This article discusses the use of the sternohyoid muscle for facial reanimation. The report outlines the rationale for use, the technical aspects of flap harvest, and early clinical outcomes. The utility of the flap and its comparative attributes relative to the gracilis flap are discussed.
Key points
- •
The sternohyoid muscle can be harvested as a free flap for microvascular transfer.
- •
The sternohyoid offers comparatively better anatomic size match to the zygomaticus major muscle compared with the gracilis.
- •
The sternohyoid has a better fiber type match to the zygomaticus major based on ATPase staining.
- •
Early clinical outcomes are promising, but significant further study and long-term outcomes must be evaluated before this flap can supplant the gracilis as the gold standard for neuromuscular free flap based facial reanimation.
Introduction
The rehabilitation facial nerve paralysis associated with nerve transection is ideally accomplished through neuromuscular reanimation of the face. When possible, the best case scenario is reestablishing a neural connection between the native facial nerve branch and its specific facial musculature target at a distal location in the nerve that would restore to the closest approximation normal facial function. Unfortunately this ideal situation is rarely encountered in the clinical setting. In most cases, nerve transection or resection occurs proximal to the pes anserinus, which in turn inherently predisposes recovery to synkinesis. Even this option becomes unavailable in long-standing cases of paralysis. Beyond 18 to 24 months after injury, the motor endplates of the denervated muscles irreversibly atrophy. In this situation, a neuromuscular transfer incorporating both a new neural input source and muscular mechanism is necessary. The 2 most commonly used options in these circumstances are local transfer of the temporalis tendon in an orthodromic fashion or free muscle transfer utilizing the gracilis muscle. These 2 options are discussed in other articles within this issue.
Of the free tissue transfer options, the most commonly used and widely accepted is the gracilis flap. This is at present considered the gold standard for microvascular flaps used in reanimation procedures. In an optimal outcome, this technique allows the rehabilitation of a spontaneous smile. This muscle has become the mainstay of free tissue facial reanimation. It is used widely in pediatric and adult indications with relatively good outcomes and results. The ease of harvest and reliability of the flap have made it an excellent option in patients with long-standing paralysis.
The use of this flap is not, however, without its limitations. There are anatomic parameters of the gracilis that can make the results suboptimal. The most frequently cited concern is the bulk of the flap, especially in relation to the temporal region and the zygoma. The skin envelope and soft tissue overlying the zygoma in adults are generally less than 8 mm thick. Draping a free muscle flap over this convex bony landmark often creates a visible facial deformity. This is less than ideal given the purpose of facial nerve rehabilitation and reanimation is to reduce physical deformity. The flap works well in children and young adults with ample facial volume, but when used in older patients who are usually affected by parotid malignancy and who usually have concurrent weight loss and facial atrophy, the flap is difficult to camouflage.
Many authors have reported successful volume reduction of the harvested gracilis flap as a modification to reduce this problem. Even with such pre-emptive measures, the muscle bulk is significantly larger than the zygomaticus major/minor that the gracilis is intended to functionally replace. Not surprisingly, the flap is noted to be more favorable aesthetically in younger patients, in whom the facial soft tissue envelope is proportionately thicker and more robust.
The numerous modifications of the gracilis reported in the literature highlight the historical reality that this flap was not originally designed and reported as a means to rehabilitate facial nerve paralysis. Initial reports in the literature and the widespread use of this flap were for indications in the peripheral extremities (eg, wound coverage). Over time, the flap has been regarded as a well-established muscle flap with a reliable pedicle and nerve input that could be harvested with ease. This clinical history and reliability led to its eventual use in the face, but the choice of this muscle for this particular indication was not based on a directed search for the ideal muscle to replace facial musculature.
There are other characteristics of the gracilis flap that are less than ideal. When considering a number of parameters, including muscle size, length contraction/ratio, intrinsic type 1/type 2 fiber ratios (although these can shift to some extent with reinnervation in certain muscle transfers), the muscle is quite distinct from the Zygomaticus major.
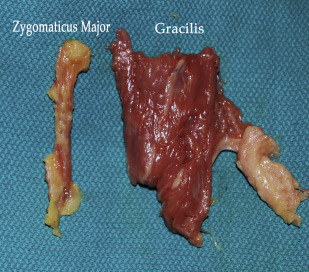
An anatomic comparison of the 2 muscles is shown in Fig. 1 . The images illustrate an obvious difference in the size of the muscles. The average length of the gracilis muscle in an adult man is 41 cm, and only a small portion of the muscle is harvested in a facial reanimation procedure. The length/contraction ratio of the muscle for the lengths harvested for facial reanimation is therefore unfavorable in contrast to that seen in the zygomaticus major, which only averages 5 cm in length and can have discursion over 2 cm in some cases.
Another potential difference is in muscle physiology. A comparison of fast twitch type II muscle fiber activity of the gracilis to the zygomaticus major shows significant differences between these muscles. The author’s findings are shown in Fig. 2 , and they corroborate the accepted literature. This is not unexpected when one considers the purpose of these muscles and their function within their native location. The gracilis is a muscle that is involved in chronic low-grade contraction associated with maintaining balance and stability of the torso. The zygomaticus major, in contrast, is involved in rapid facial expression and has almost the highest ratio of fast twitch fibers of any muscle in the body just behind the orbicularis oculi.
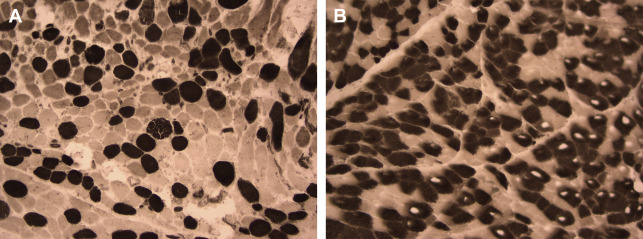
Because muscle fiber type is thought to be determined by the neural innvervation source, this may not represent a clinical problem, but the limited data available on gracilis flaps suggest this transformation is not seen clinically.
This led the author and colleagues to a directed need-based search for an alternative to the gracilis as a potential free flap for facial reanimation. Ideally, this flap would have several characteristics:
- 1.
Reliable and nonessential vascular pedicle
- 2.
Motor nerve input with a reliable nerve (nonessential function, appropriate length, diameter, branching)
- 3.
Fast twitch muscle fibers with a rapid and brisk contraction profile or clinical evidence of fiber type transition with reinnervation
- 4.
Shorter length from origin to insertion and a superior length/contraction ratio
- 5.
Rigid or semirigid origin/insertion point for better fixation
- 6.
Smaller muscle mass and size ( Fig. 3 )
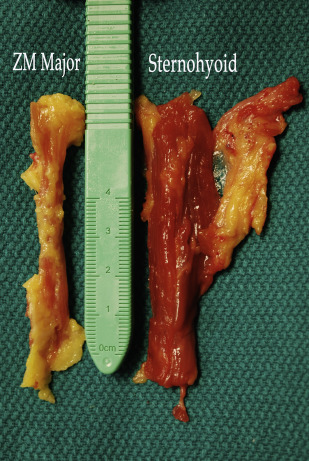
Fig. 3
An equivalent length of zygomaticus major ( left ) and harvested sternohyoid flap ( right ) for comparison of size and volume.
Using these criteria, the author and colleagues hypothesized the sternohyoid muscle potentially could be an ideal replacement. The vascular supply of the strap muscles had been previously shown as potentially reliable for use as a pedicled flap, but its potential use as a free flap had not been reported.
The findings of a preclinical, cadaver-based study that described this novel flap were reported in The Archives of Facial Plastic Surgery . Details of the operative technique and a comprehensive description of the flap are provided from that study. Specific diagrams are reprinted here with permission.
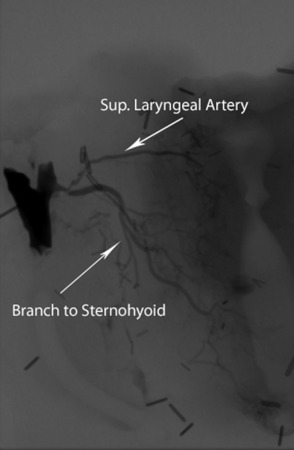
The conclusion of this work documented that the sternohyoid muscle could reliably be harvested as a free flap with a pedicle based on the superior thyroid vessel. A representative angiogram is shown in Fig. 4 . The flap has a pedicle length of over 5 cm and a reliable long motor nerve in the ansa branches.
Introduction
The rehabilitation facial nerve paralysis associated with nerve transection is ideally accomplished through neuromuscular reanimation of the face. When possible, the best case scenario is reestablishing a neural connection between the native facial nerve branch and its specific facial musculature target at a distal location in the nerve that would restore to the closest approximation normal facial function. Unfortunately this ideal situation is rarely encountered in the clinical setting. In most cases, nerve transection or resection occurs proximal to the pes anserinus, which in turn inherently predisposes recovery to synkinesis. Even this option becomes unavailable in long-standing cases of paralysis. Beyond 18 to 24 months after injury, the motor endplates of the denervated muscles irreversibly atrophy. In this situation, a neuromuscular transfer incorporating both a new neural input source and muscular mechanism is necessary. The 2 most commonly used options in these circumstances are local transfer of the temporalis tendon in an orthodromic fashion or free muscle transfer utilizing the gracilis muscle. These 2 options are discussed in other articles within this issue.
Of the free tissue transfer options, the most commonly used and widely accepted is the gracilis flap. This is at present considered the gold standard for microvascular flaps used in reanimation procedures. In an optimal outcome, this technique allows the rehabilitation of a spontaneous smile. This muscle has become the mainstay of free tissue facial reanimation. It is used widely in pediatric and adult indications with relatively good outcomes and results. The ease of harvest and reliability of the flap have made it an excellent option in patients with long-standing paralysis.
The use of this flap is not, however, without its limitations. There are anatomic parameters of the gracilis that can make the results suboptimal. The most frequently cited concern is the bulk of the flap, especially in relation to the temporal region and the zygoma. The skin envelope and soft tissue overlying the zygoma in adults are generally less than 8 mm thick. Draping a free muscle flap over this convex bony landmark often creates a visible facial deformity. This is less than ideal given the purpose of facial nerve rehabilitation and reanimation is to reduce physical deformity. The flap works well in children and young adults with ample facial volume, but when used in older patients who are usually affected by parotid malignancy and who usually have concurrent weight loss and facial atrophy, the flap is difficult to camouflage.
Many authors have reported successful volume reduction of the harvested gracilis flap as a modification to reduce this problem. Even with such pre-emptive measures, the muscle bulk is significantly larger than the zygomaticus major/minor that the gracilis is intended to functionally replace. Not surprisingly, the flap is noted to be more favorable aesthetically in younger patients, in whom the facial soft tissue envelope is proportionately thicker and more robust.
The numerous modifications of the gracilis reported in the literature highlight the historical reality that this flap was not originally designed and reported as a means to rehabilitate facial nerve paralysis. Initial reports in the literature and the widespread use of this flap were for indications in the peripheral extremities (eg, wound coverage). Over time, the flap has been regarded as a well-established muscle flap with a reliable pedicle and nerve input that could be harvested with ease. This clinical history and reliability led to its eventual use in the face, but the choice of this muscle for this particular indication was not based on a directed search for the ideal muscle to replace facial musculature.
There are other characteristics of the gracilis flap that are less than ideal. When considering a number of parameters, including muscle size, length contraction/ratio, intrinsic type 1/type 2 fiber ratios (although these can shift to some extent with reinnervation in certain muscle transfers), the muscle is quite distinct from the Zygomaticus major.
An anatomic comparison of the 2 muscles is shown in Fig. 1 . The images illustrate an obvious difference in the size of the muscles. The average length of the gracilis muscle in an adult man is 41 cm, and only a small portion of the muscle is harvested in a facial reanimation procedure. The length/contraction ratio of the muscle for the lengths harvested for facial reanimation is therefore unfavorable in contrast to that seen in the zygomaticus major, which only averages 5 cm in length and can have discursion over 2 cm in some cases.








