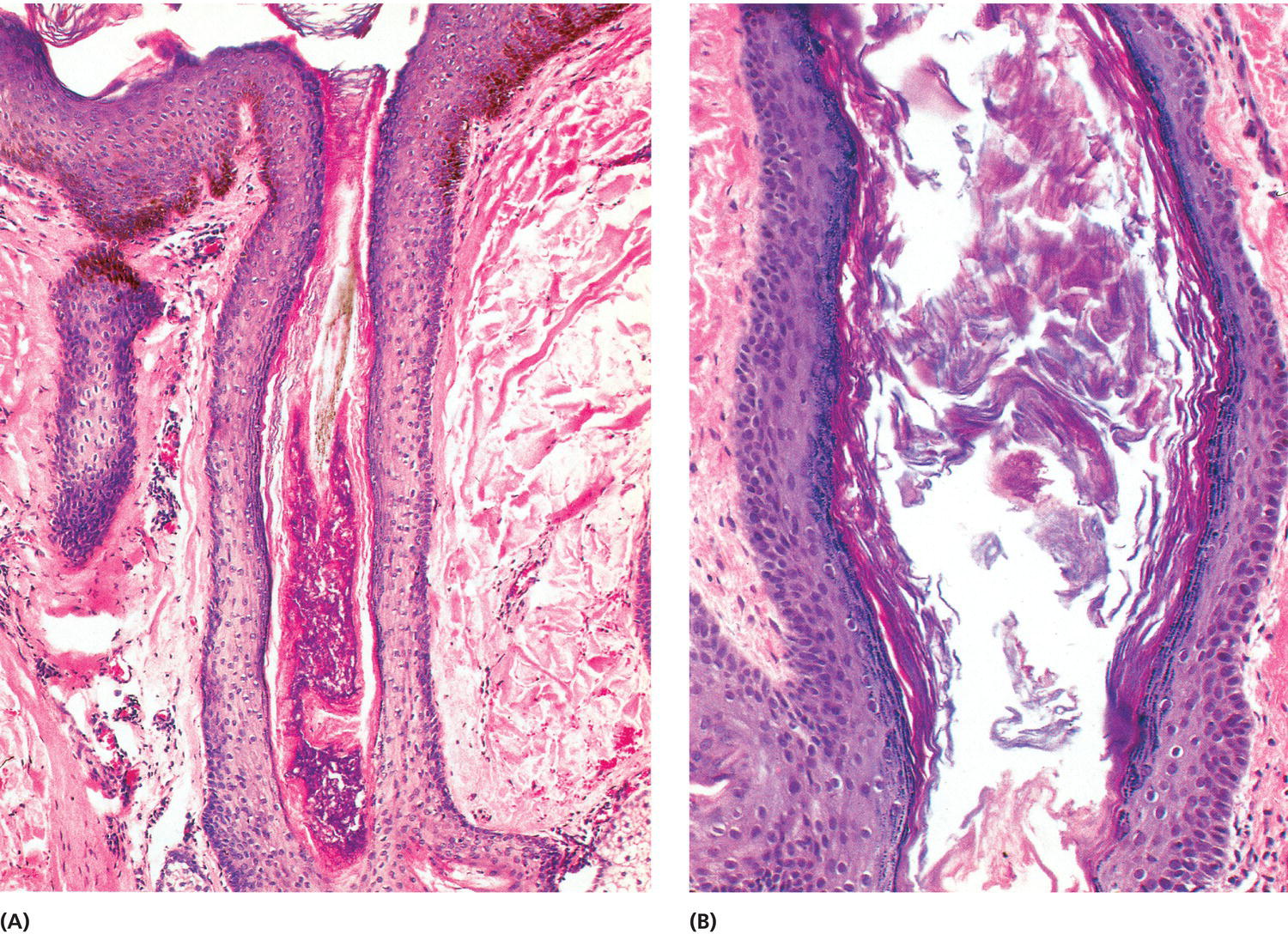
Chapter 1 The visibility of the lesions of acne vulgaris and acne rosacea as we present ourselves to the world and interact with others is a source of anguish to many. The hidden lesions of acne inversa (hidradenitis suppurativa) may interfere even with the most basic social interactions. The most profound effect of the acnes is on the psyche, so that aspect will be discussed “up front,” but first we need to know what we are talking about. Vulgaris is a Latin word, an adjective that means common. It is not a pleasant term, but it is descriptive (even a little vulgar). It is also highly accurate because the lifetime risk of acne in developed countries with “Western” diets is 85–90% of the population. Indeed, acne vulgaris is so common that even senior dermatologists (who should know better) have stated, “Children as young as 7 years of age can present with mild, usually comedonal disease, which most often is a normal physiologic occurrence.” To avoid embarrassing the author, no reference is provided. If I agreed with the statement that acne is “normal” (or “physiologic”), there would be no point to this book. My purpose in writing it is to draw together numerous threads of information, from very old to very new. I want to define the problem. Then I want to explain how this disorder (and its relatives) arises. Only then can we sort out how to treat it (and its various types) in as logical a fashion as possible. So let’s get started—at the beginning. Acne occurs when a plug forms in the follicular portion of the little oil gland and hair follicle organs on the skin called, in the older literature, pilosebaceous units. Here they will be called folliculopilosebaceous units (FPSUs), for reasons discussed in the Introduction. There are other small organs that develop from the underside of the skin: The eccrine sweat glands over most of our skin surfaces produce ordinary sweat. The apocrine sweat glands in our armpits and groin areas produce a different kind of sweat, plus a peculiar class of chemicals called pheromones. The mammary glands that form the breasts are derived in the same way, but obviously grow bigger than the others. These are all referred to as skin appendages. They all have their own diseases, and some may be related to acne. The first plugs that lead to acne occur in the structurally quiet, non-inflamed, and non-infected follicular portion of the FPSU. The story starts with a stimulus to the development of a structure named the Follikel-Filament [1], the first tiny accumulation of the lining cells, the keratinocytes, in the follicular duct (Figure 1.1a). These cells produce the tough linear protein called keratin that makes up the surface of our skin. When formed into a long thin fiber, keratin makes hair, and when produced in thick flat compact sheets, keratin becomes nail. Thin sheets of keratin, made of individual terminal keratinocytes, form the surface of skin and line the follicular portion of the FPSU. The process of formation of keratin by keratinocytes in the follicular canal and on the skin surface is called keratinization. Normally, as these cells mature they separate from each other toward the center of the follicular duct, and the loose cells are released into the ductal canal where they are pushed to the top of the duct by the flow of sebum. Accumulation of these flat cells in the follicle leads to the microcomedo (Figure 1.1b). This growth progresses next with larger and larger masses of these lining keratinocytes, leading to the physical plugging of the duct. Next come microbial colonization and overgrowth of preexisting bacterial and yeast colonies. This continues at the same time as the increased plugging. The increase in intrafollicular mass causes expansion, leaking, and then rupture of the follicular unit. Figure 1.1 (A) The first tiny accumulation of the lining cells, the keratinocytes, in the follicular duct. (B) Accumulation of these flat cells in the follicle leads to the microcomedo. The pilar unit is unaffected in early acne. It just keeps doing its job, which is to make hair, some of which may become trapped in the plugged and dilated follicular unit. That hair normally becomes increasingly coarse during the teen years, especially in boys, and has the effect of keeping the larger FPSUs open and uninvolved in the acne process. The sebaceous unit is also growing and producing more sebum. At body temperature, that sebum is a liquid. It quietly percolates to the surface, through and around the plugs, and is responsible for von Jacobi–Pringle’s “peculiar seborrhoeic condition,” the oily skin of acne that we all recognize [2]. It also happens to be the preferred food for the organisms that come to live in the follicular unit, so that encourages their growth. Much more on them later (Section 6.0). The leaking and rupture of the follicular unit of the FPSU are intimately involved with inflammation. This is a huge and very complex area. Hundreds of papers have been written on the subject. As of this writing, there have been 619 papers since 1952. I don’t plan to review them all here, but you need to know that there is serious debate as to what starts the process. Does the plugging of the follicular unit come first, with pressure-induced leakage leading to inflammation [2]? Or does very early inflammation actually stimulate the plugging of the duct to produce excessive numbers of ductal cells [3]? My personal belief is that hormones plug the pore, and that causes the expansion that leads to the leaking, which leads to the inflammation. My reasoning is simple: the organisms said to trigger the inflammation that triggers the keratinization are present in almost everyone, throughout life, and are in no greater number in acne patients than in normal persons [2]. If these organisms were the cause, we would all have acne, all the time. There has to be a factor that comes on at puberty, and generally leaves at the onset of maturity, in order to explain the timeline of acne in our population. More on that later (Section 2.6). There also needs to be a trigger that links the overproduction of the keratinocytes in the follicular duct to the onset of inflammation. That may be a recently described simple product of the pressure and hypoxia that build up in the follicular duct. More on that as well later. Whether inflammation starts the plugging process or is a response to early leakage of materials from the FPSU, inflammation is seen as a target for therapy. For hundreds of years, physicians have been treating acne by trying to suppress the inflammation. I will try to convince you in this book that treating the inflammation is like chasing the horse after he has left the burning barn. Far more important is preventing the fire in the first place. The “inflammatory process” doesn’t just cause inflammation. It is often forgotten that its main chore is to repair the damage caused. Sometimes, the inflammatory process stops with simple healing of the wall of the follicular unit. In the absence of repair, the inflammatory reaction just keeps burning. Unfortunately, that leads to much more destruction. The contents of the dilated follicles leak or explode into the tissue under the skin surface. That causes more inflammation and leads to scarring. This prolonged destructive inflammatory activity is the cause of the tender nodules that are so ugly. Untreated, resolution occurs over a long time period, often years. This is referred to as “burning out” of acne. It leads to loss of parts of the FPSU, or the entire FPSU can be destroyed. It also leaves serious scarring behind. The primary target of acne therapy must be the prevention of the environment that produces the Follikel-Filament and so the microcomedo [1]. All the other events are “downstream” and secondary. These downstream events are called epiphenomena—things that happen “on top of” (that is what epi means) other things. Management of acne has for over a century concentrated upon suppressing these epiphenomena, while ignoring the real cause of the disease. It is time to address the cause. Classic acne rosacea is a variant of the acnes that shows up on the curved surfaces of the face (Figure 1.2). It is made up of blemishes centered on the openings of the follicular units of individual FPSUs. There are little raised bumps (folliculopapules) and very small pustules (folliculopustules). These little bumps and pustules are the “acne,” and they appear on a rosy-red background, the “rosacea.” The word rosacea has been used for a couple of hundred years as an adjective to modify the noun acne. So acne rosacea is really just rose-colored acne. Figure 1.2 Acne rosacea loves convex, sun-exposed skin with a healthy population of well-stimulated FPSUs. The word rosacea is now seen in the public eye and in some dermatological writing. The adjective has become a noun, and rosacea has become a “disease” or “condition” all by itself. See Appendix A for more on the name’s change. It is important to understand that acne rosacea actually has three separate components on the face. The first is the pimply acne, the second is the background redness (Figure 1.3), and the third is a thickening of the skin. There are also eye changes that cause a fourth, separate, but associated condition, but it is not always present. Figure 1.3 Some dermatologists consider this “pre-rosacea.” Close inspection reveals a few comedones—almost normal in a 15 year old. He needs lifelong, truly broad-spectrum sun protection to prevent worsening of his actinic telangiectasia; a dairy-free diet; and a gentle topical retinoid. Just as acne vulgaris always starts with plugs in the follicles that show up as comedones (blackheads) when mature, true acne rosacea always has the folliculopapulopustular lesions instead. Indeed, the presence of visible comedones rules out acne rosacea as the prime diagnosis. Just to confuse the issue, there are occasional patients who have both acne rosacea and acne vulgaris. The little bumps and pustules are caused by the body’s immune systems (both of them) reacting to “stuff” that is caught in the pore. This is an automatic rejection reaction aimed at things like bacteria and yeasts, some tiny beasties called Demodex (see Section 6.4), and little ingrown hairs. This reaction is the job of the innate immune system. Innate means inborn or born with, and it is the part of the immune system that does not need to “learn” what to do with foreign material. We are able, from birth, to recognize various foreign materials, and this part of the immune system is aimed automatically at anything in the pores or escaping under the skin from the pores that it recognizes as foreign material. It can be triggered by anything from tiny viruses to large ingrown hairs. (See Section 7.1.) There is also a second part of the reaction caused by the “adaptive” immune system. Its job is to recognize, target, and eliminate foreign material when the innate immune system needs some extra help. It sometimes gets involved as well, but it takes a little while to get going, because it needs time to learn how to “adapt” to a new threat. There is much more on that to come (see Section 7.2). The redness (erythema) that causes the rosy color is made up of three separate components: The first, structural erythema, is due to dilated blood vessels. These are sometimes called broken blood vessels, but they are not really broken. Their structure is actually dilated, which just means they are increased in diameter and so are carrying more blood than usual as a result (Figure 1.4). More blood in the blood vessels makes the skin redder than usual. Structural dilation of a blood vessel is due to a gradual weakening of its walls that allows the blood vessel to bulge. Early bulging of very fine facial blood vessels is due to minor injury, most commonly from sun exposure. Even babies (who are usually protected against direct sunlight) will show pink cheeks. This is the earliest sign of actinic telangiectasia, the permanent and visible dilated blood vessels just under the skin surface. In a letter to the British Medical Journal in 1976, Dr. Ronald Marks stated that we have pointed out that the upper dermis in rosacea is quite abnormal and shows evidence of both solar elastotic degeneration considerably in advance of what might reasonably be expected for a group of middle-aged Britishers and other dystrophic changes that are not easily categorized. Autoradiographs after injection of tritiated thymidine and enzyme histochemical tests have suggested that small dermal blood vessels are also involved in rosacea (probably secondarily). It is my belief, based on these findings, that the primary disorder is a dermal dystrophy resulting from “weathering” (sun, wind, and cold) and an inherent susceptibility to this process. The dermal attenuation produced in this way causes lack of dermal support for the sub papillary venous plexus, allowing these channels (and the neighboring lymphatics) to dilate enormously. The flushing seen in rosacea is in all probability the result of the vessel dilatation – not its cause. The dilated vessels could become incompetent in addition as a result of the persistent and extreme pooling seen in them and this in turn may lead to diffusion of injurious macromolecules and mediators of the inflammatory process into the dermis. [4] Figure 1.4 Longstanding sun exposure gradually weakens the collagen and other support tissues that wrap around and support the blood vessels, allowing them to dilate. The blood pools in them and turns dark, as on this man’s nose. Dr. Marks labels this as a hypothetical process, with which I agree, but I can conceive of no other reasonable hypothesis that so neatly explains the features we see. Kligman supports this view in his essay on the subject, stating, “I, and others, regard rosacea as fundamentally a vascular disorder” [5]. In researching the literature while writing this chapter, I was delighted to find such valuable support for my working theory of the disorder (which follows shortly), but having read the supportive opinions of the experts, the next question of course must be “What is the vascular abnormality, and what causes it?” The question is neither addressed nor answered by Marks or Kligman. Instead, Kligman pointed out that the “histopathology of rosacea always shows the classic signs of damage to the dermal matrix, namely elastosis, collagenolysis, and increased glycosaminoglycans.” He felt the changes were so similar to those seen in the advanced photodamage seen in the fair and often freckled skin of men of Celtic heritage that separating the two “is difficult and may be fruitless because the two may come together,” but neither he nor Professor Marks went so far as to suggest that this actinic damage might extend to weakening of the other collagenous supporting tissues in the area. I strongly suspect that damage to the supporting material of the follicular portion of the FPSU occurs simultaneously as a concurrent or parallel process. Furthermore, I would be willing to suggest that both Kligman and Marks would be likely, upon reflection, to admit that as a possibility. Indeed, the reason that rosacea and actinic damage “may come together,” as Kligman wrote, is very simple. I believe they are one and the same process. The impact on dermal collagen causes wrinkles; the impact of sun on the collagen that wraps blood vessels causes the blood vessels to dilate, producing the condition called actinic telangiectasia (discussed in this section); and the impact on the collagen wrapping the FPSU allows the follicular part of the FPSU to dilate when subjected to internal pressure. And when a weakened follicle dilates, it bursts. Where does it burst? Exactly where you would expect—where the damage from the sun is at its worst—at the top of the follicle where the sun has its greatest impact. Older sun-exposed and collagen-damaged follicular units simply have no chance of making comedones, especially if they are the small short follicles in the superficial dermis of a fair-skinned Celt who doesn’t have the deep and voluminous FPSUs that harbor deep aggressive acne. The follicular units of these shorter and smaller FPSUs simply leak or rupture first, producing the papules and pustules of classic acne rosacea because they cannot maintain their structural integrity long enough to progress to or support comedo formation. Actinic means caused by the sun’s rays, and telangiectasia is the condition of having lots of actinic telangiectases (the plural of telangiectasis, the word that describes the involvement of a single vessel). If you look closely, even with a magnifying glass, you will see only a pink blush in the early stages. As time passes, however, the little dilated vessels’ walls absorb more ultraviolet light from the sun. That causes more sun damage. Extensive telangiectatic sun damage is easily observed on the cheeks of Peruvian children in the mountains near Cuzco, Peru. The combination of high altitude (about 3800 m) and daily exposure worsens and accentuates the damage. To understand the mechanics of the problem, first take a look at a common garden hose to gain some insight into how blood vessels are constructed. There is an inner lining that forms a very fragile tube to carry the blood. Around that is a layer of supporting tissue that looks like the concentric woven strings you can see in the wall of a garden hose, and then there is the outside support material. Much of this support material in blood vessels is collagen. When collagen is damaged by ultraviolet light, it deteriorates. That is what causes wrinkles. Take a look at stained skin sections under the microscope, noting the pink and highly structured collagen in the dermis of young healthy skin, and then look at the gray-blue mush in sun-damaged skin. The same thing happens, I propose, to the fine supporting strings wrapped around blood vessels. With such loss of the original firm healthy structure, the blood vessels weaken further. That allows them to dilate, and so more blood will be carried. The vessels actually structurally expand in cross-sectional area so they become big enough to be visible just by looking at them up close. Over the years, these blood vessels can dilate hugely. They become visible at social distances or even from across a room. The tendency to develop this background facial redness is partly genetic, a point not lost on Prof. Marks and emphasized by Prof. Kligman, who estimated “that the prevalence may approach 35% in adult women of Scotch [sic]-Irish-Welsh Celtic ancestry.” Further, he states, “I regard rosacea as belonging to the general class of photosensitivity disorders.” Certainly, it is generally developed and worsened by sun exposure, so the fair and freckled part of the population is at greatest risk. This vascular damage is not, by itself, acne rosacea. This is, purely and simply, actinic (or solar, if you prefer) telangiectasia—caused by photodamage that led to dilated blood vessels. It has no hope of clearing with oral antibiotics or topical creams, lotions, gels, foams, or ointments. The best treatment for structural erythema is preemptive and consists of Second best is active selective photothermolysis with laser or intense pulsed light (IPL) therapy. More on those later (Section 8.8). The second component of the redness is functional erythema, and that relates to the increase in blood flow through the dilated blood vessels. The increased flow reflects temporary wider opening of the vessels. This comes and goes, and these temporary changes are of course reversible. The simple maiden’s blush (and the even more embarrassing male counterpart) is a classic temporary high-blood-flow condition. It can come in seconds and vanish in less than a minute. The menopausal “flush” or “hot flash” that can be so embarrassing as a marker of “the change” is a more prominent and longer lasting (but still temporary) episode of high blood flow. Other longer lasting but temporarily dilators of blood vessels that cause functional erythema are sun, cold, wind, hot drinks and soups, caffeinated drinks, some drugs like niacin, and alcohol of all sorts. And then there is a special third category of redness—that caused by inflammation. This is best called inflammatory vasodilation, and is both functional and structural. It is the only part of the redness that can actually be treated (even if only partly) with the medications generally used for “rosacea.” If it is possible to get rid of the inflammation, the redness will fade to a certain extent. That will help reduce the color. That is where the tetracycline family of anti-inflammatory antibiotics can be very useful. Note that decreasing or eliminating bacteria or yeast or Demodex-induced inflammation will reduce the associated inflammatory vasodilation but will not touch the redness from structural dilation. Note that the inflammation that causes the functional redness can also damage the walls of the blood vessels, further weakening them and contributing even more to the structural dilation of the blood vessels. So why is this important? It is absolutely essential that patients understand that only part of the redness will respond to medications. I have seen dozens of patients over the years who have been on long-term antibiotics and numerous other medications, either topically or by mouth, who are frustrated by the expense of the medications, their side effects, and the lack of response of the redness to them. Setting reasonable expectations for patients will go a long way toward avoiding therapeutic disappointment. The failure to explain this can lead to misunderstanding, frustration, and friction between patient and physician. anti-inflammatory medication, whether topical or oral, does absolutely nothing for purely structural erythema or purely functional erythema. Topical brimonidine gel or even topical oxymetazoline nasal drops or spray provide a temporary paling effect. The classic “end stage” of acne rosacea is the rhinophyma, or the “drinker’s nose.” This is relatively rare, fortunately, and is caused by an increase in thickness of the involved tissue that is termed a phymatous change, from the Greek word phyma meaning nodule or swelling (Figure 0.33). The nose is most commonly involved, although the cheeks, forehead, and chin may sport the disorder. W.C. Fields is the actor and personality most often associated with rhinophyma, but President William J. Clinton may be a more familiar face. Alcohol intake has been suspected as a co-factor but need not be present. The true cause may (again, hypothetically) be suspected by reference to the progressive fibrosis that occurs in areas of chronic edema of the lower extremities, a component of stasis dermatitis often seen on biopsy. Some individuals may simply be sufficiently susceptible to overproduction of such material either on their lower extremities or as a result of stasis in the dermis of the face, induced secondarily, as Prof. Marks would suggest, by the vascular damage caused by the sun, not only to the venules but to the lymphatics as well. This results in leakage of proteins and induction of a fibrotic reaction that thickens the areas under the skin in the facial area, and occurs on the lower leg due to gravity and senior citizenship. The reason why all patients with rosacea do not progress to phyma formation remains a mystery. There does seem to be a genetic predisposition, but choosing new parents is not an option in this age group. If an itchy, scratchy, or gritty feeling in the eyes occurs in association with other signs of acne rosacea, then consider the diagnosis of ocular rosacea. There is dilation of the blood vessels on the surface of the sclerae (the whites of the eyes) and a swelling of the tissues around the eyes, particularly the eyelids and the eyelid margins (see Figure 0.34). This disorder does not seem to appear often as an isolated ophthalmological disease, so it seems to be truly related to cutaneous acne rosacea. The mechanism of its cause, however, is as mysterious as the cause of rhinophyma. While there is no denying that acne rosacea is usually associated with background redness, patients with background erythema and telangiectasia may experience redness and flushing alone. Other individuals with actinic telangiectasia may have bumps alone or bumps and pimples together, with or without phyma formation (thickening of the involved skin), and with or without ocular (eye) rosacea. Combinations of all six features are common, but real acne rosacea starts in the little oil- and hair-producing organs, the FPSUs that populate all but a few areas of our body surface. So what is the common thread that connects the redness with the bumpiness and the little pustules? We need to go back and look at several parts of the whole, and then tie them all together. First, we need to review what we know about the epidermal appendages that host this disorder. As discussed elsewhere, we need to use a name that is anatomically more accurate, because the follicular component plays an underrecognized role in the pathogenesis of all the acnes. These appendages have three components, so they are better called folliculopilosebaceous units (FPSUs) (see Figure 0.20) to reflect their actual anatomy. In classic acne rosacea, there are papules and pustules just like those in some forms of acne vulgaris, but in acne rosacea there is something missing. Consider the curious lack of comedones. This is a major clue to what is going on. If you take a close look at the lesions of acne rosacea, and talk to the patients who suffer from this disorder, two facts emerge. First, the folliculopapules come up fairly quickly, and they turn into folliculopustules fairly quickly, then they burst and heal, also fairly quickly. When they do burst, there is no “core” or “plug” in the material that exits the folliculopustule. There is usually nothing visible except pus. Acne surgery (Section 8.7.1) is not needed to remove retained foreign material. The involved FPSUs do not spend months gradually building up to the point that the wall of the duct is weakened, leaks, and then ruptures as happens with acne vulgaris. Acne rosacea is different from acne vulgaris; it is quicker and shallower. Why should that be? It appears that the same processes that are acting on healthy young FPSUs in acne vulgaris have an entirely different effect on the FPSUs of patients with acne rosacea. For an explanation, we need to look back to the section on actinic telangiectasia (Section 1.2.2, “The ‘Redness’ Part”). What causes the telangiectases to form? Profs Marks and Kligman agreed that this was caused by damage to the support structure of the thin walls of the capillaries in the upper layers of the dermis. And what causes that damage? Ultraviolet (UV) light, specifically the damaging “superficial” UVB and the “deeper” UVA rays of wavelengths from 280 to 400 nm. This is the same ultraviolet light that damages the collagen supporting the fresh smooth face of youth. For an example, look at another comedonal disease, Favre–Racouchot syndrome. It is not common, but its presentation and location are classic examples of what too much UV light can do on the convex curved surfaces of the face. It is apparent that destruction or weakening of the support tissue, the fibrous root sheath, and its analogs (Section 0.4) allows dilation of the duct and permits development of the classic picture in that disorder. Indeed, the full descriptive name of Favre–Racouchot syndrome is “solar elastosis with comedones” (Figure 1.5). Figure 1.5 Longstanding sun exposure gradually weakens the collagen and other support tissues that wrap around and support the follicular units, allowing them to dilate. The keratin and some sebum pool in them, and some even turn dark, as on this man’s cheek. That picture takes a long time to develop, but the physical location on the convex facial surface of the malar, orbital rim, and zygomatic areas of the face plus the associated actinic damage bear witness to the likelihood that the pathogenesis is mediated by photodamage. There is simply not enough stretch in that thin material, wrapped like a vinyl glove around the FPSU, to push these blackheads out of the weak-walled and dilated follicular canals. If you have ever had the opportunity to (sorry to offend anyone) squeeze the material out of Favre–Racouchot lesions, you will know that the keratinous mass is soft, mushy, and greasy. Its mechanism of formation relies on the weakness of the duct, the duct’s expansion, and the failure of the overly compliant follicular wall to contain the mass and generate the pressure required to empty the passively filling follicular unit. This is a compliant variation of the mechanism and sequence of events that produce the hard keratinous plug in acne vulgaris. So let’s apply what we know about sun damage to acne rosacea. Look at the intimate association of the papulopustules of classic acne rosacea with actinic telangiectasia. They are basically located on top of each other. While this has led to a new classification of this disorder, the close relationship of these two features of the disorder has been, I believe, misinterpreted. This is not just a geographic association of two different processes; it is one single environmental impact that is responsible for the two most prominent features of the disorder. I propose that UVA and UVB exposure is sufficiently potent and penetrating to damage the collagenous sheath that supports the wall of the follicular unit. In youth, this support structure is quite strong and forms a natural constrictive resistance. Newly formed keratinocytes and sebum press against it and are forced toward the surface by the resistance provided, so the pressure created empties the duct. That allows no time for the microcomedo to accumulate, and in youth it is unusual to have the sheath (that vinyl glove again) weakened by UV photodamage. But the rupture of the sun-weakened ducts’ support does occur on occasion. Acne vulgaris flared by sunlight does occur. But, more importantly, this supports the suggestion that the reason why there are no comedones in acne rosacea and the reason why acne rosacea lesions are short-lived are pretty simple, and they are identical in both cases. The explanation is simply that the walls of the follicular portion of the FPSU are weakened by the same UV light that caused the actinic telangiectasia. Acne rosacea pores simply lack the ability to resist the early expansion of the follicular canal, and they burst early in the game. Indeed, they burst long before the follicular canal has a chance to make a visible comedo. The break occurs at the top end of the follicle, because that is where the sun damage is the worst. Likewise, these weak follicular canal walls are so thinned that they leak easily, which leads to early activation of the innate and adaptive immune systems, so pustule formation and destruction of the upper end of the FPSU also occur early. In short, acne rosacea is a distinct variant of the folliculo-occlusive disorders called the acnes. The basic cause of the lesions is identical in all acne types, but acne rosacea is localized to its specific distribution because of solar exposure. That sets the stage for the other players on the field, and that is a whole different story. Each of the three acnes is distinct. The distinctions include location, time of life, the impact of environmental variables, response to therapy, lesion type, and the triggers. The eruptions of acne rosacea occur mainly on the face and in sun-exposed areas, and the general pattern is of follicular plugging, early rupture, inflammatory reaction, and healing. The reasons for the plugging and rupture are explained in this chapter, and ways to prevent, modify, and treat them will be dealt with in this volume. In addition, there are a number of variables that are important in the development of the inflammatory reaction. Inflammation in acne rosacea, as in all acnes, is driven by the immune systems responding to materials considered a threat to the organism. As described in Section 7.1, that means that anything that should be “outside” (or above) the basement membrane is considered the enemy (see Figure 2.7). Foreign material on the surface, if it gains access through a scratch or cut, will be attacked. Likewise, anything that is caught under the epidermis (like an ingrown hair) or takes up residence in the pores (there are several organisms to consider) has the potential to stir up trouble. It is time to look at these. There are five sets of troublemakers that occupy the follicular portion of the FPSU: It is assumed that there are also bits of retained adherent keratinocytes in this material, and it is generally understood that loose keratin under the skin is not welcomed by the innate immune system. When an epidermoid cyst ruptures under the skin, exposing released keratin, it is sterile but it causes a massively hot and tender inflammatory reaction that is often mistaken by the unaware for infection. The resolution of such lesions, brought about by simply removing the keratin (and the germinative epithelium surrounding it), is both swift and impressive. Likewise, simply opening these little rosacea pustules brings about a very quick overnight cooling of the lesions. Figure 1.6 This family of adult, juvenile, and a baby Demodex mite had occupied a pustule on the forehead of a rosacea patient. The background shows pus and a keratinous plug (plus some round air bubbles). Figure 1.7 The innate immune system reacts to ingrown hairs, likely even the tiny ones like this, caught in a keratinous plug in a folliculopustule in acne rosacea. First, it is everywhere. Cultures of this yeast, using material taken from the scalp, its natural reservoir, are almost universally positive. It loves to live where its natural food, oil from the sebaceous glands, is present. Second, it doesn’t always cause disease. Indeed, there is a good case to be made that it is the victim, not the aggressor. Third, it has relatives (there are 14 Malassezia species in all), and a close relative, M. globosa, appears to be responsible for the seborrheic group of disorders [10]. This trio of facts makes it very difficult to actually prove the relationship between the yeast and several cutaneous disorders. The yeast is accepted as having a causative role in tinea (or pityriasis) versicolor, and the same is generally true of Malassezia folliculitis of the upper back, upper chest, and shoulders, but there is ongoing discussion about its role in seborrheic dermatitis, psoriasis, and atopic dermatitis. And when it comes to acne vulgaris and acne rosacea, there is hardly a mention in the modern literature. In making the case for Malassezia
The three acnes and their impact
1.1 Acne vulgaris
1.1.1 Terminology
1.1.2 The starting point
1.2 Acne rosacea


1.2.1 The “pimply” part
1.2.2 The “redness” part

1.2.3 The third part, the firm fibrosis
1.2.4 Part four—ocular rosacea
1.2.5 Putting it all together

1.2.6 The inflammatory epiphenomena in acne rosacea


![]()
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree






