Tissue Expansion in Forehead and Scalp Reconstruction
L. C. ARGENTA
EDITORIAL COMMENT
In the discussion following Radovan’s pioneering article (1982) (1) on tissue expansion, Grabb stated, “I predict that over the next 5 years, the technique of tissue expansion will be of equal importance to the impact of microsurgery techniques in muscle flaps. Heaven only knows the principle of skin expansion has been staring us in the face.”
The skin of the forehead and scalp differs considerably in color, texture, thickness, and hair-bearing qualities from tissue elsewhere on the body. Reconstruction of defects of this area is best accomplished with the use of similar tissue. Expansion of facial and scalp tissues is a relatively painless, well-tolerated procedure that can be accomplished over a period of several months (2).
Tissue expanders are available in multiple sizes and shapes from various manufacturers; custom prostheses can be produced if necessary. All prostheses presently available require periodic percutaneous injection of saline.
INDICATIONS
Because visits are required at 2- to 3-week intervals, skin expansion should be carried out only on reliable individuals who will conform to the required schedule and will modulate their activities appropriately during the expansion process. Expansion of facial and scalp tissues, in most cases, can be done only in well-healed injuries. Although the procedure has been used in subacute trauma, there is insufficient experience at this time to recommend this.
There is no tissue on the body that can cosmetically reproduce the qualities of the scalp. Expansion is particularly useful in individuals who have lost full-thickness hair-bearing tissue of the scalp secondary to burns or trauma.
PLANNING AND DESIGN
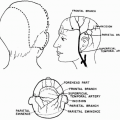
Careful planning is necessary so that the tissue to be expanded is compatible in physical nature to the area where tissue is needed. All incisions should take into account previous scars or should be at the margin of the tissue to be advanced. In the scalp, the prosthesis is placed beneath the galea.
The largest prosthesis that will fit comfortably into the pocket is selected. It must be adequate enough to develop the necessary expansion without being so large as to develop folds that may precipitate extrusion.
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree