Chapter 51 The use of skin grafts, skin flaps and tissue expansion in burn deformity reconstruction
![]() Access the complete reference list online at http://www.expertconsult.com
Access the complete reference list online at http://www.expertconsult.com
Skin grafts
The skin thickness varies depending upon the bodily locations; the eyelid skin, especially the upper eyelid, and the skin located behind the ear is thin, while the scalp, trunk, the palmar skin, and the sole of the foot are thick.1–3
A skin graft is classified into two types depending upon the amount of skin structures included, i.e. a piece of skin shaved to contain epidermis and various layers of dermis is said to be a split- (partial-) thickness skin graft (STSG). The graft can be harvested in different thicknesses; a thin graft is 6–8/1000th of an inch (0.15–0.20 mm) in thickness, while a graft with a thickness of 16–18/1000th of an inch (0.40–0.45 mm) is a thick split-thickness skin graft. A skin cut to contain all components of the skin, i.e. epidermis and dermis, is classified as a full-thickness skin graft (FTSG) (Fig. 51.1).4,5
Skin flaps
The techniques to fabricate various skin flaps
A random cutaneous flap
Design and fabrication of a random cutaneous flap could be made anywhere in the body surface. The shape and the form of a random skin flap can vary depending upon the treatment plan; a flap is configured according to the outline of the wound defect. A fabricated skin flap is advanced to complete wound closure. The flap mobility, however, could be restricted if the layer of underlying subcutaneous tissues is thick or fibrous. The length and the width of a random cutaneous flap are determined according to the pattern of vascular supplies to the skin; the ratio of flap length and the width is limited to 2 : 1. Necrosis of the skin at the end is common for a long and narrow skin flap (Fig. 51.2).6–8
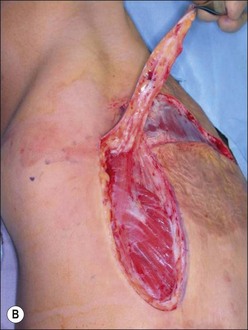
An axial or an arterialized skin flap
As shown, a nasolabial flap can be fabricated with a length versus width ratio in excess of 2 : 1; this is a skin flap formed along the side of nose. The Bakamjian flap, a deltopectoral flap, basing its vascular supplies upon the branches of intercostal vessels, has been used frequently to reconstruct deformities that involve the lower face and the neck (Fig. 51.2).9–12
Z-plasty
Surgical release of a tight band can be achieved by switching right angularly two triangular skin flaps 60° with their catheti formed in continuity along the axis of a tight scar, i.e. the z-plasty technique.13–15 Although the technique is suited for releasing a tight scar band across a joint surface, in practice a scarred area is seldom left with unburned skin on both sides of a burn scar band. Consequently, the relief of contraction obtainable by means of classic z-plasty technique may be limited.
Modified z-plasty alias  z-plasty
z-plasty
Switching or transferring the flaps, unlike a z-plasty technique, is limited to one, as the opposing 90° skin flap fabricated by incising a contracted scar is unmovable. The narrower flap is rotated 90° to make up an open wound resulted from releasing maneuver (Fig. 51.3).
 Fasciocutaneous z-plasty
Fasciocutaneous z-plasty
The flap length versus width ratio of a random skin flap may be increased from a standard 2 : 1 to 4 : 1 if not to 5 : 1, by including the underlying fascial layer in the flap fabrication. That is also to say that a long and narrow skin flap may be easily fabricated to make up an open wound that is long (Fig. 51.4).
Flap techniques to reconstruct common burn deformities
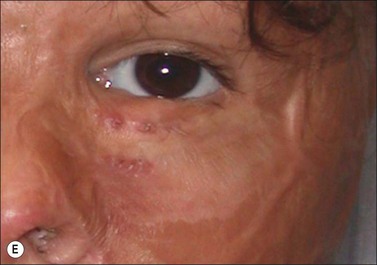
The eyelid deformities
Although the use of a skin graft has been advocated as the method to reconstruct eyelid deformities, i.e. eyelid ectropion and entropion, recurrence of contraction is quite common. The use of a nasolabial skin flap is a preferred technique to reconstruct ectropic or entropic deformities of the lower eyelid. It provides the tissue bulk needed and the means for a complex eyelid reconstruction that requires the use of cartilage graft (Fig. 51.5).








 z-plasty.
z-plasty.