11
Transconjunctival Subperiosteal Cheek Lift with and without Malar Augmentation
Cosmetic and reconstructive subperiosteal cheek lifting has become more popular and controversial over the past few years. Although it can be performed through several approaches, this chapter will describe the technique that I prefer—the transconjunctival blepharoplasty approach as described by Putterman,1 with several modifications. One of these modifications is the augmentation of either or both the inferior orbital rim and the malar soft tissue with the aid of standard prefabricated porous polyethylene implants. Augmentation just below the inferior orbital rim has several benefits. In cases of previous maxillectomy with loss of the inferior rim it can restore the support structures and cosmetic contour of the entire midface. Soft tissue and periosteum can be directly fixated to the implant itself. In cases of bony or soft tissue hypoplasia (i.e., iatrogenic lid retraction, exophthalmos, pseudoexophthalmos from a hypoplastic inferior orbital rim, congenital euryblepharon, childhood radiation therapy, etc.) the implant can be fashioned to maximize volume directly where it is needed. In cases of focal lid or cheek anomalies, the periosteal flap can be directed where it is needed and easily fixated to the implant for greater support.
A second modification (or series of modifications) deals with lateral bunching of redundant soft tissue. One of the most common criticisms of the technique from patients and surgeons is bunching and dimpling of tissue in the lateral lower lid and lateral canthal area. This seems particularly prevalent in faces with significant subcutaneous fat or those requiring excessive lift. Although patients commonly complain about this it generally resolves in 6 to 12 weeks. Despite this fact, simple attention to detail during closure can greatly diminish this problem.
 Background and History
Background and History
Various techniques for safe and efficacious midfacial rejuvenation or augmentation are continually argued in the literature. Hester et al were instrumental in advancing the subperiosteal midface lift among oculoplastic and facial plastic surgeons.2 However, Ramirez et al were probably among the first to describe a subperiosteal approach to midfacial rejuvenation performed in combination with cervicofacial rejuvenation.3 When malar augmentation is performed in conjunction with other facial techniques, we perform a cheek lift as a separate procedure rather than performing extended dissections through endoscopic brow and cervicofacial dissections.
In 1989 Binder described a “new” technique of mid-facial rejuvenation using a silastic implant to augment malar tissues during facial rejuvenation.4 Following this, Mladick subclassified variations in malar hypoplasia and described two implants that could be placed in different “pockets” during various facial surgical procedures.5 These implants included Silastic and Proplast implants and were reported associated with minimal complications. I prefer the use of preformed porous implants directly fixated in the subperiosteal pocket. The porous implants integrate well and are easily contoured for specific needs. If one desires, a variety of porous polyethylene malar implants are also available. Both types of implants (malar and inferior orbital rim) augment a hollow midface. In my experience the majority of patients with malar hypoplasia require elevation and augmentation to minimize the nasojugal trough and midface.
Although McCord emphasized the importance of incorporating lid-tightening procedures to prevent postoperative ectropion,6 authors have also described techniques with minimal complications without lid tightening.3,7,8 The technique that will be described here includes lid tightening. The dramatic amount of tissue that is brought into the lower lid by this technique can have a profound effect on stabilizing vectors in the lower lid. The addition of a malar implant increases the effects on these vectors. I advocate a lateral tarsal strip procedure in each case for several reasons. It affords complete control of the shape of the palpebral fissure, prevents the occasional ectropion due to undiagnosed laxity, and allows direct access to the orbicularis muscle, suborbicularis oculi fat (SOOF), and periosteum for flap elevation and manipulation (Figs. 11-1; 11-2).
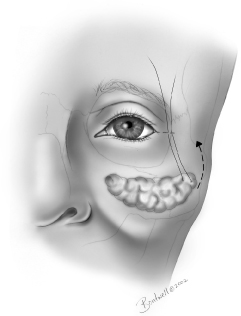
Figure 11-1 Illustration of canthotomy, descended or ptotic suborbicularis oculi fat, and principle of suture fixation of SOOF.
 Patient Selection and Indications
Patient Selection and Indications
Transconjunctival subperiosteal cheek lifting has many functional and aesthetic indications. It probably affords the safest and most effective access to mobilize the entire midfacial unit. Reliance on periosteal refixation to support the soft tissues provides long-lasting and effective effacement of midfacial folds, deficits, and lid retractions. In patients with mild malar hypoplasia a simple cheek lift can bring fullness to a hollow-appearing infraorbital area, simulating a small implant. In cases where there is a more substantial volume deficit, augmentation can be achieved by subperiosteal placement of an implant. The indications listed here are for standard subperiosteal cheek lifting. Each one of these cases can be further augmented with a malar implant if desired. In addition to these primary indications, this technique can be combined with other facial rejuvenation procedures including cervicofacial rhytidectomy, endoscopic brow lifting, and upper lid blepharoplasty.
 Common Indications for Midface Lifting
Common Indications for Midface Lifting
- Cicatricial ectropion
- Lower eyelid retraction (from lack of anterior lamellae)
- Hollowness of lower eyelid and/or cheek (congenital or postsurgical)
- Deep nasojugal trough
- Prominent nasolabial fold
- Malar festoons
- Midfacial and lower eyelid deficit
- Facial palsy (with or without facial rhytidectomy)
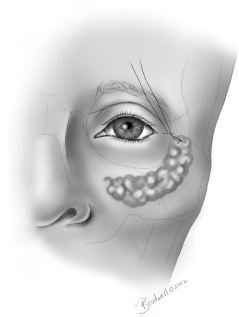
Figure 11-2 Conceptual illustration of relationship of lifted suborbicularis oculi fat and periosteum performed through standard lateral canthotomy incision with fixation to lateral periosteum or temporalis fascia.
 Surgical Technique
Surgical Technique
Patient Preparation and Local Anesthetic
This technique can be performed under general anesthesia or local anesthesia with sedation. The patient is laid supine on the table and the entire face is prepped with 10% Betadine solution. Betadine soap is avoided and 10% solution is kept out of the eye to avoid chemical irritation of the conjunctiva and cornea. I prep the nasal cannula or endotracheal tube to the level of the chin (if there will be other procedures performed, the prep is done as indicated for those procedures). The top of the head and forehead are also draped according to surgeon preference and additional procedures. I place a split bodysheet below the chin and out around the ear, which allows draping without any tension on the cheek or lateral periorbital tissue. This is particularly important if the patient is placed in a sitting position intraoperatively to judge symmetry.
Protective scleral shells are placed for comfort and protection, after instilling a topical anesthetic drop for patients not under general anesthesia. A normal-length (∼1 cm) lateral canthal incision is drawn out. It is unnecessary to make an extended incision. The eyelids are infiltrated with a mixture of 0.5% lidocaine with 1:200,000 epinephrine (40 mL) and 0.5% bupivacaine (4 mL) in the lateral canthus, lateral one third of the upper lid, and anterior lower lid lamellae, and transconjunctivally into the fat pads. The infraorbital nerve foramen is palpated and marked. If it cannot be palpated secondary to excess malar fat, the foramen is located by making a plumb line directly inferior from the supraorbital notch to the superior fold of the external ala of the nose. Once marked, the infraorbital nerve and the cheeks are infiltrated with the dilute mixture down to the nasolabial fold and the superior gum line.
Transconjunctival Approach
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree



