div class=”ChapterContextInformation”>
3. Strategies to Improve Adherence
Keywords
NonadherenceHealthcare providerPatientStrategyTechniquesIntroduction
A good patient-physician relationship is integral to optimizing adherence to treatment and clinical outcomes. However, the concept of the patient-physician relationship has been evolving in recent years. Previously, an asymmetric relationship between the physician and the patient was assumed – the physician knows best about the disease and treatment, the patient accepts this and follows instructions. In this model, the term compliance described the patient’s consent to follow medical recommendation. Compliance implies that the physician instructs and the patient is to follow those instructions. Recently, the patient-physician relationship has become viewed as a more collaborative process, one which the patient is more involved in the decision process. For this reason, the term adherence has replaced compliance and the even newer term concordance has been proposed [1]. Concordance more clearly implies a shared responsibility between the physician and patient to agree on medical recommendations.
The realization has also arisen that adherence does not rest alone with the patient. Other factors—such as the physician, the diagnosis, and the medication— may influence the patient’s adherence behavior. Patients may accept or reject the medical advice, especially depending on the relationship they have with their physician. A growing body of literature supports the positive effect of agreement within the patient-physician relationship on adherence and patient outcomes [2]. Other studies demonstrate that disagreements between patients and physicians lead to poor adherence and health outcomes [3, 4]. For this reason, it may be helpful to understand how physicians can influence agreement, and ultimately patients’ adherence to treatment.
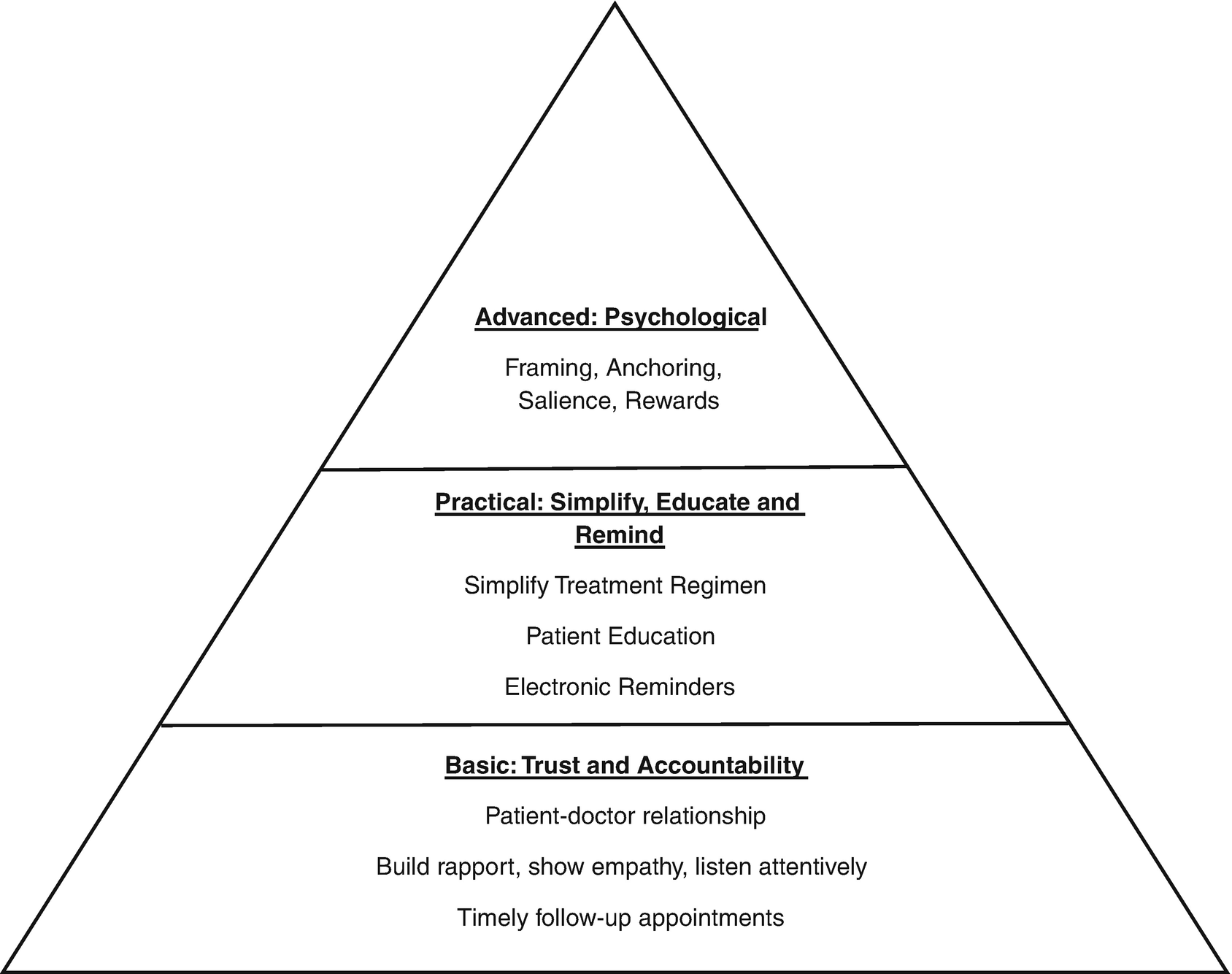
There are many aspects of the patient-physician relationship for which physicians have some degree of direct control. These include continuity of care, patients’ trust in their physician, and the ability of the physician to enable the patient toward effective self-management. Physicians build trust by creating a supportive and friendly environment that eases patients’ distress. By educating patients on the disease and treatment plan, physicians increase patient confidence patients have in their physician, in their treatment regimen, and in their own self-management. In addition to building trust in the physician and confidence with simple interventions, physicians may employ more advanced strategies to develop agreement with the patient on the recommended treatment plan. This chapter will examine interventions ranging from basic interventions to more complex techniques to improve patient adherence.
Physician-Centered Strategies
Physician-centered strategies
Foundation: Trust and Accountability
An important step to improving adherence is building a foundation that increases trust and accountability. Trust develops over time as physicians build rapport with patients, create a friendly, supportive environment, and appear understanding to patients’ situations and concerns. Being perceived as a caring physician is central to building this trust. A physician’s interpersonal skills such as showing empathy, listening attentively and clear communication are important in fostering trust, allowing patients to reveal any barriers affecting their ability to take their medications [5]. Studies on the doctor-patient relationship focus on how these interpersonal skills rather than time spent can lead to increased satisfaction of care [6, 7]. Increased patient satisfaction with the doctor-patient relationship improves treatment adherence [8]. In pediatric atopic dermatitis (AD), the strongest predictor of adherence to skincare advice is a solid doctor-patient or caregiver relationship. This results in greater self-efficacy as mothers feel more comfortable managing their children’s disease [9]. For psoriasis patients using biologics, patient-physician communication and good interpersonal relations were drivers for greater adherence [10].
Another important component at this level is improving accountability by scheduling an early follow up visit or other contact with the patient. Early and frequent follow-up visits increases the likelihood of patients taking their medication in anticipation of those visits with the physician [11, 12]. An analysis of 5 studies on AD patients and adherence revealed that the length of time between baseline and first return visit was inversely proportional to adherence [13].
Practical: Simplify, Educate, and Remind
After establishing a foundation, the next level of physician-centered strategies involves simple, effective interventions that physicians can implement to help patients manage their conditions better. This includes simplifying treatment regimens, patient education, medication reminders, and medication cost.
Simplified Treatment Regimens and Patient Preference
Overly complicated treatment regimens are common impediments to poor adherence. Although multiple treatments might be effective in improving outcomes if they were all used, the complexity of such regimens increase treatment burden, may reduce adherence, and, potentially, worsen treatment outcomes. When multiple treatments are needed, simplifying the treatment regimens by prescribing a combination product with multiple active ingredients may be a worthwhile intervention. A clinical trial randomized 26 subjects with mild-to-moderate acne to clindamycin phosphate 1.2%-tretinoin 0.025% (CTG) gel or clindamycin phosphate 1% gel plus tretinoin 0.025% cream (C gel + T cream) for 12 weeks. At week 12, the median adherence of the combination group was higher than for the group that received C gel + T cream separately (86% vs 14%, P = 0.02) [14].
Patients may prefer one treatment over another, the vehicle type of a medication, or a certain dosing schedule that is convenient for them. Messy application is a common reason for nonadherence so patients may prefer less greasy topical corticosteroid vehicles such as foams or sprays [15]. About 69% of patients using biologics preferred a less frequent dosing schedule limited to once every 12 weeks as opposed to 1-week or 2-week dosing schedules [16]. It is important for physicians to listen to these patient preferences and adjust care because patients feel more empowered when they help develop the treatment plan and thus are more likely to adhere to it [17].
Patient Education
Educating patients is a simple intervention that can be done during the clinic office visit, sometimes with the aid of technology or through formalized workshops. The impact of education on adherence can be considerable as patients learn more about the disease and treatments and may influence patients’ perceptions of treatment efficacy and necessity. Educating patients during the office visit is effective as patients respond better when they receive individualized advice and learn how to incorporate management into everyday lives [18]. However, this may be more time consuming and results in less recall by patients if the information is presented verbally with no other educational aids [19, 20].
Written information in the form of written action plans, pamphlets, and office posters are useful tools to aid in relaying vital information to patients. Providing written information can also save time and be cost effective. Lists are more effective than paragraphs [21, 22]. Written information along with verbal instructions can help with recall [23]. Individualized printed materials tailored to patient’s demographics and stage of disease are more likely to be read than general information about the disease [24]. A multidisciplinary, informative brochure plus a personalized patient notebook can teach patients on how to manage their disease and result in improved quality of life and severity of disease [25].
The use of audiotapes, videotapes, computer-assisted patient education can assist physicians in teaching patients. These modes of information are more interactive and may help reduce the amount of time physicians have to spend educating and addressing patient concerns and questions. In addition, the use of the internet in educating patients may be effective if patients are directed to the right resources. For example, the Contact Allergen Replacement Database is a fabulous resource that allows dermatologists to input allergens and develop lists of products free of those allergens and saves time patients searching for the appropriate products [14]. The National Psoriasis Foundation offers a host of brochures on treatment options that can be used to educate patients on the risks, benefits and alternatives of commonly used systemic treatments for psoriasis.
Regardless of the mode of education, educating can have a substantial impact on helping patients manage their disease and improve adherence. A multicenter, clinical trial randomized 97 subjects with acne to either adapalene/benzoyl peroxide (A/BPO) + supplementary education material (SEM), A/BPO + 2 additional visits or A/BPO alone. A/BPO + SEM group had more subjects with greater than 75% adherence compared to A/BPO+ 2 additional visits and A/BPO alone groups (45% vs 30.4% vs 25%), although mean adherence was still less than 50% in all groups [26]. The impact of oral and written counseling on treatment adherence in acne patients was assessed by randomizing 80 subjects to receive either a patient information leaflet plus oral instruction via telephone or oral counseling during the clinic visit only. There was a higher self-reported adherence in the group that received oral and written instruction compared to group with standard office visit instructions (80% vs 62%, P = 0.043) [27].
Medication Reminders
Timely reminders can be another simple intervention physicians can utilize in helping improve adherence. Text message reminders are a novel way to improve adherence and convenient for patients to use. Daily text message reminders were sent to 20 patients with psoriasis for 12 weeks. Adherence was measured by investigating how many days per week patients correctly took their medication. At Week 12, the daily text message intervention group had a 67.4% increase in adherence from baseline (adherence improved from 3.86 days/week to 6.46 days/week; P < 0.001) [28]. Another way to incorporate reminders is to use a smartphone app that has built in reminders that pop up on screen. A clinical trial randomized 134 psoriasis subjects treated with once-daily calcipotriol/betamethasone dipropionate (Cal/BD) foam to receive either a smartphone app reminder or standard care. Subjects who used the app were much more adherent to Cal/BD foam than were subjects in the control group (65% vs 38%, P = 0.004) at Week 4 [29].
Cost
Unaffordable drug prices may negatively impact adherence. Healthcare providers can prescribe low-cost generic medications to help reduce the burden of treatment. Furthermore, providers may also communicate with pharmacies to choose the best cost-effective treatment for the patient. Although brand name medications are generally more expensive then generic, some generic medications may also be expensive. Therefore, choosing the most cost-effective medication in a collaborative approach between the healthcare provider, patient, and pharmacy, could avoid a detrimental impact on the patient economically [30].
Advanced: Psychological Techniques
Physicians may employ a variety of psychological techniques including framing, anchoring, salience and rewards when discussing potential treatment recommendations with patients to increase the likelihood that patients will adhere.
Framing
Framing the information patients receive may influence their perspective on the treatment. Framing is a type of cognitive bias in which people react to a particular choice in different ways depending on how it is presented. Many times, patients may fear the adverse effects (AEs) of a given medication, and framing the information about AEs can help lessen those fears. For example, if a medication has a 1/1000 chance of causing AEs, a physician could frame this piece of information by saying that 999/1000 people using the medication do not experience AEs. Patients fine the latter framing—999 out of 1000 not having an AE—more reassuring even though the two approaches are mathematically identical ways of presenting the information. One study analyzed the different ways in which information on actinic keratosis (AK) was presented and how that influenced whether patients sought treatment. Of the patients who were told AKs were precancerous, 92.2% preferred treatment [31]. Of patients who were told AKs do not progress to cancer, 57.7% chose treatment [31].
Another way to reduce the negative effects of AEs on adherence is to explain to patients that AEs are signs that a medication is working. Some patients might stop the medication if they experience pain or burning after applying a topical agent. If patients are told beforehand that these AEs are indicators that a medication is working (and arguably such side effects are a sign the medication is working because these side effects indicate the patient is effectively applying the medication), patients may be more likely to continue with the medication instead of prematurely stop it. Framing the same information in a different way is a powerful tool to change a patient’s perspective and influence their decision on treatment.
Anchoring
Anchoring can reduce the perceived burden of treatment. Anchoring occurs when people make a judgment relative to the first piece of information. For example, if patients are presented a complex, difficult dosing regimen first, they may find a standard regimen more appealing. In the treatment of psoriasis patients who’ve never before taken by injection but who need a biologic, it may be helpful to explain that, “biologics have to be taken like insulin: by injection. You know how diabetics have to take insulin injections twice a day? Well, this medication is a lot like that, only you don’t have to take it twice a day, you only need to take it once a month.” If patients are simply offered once a month injections, they mentally compare taking a shot once a month to not taking shots, and it doesn’t seem very appealing. On the other hand, if patients are first anchored on the idea of shots twice a day, the 1 month frequency of injection seems very tolerable. One study measured this anchoring technique with biologics, and patients anchored to once-daily injectable biologic intervention were more willing (on a scale of 1–10) to start a once-monthly injectable biologic (median, 7.5) than those not anchored to a once-daily injection first (median, 2.0, P < 0.001) [32]. Anchoring can dramatically change the perception of treatment, making a standard approach seem like a bargain compared to a less appealing dosage regimen.
Salience
Salience relies on creating a vivid picture in a patient’s mind that may make patients more amendable to a treatment. Presenting quantitative statistics about the effects of a treatment may not be as attention-grabbing as creating a picture or presenting an anecdote that is more likely to stick in patients’ minds. For example, explaining that 9 out of 10 psoriasis patient clear up with a topical corticosteroid may seem promising to patients, but it may not be as powerful as creating a visual image. If a physician described how a psoriasis patient with large erythematous, scaly plaques all over their body cleared up with consistent use of a topical corticosteroid, started wearing a two-piece bathing suit, and wore a sleeveless wedding dress, patients may be more willing to try the same treatment compared to a physician who provides statistical facts about the treatment.
Reward System
A final technique that can be used is a rewards system to improve adherence. This technique draws from the psychological idea of operant condition and positive reinforcement. Adding a positive, reinforcing stimulus following a behavior will increase the chance the behavior will occur again in the future. A sticker calendar chart can be a tool for rewarding children with AD when they take their medication. A sticker is placed on each day of the calendar following a dose administration which provides positive reinforcement as well as a reminder for the next dose of medication.
Conclusion
Each of three levels of physician-centered strategies target different areas to help improve adherence. The foundation level focuses on improving the patient-doctor relationship and establishing accountability; without these, other approaches are likely not to be particularly effective. Once this foundation is established, specific approaches can be used to address the common reasons cited for nonadherence; belief in treatment inefficacy and forgetfulness may be overcome with education and medication reminders. More advanced psychological techniques— such as framing the efficacy of treatment more positively and reducing disproportionate concerns about adverse effects—are among a host of other approaches physicians can use to enhance adherence and treatment outcomes.
Conflicts of Interest
Dr. Steven Feldman has received research, speaking and/or consulting support from a variety of companies including Galderma, GSK/Stiefel, Almirall, Leo Pharma, Boehringer Ingelheim, Mylan, Celgene, Pfizer, Valeant, Abbvie, Samsung, Janssen, Lilly, Menlo, Merck, Novartis, Regeneron, Sanofi, Novan, Qurient, National Biological Corporation, Caremark, Advance Medical, Sun Pharma, Suncare Research, Informa, UpToDate and National Psoriasis Foundation. He is founder and majority owner of www.DrScore.com and founder and part owner of Causa Research, a company dedicated to enhancing patients’ adherence to treatment.
Dr. Adrian Pona, Dr. Abigail Cline, and Sree S. Kolli has no conflicts to disclose.
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree