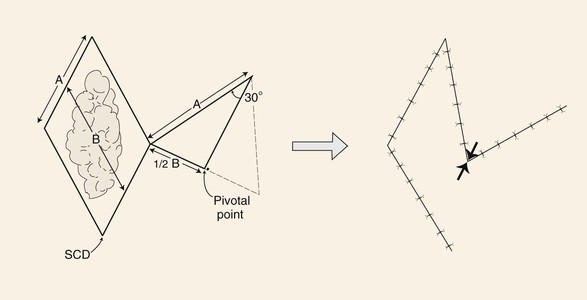
FIGURE 8-5 A 30° rhombic transposition flap designed by approximately halving an equilateral triangle. Length of triangle side is length of side of defect (A). Angle formed at apex of triangle-shaped flap is 30°. Width of flap is half widest width of defect (B). Point of greatest wound closure tension is indicated by opposing arrows. Standing cutaneous deformity (SCD) forms at base of flap.
The Dufourmentel modification of the rhombic flap can be used for rhombus-shaped defects that have any combination of interior angles, not just those of 60° to 120°. It is particularly useful for repair of rhombic defects with acute angles of 60° to 90° when the surgeon does not wish to excise additional tissue to create a 60° to 120° rhombus.6 The flap is designed first by bisecting the angle between the extension of the short diagonal and one of the sides of the defect (Fig. 8-6). The bisecting line is extended a length equal to the length of a side of the defect. This creates the first side of the flap. A second line of the same length is drawn parallel to the long diagonal of the rhombus defect. This creates the second side of the flap that is not parallel to the side of the defect, as with the Limberg flap. Like in other transposition flaps designed to close rhombus-shaped defects, the greatest wound closure tension is at the closure site of the donor defect. Therefore, whenever possible, the donor site closure should be planned so that it is parallel to the lines of maximum extensibility (LME) and perpendicular to RSTLs.
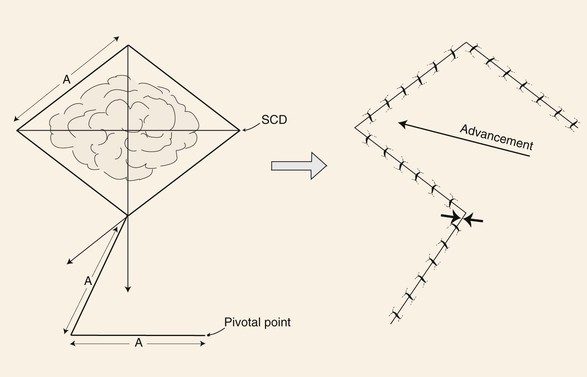
FIGURE 8-6 Dufourmentel flap designed by bisecting angle between extension of short diagonal and one side of defect. Length of bisecting line extended length of side of defect (A). Line of same length creating second side of flap drawn parallel to long diagonal of rhombic defect. Point of greatest wound closure tension is indicated by opposing arrows. Standing cutaneous deformity (SCD) forms at base of flap.
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree