Introduction94
INTRODUCTION
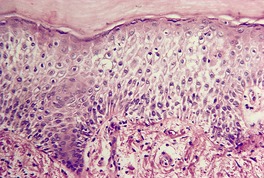
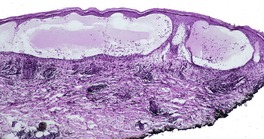
Fig. 5.1
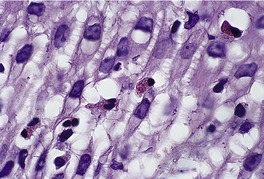
Fig. 5.2
Simulants of the spongiotic tissue reaction
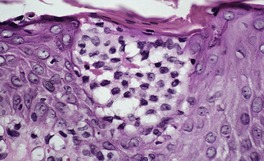
Fig. 5.3
Patterns of spongiosis
NEUTROPHILIC SPONGIOSIS
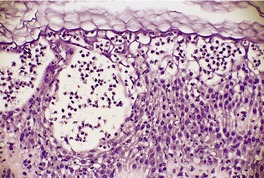
Fig. 5.4
PUSTULAR PSORIASIS
PRURIGO PIGMENTOSA
Histopathology
IgA PEMPHIGUS
ACUTE GENERALIZED EXANTHEMATOUS PUSTULOSIS
DERMATOPHYTOSES AND CANDIDOSIS
BEETLE (PAEDERUS) DERMATITIS
Histopathology
EOSINOPHILIC SPONGIOSIS
PEMPHIGUS (PRECURSOR LESIONS)
Histopathology
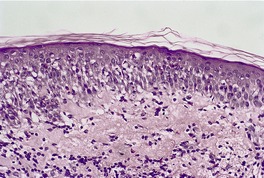
Fig. 5.5
PEMPHIGUS VEGETANS
BULLOUS PEMPHIGOID
IDIOPATHIC EOSINOPHILIC SPONGIOSIS
EOSINOPHILIC, POLYMORPHIC, AND PRURITIC ERUPTION
Histopathology
ALLERGIC CONTACT DERMATITIS
ARTHROPOD BITES
EOSINOPHILIC FOLLICULITIS
INCONTINENTIA PIGMENTI
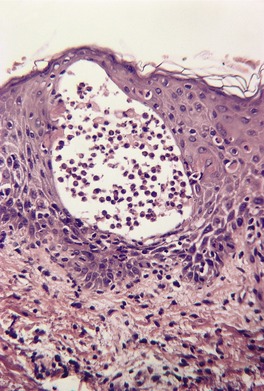
Fig. 5.6
MILIARIAL SPONGIOSIS
MILIARIA
Histopathology
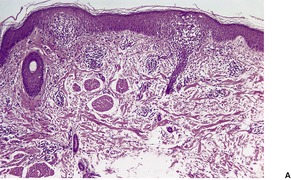
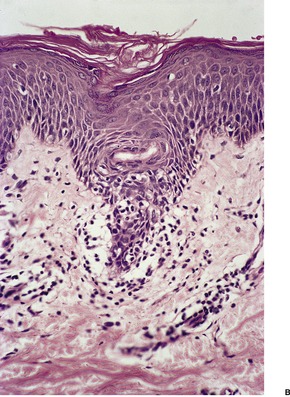
Fig. 5.7
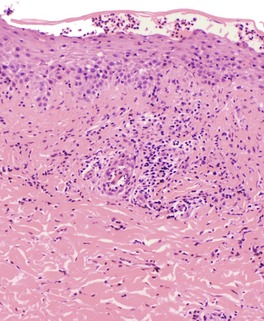
Fig. 5.8
FOLLICULAR SPONGIOSIS
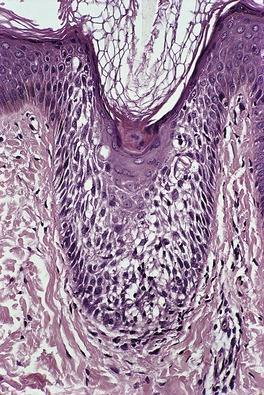
Fig. 5.9
INFUNDIBULOFOLLICULITIS
Histopathology59.61. and 63.
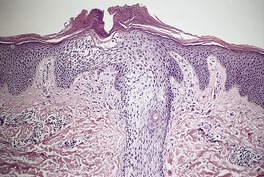
Fig. 5.10
ATOPIC DERMATITIS
Histopathology
APOCRINE MILIARIA
Histopathology
EOSINOPHILIC FOLLICULITIS
PITYRIASIFORM SPONGIOSIS
PITYRIASIS ROSEA
Treatment of pityriasis rosea
Histopathology106.114. and 115.
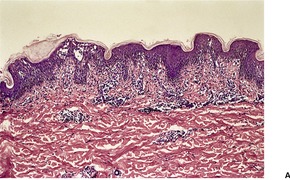
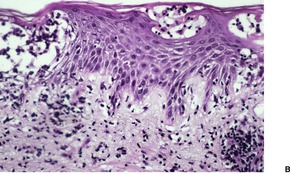
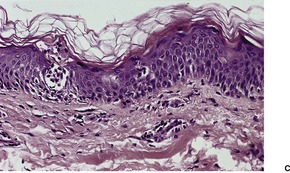
Fig. 5.11
Electron microscopy
PITYRIASIFORM DRUG REACTION
Note: Ampicillin may exacerbate pityriasis rosea.
Adalimumab
Ketotifen
Arsenicals
Lisinopril
Barbiturates
Metronidazole
BCG vaccination
Omeprazole
Benfluorex
Penicillamine
Bismuth
Pneumococcal vaccination
Captopril
Pyribenzamine
Clonidine
Smallpox vaccination
Gold
Tiopronin
Imatinib mesylate
Terbinafine
Isotretinoin
Histopathology
ERYTHEMA ANNULARE CENTRIFUGUM
Histopathology
OTHER SPONGIOTIC DISORDERS
IRRITANT CONTACT DERMATITIS
Types
Features
Acute ICD
Caused by potent irritant
Delayed acute ICD
Reaction 8–24 hours after exposure
Irritant reaction
Seen with wet work
Sensorial irritation
Sensory discomfort, no clinical lesion; lactic acid, propylene glycol are causes
Non-erythematous irritation
Clinically normal, histologically apparent; consumer products with high content of surfactants are causes
Cumulative ICD
Most prevalent; multiple subthreshold insults from weak irritants
Traumatic ICD
Follows acute skin trauma, such as acute dermatitis or a burn
Pustular and acneiform ICD
Metals, tars, oils, chlorinated agents, cosmetics
Asteatotic ICD
In elderly patients; dry skin
Frictional ICD
Confined to locations of frictional trauma; often appears psoriasiform
Treatment of hand eczema
Treatment of irritant contact dermatitis
Histopathology
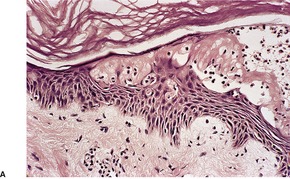
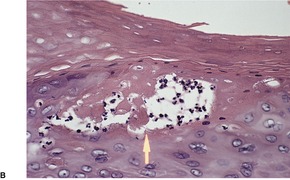
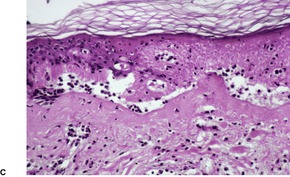
Fig. 5.12
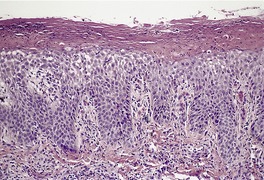
Fig. 5.13
ALLERGIC CONTACT DERMATITIS
Etiology of allergic contact dermatitis
Pathogenesis of allergic contact dermatitis
Treatment of allergic contact dermatitis
Histopathology202. and 203.
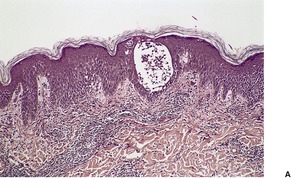
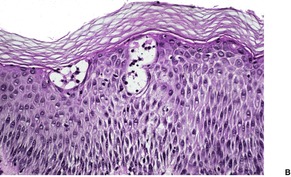
Fig. 5.14
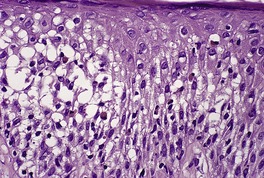
Fig. 5.15
Special variants of allergic contact dermatitis
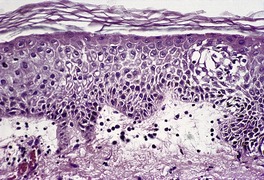
Fig. 5.16
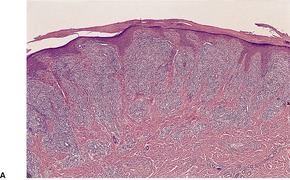
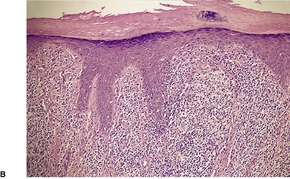
Fig. 5.17
PROTEIN CONTACT DERMATITIS
Histopathology
NUMMULAR DERMATITIS
Treatment of nummular dermatitis
Histopathology534.537. and 544.
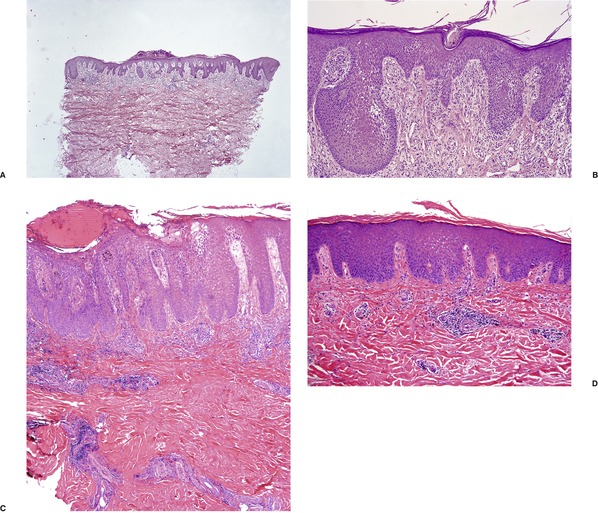
Fig. 5.18
SULZBERGER–GARBE SYNDROME
Histopathology544. and 547.
SEBORRHEIC DERMATITIS
Pityriasis amiantacea
Dandruff
Pathogenesis of seborrheic dermatitis
Treatment of seborrheic dermatitis
Histopathology595. and 596.
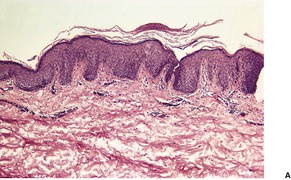
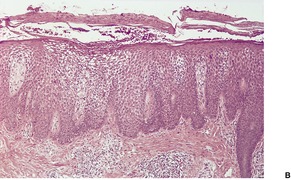
Fig. 5.19
Pityriasis amiantacea
Dandruff
ATOPIC DERMATITIS
Pathogenesis of atopic dermatitis
Treatment of atopic dermatitis
Histopathology600.859.860.861. and 862.
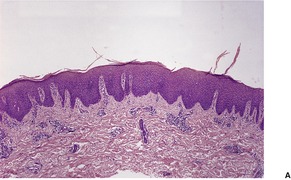
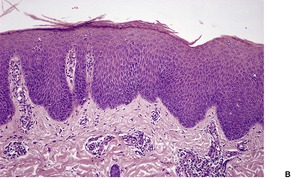
Fig. 5.20
PAPULAR DERMATITIS
Histopathology
POMPHOLYX
Histopathology884
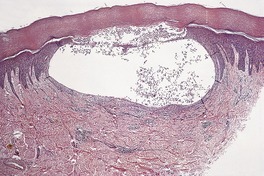
Fig. 5.21
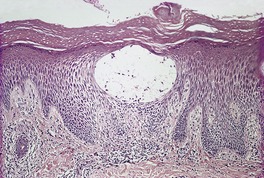
Fig. 5.22
UNCLASSIFIED ECZEMA
HYPERKERATOTIC DERMATITIS OF THE PALMS
Histopathology
JUVENILE PLANTAR DERMATOSIS
Histopathology895.899. and 900.
VEIN GRAFT DONOR-SITE DERMATITIS
STASIS DERMATITIS
Histopathology902. and 905.
AUTOECZEMATIZATION
Histopathology
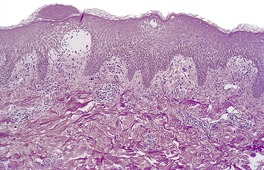
Fig. 5.23
PAPULAR ACRODERMATITIS OF CHILDHOOD
Histopathology930
SPONGIOTIC DRUG REACTIONS
*Excluded from consideration are the drugs causing neutrophilic and eosinophilic spongiosis as precursors of vesiculobullous diseases, and the chemicals (largely industry-related) producing irritant contact dermatitis.
Allergic contact dermatitis: amide anesthetics, antihistamines (topical), bacitracin, benzocaine, corticosteroids, cosmetics, doxepin, ethylenediamine, fluorouracil, formaldehyde, idoxuridine, lanoconazole, melaleuca (tea-tree) oil, mupirocin, neomycin, nickel, NSAIDs, parabens, phenylenediamine, propacetamol, propylene glycol, psoralens, vitamin E preparations
Nummular dermatitis: antimycobacterial drugs (in combination), gold, interferon alfa-2b and ribavirin, latanoprost eye drops, mercury (in dental fillings), methyldopa
Seborrheic dermatitis: arsenic, chlorpromazine, cimetidine, gold, interleukin-2, methyldopa
Pityriasis rosea-like: see Table 5.1
Systemic contact dermatitis: aminophylline, amoxicillin, ampicillin, balsam, cetuximab, chloral hydrate, cimetidine, cinnamon oil, clonidine, codeine, disulfiram, diuretics, erythromycin, gentamicin, hydroxyurea, hypoglycemic agents, immunoglobulins, isoniazid, minoxidil, neomycin, procaine, quinine, roxithromycin, sweetening agents (artificial), synergistins, thiamine, zinc in dental fillings
Non-specific spongiosis: the most common causes (leading to biopsy) are ACE inhibitors, allopurinol, atenolol, calcium channel blockers, NSAIDs (some) and thiazide diuretics (particularly compound ones such as Moduretic). Specific drugs include amlodipine, calcitonin, epoprostenol, estrogen, etanercept, fluoxetine (Prozac), gold, indomethacin, immunoglobulin infusion, infliximab, interferon-alfa with ribavirin, interleukins, lamotrigine, methadone, nifedipine, paroxetine (Aropax), phenytoin sodium, piroxicam, progesterone, smallpox vaccination, sulfasalazine, tamoxifen, and subcutaneous injection of danaparoid, GMCSF, heparin, vitamin K. Intravenous immunoglobulin and chemotherapeutic agents may also produce a spongiotic reaction
Photoallergic dermatitis: alprazolam, amlodipine, ampiroxicam, chlordiazepoxide, chlorpromazine, clofibrate, cyclamates, diphenhydramine, droxicam, fenofibrate, flutamide, griseofulvin, ibuprofen, ketoprofen, lomefloxacin, piketoprofen, piroxicam, pyridoxine, quinidine, quinine, ranitidine, sertraline, sulfonamides, tegafur, tetracyclines, thiazides, tolbutamide, triflusal
Phototoxic dermatitis (spongiosis variable; apoptosis ballooning and/or necrosis may be present): amiodarone, carbamazepine, doxycycline, dyes (some clothing), fleroxacin, non-steroidal anti-inflammatory drugs, oflaxacin, phenothiazines, retinoids, sulfonamides, tetrazepam, thiazides, thioxanthenes
Histopathology
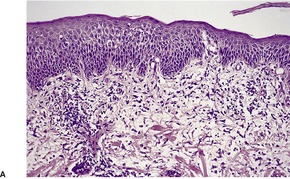
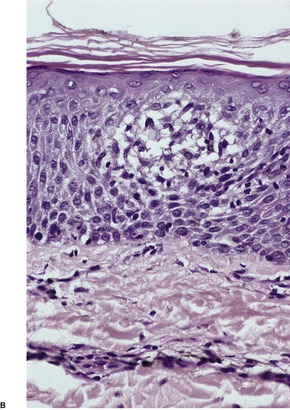
Fig. 5.24
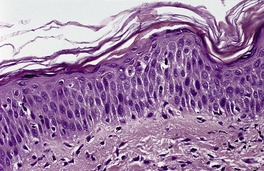
Fig. 5.25
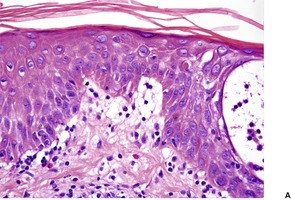
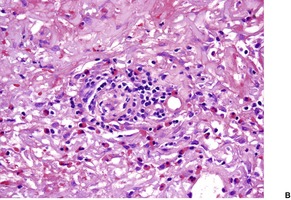
Fig. 5.26
AUTOIMMUNE PROGESTERONE DERMATITIS
Histopathology
ESTROGEN DERMATITIS
Histopathology
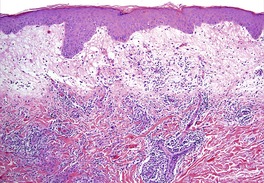
Fig. 5.27
CHRONIC SUPERFICIAL DERMATITIS
Histopathology1006. and 1009.
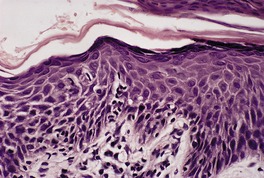
Fig. 5.28
BLASCHKO DERMATITIS
PSORIASIS
Early psoriasis/guttate psoriasis
Psoriasis of palms and soles
Erythrodermic psoriasis
Flexural psoriasis
Established psoriasis (rare, may have subtle histopathological features of glucagonoma syndrome as well)
Spongiotic psoriasis
LIGHT REACTIONS
Histopathology
DERMATOPHYTOSES
Histopathology
ARTHROPOD BITES
Histopathology
The spongiotic reaction pattern
Eosinophilic spongiosis96
Other spongiotic disorders102
Irritant contact dermatitis102
Allergic contact dermatitis104
Protein contact dermatitis107
Nummular dermatitis108
Sulzberger–Garbe syndrome108
Atopic dermatitis111
Papular dermatitis113
Pompholyx114
Unclassified eczema114
Hyperkeratotic dermatitis of the palms114
Juvenile plantar dermatosis115
Vein graft donor-site dermatitis115
Stasis dermatitis115
Autoeczematization115
Papular acrodermatitis of childhood116
Spongiotic drug reactions116
Autoimmune progesterone dermatitis117
Estrogen dermatitis119
Chronic superficial dermatitis119
Blaschko dermatitis119
Psoriasis119
Light reactions120
Dermatophytoses120
Arthropod bites120
Grover’s disease (spongiotic variant)120
Toxic shock syndrome120
PUPPP120
Pigmented purpuric dermatoses121
Pityriasis alba121
Eczematoid GVHD122
Eruption of lymphocyte recovery122
Lichen striatus122
Erythroderma122
Mycosis fungoides122
Acrokeratosis paraneoplastica122
The spongiotic tissue reaction is characterized by the presence of intraepidermal and intercellular edema (spongiosis) (Fig. 5.1). It is recognized by the widened intercellular spaces between keratinocytes, with elongation of the intercellular bridges (Fig. 5.2). 1 The foci of spongiosis may vary from microscopic in size to grossly identifiable vesicles and even bullae. Mild spongiosis is well seen in semithin sections. 2 Inflammatory cells, usually lymphocytes but sometimes eosinophils or even neutrophils, are also present. 1
The spongiotic reaction pattern. There is mild intracellular edema leading to pallor of the keratinocytes, in addition to the intercellular edema. (H & E)
The spongiotic reaction pattern. Note the elongation of the intercellular bridges resulting from the intercellular edema. Occasional eosinophils are present within the epidermis. (H & E)
The spongiotic tissue reaction is a histopathological concept and not a clinical one, although several of the many diseases with this tissue reaction have been included, in the past, in the category of ‘eczemas’. This term (derived from Greek elements which mean ‘boiling over’) has fallen into some disrepute in recent years because it lacks precision.3.4. and 5. The ‘eczemas’ all show epidermal spongiosis at some stage of their evolution, even though this has been disputed for atopic eczema. Clinically, the various spongiotic disorders may present with weeping, crusted patches and plaques, as in the so-called ‘eczemas’, or as erythematous papules, papulovesicles, and even vesiculobullous lesions. Resolving lesions and those of some duration may show a characteristic collarette of scale.
The mechanism involved in the collection of the intercellular fluid is controversial. It is generally accepted that the fluid comes from the dermis and, in turn, from blood vessels in the upper dermis. Various immunological reactions are involved in some of the diseases discussed in this chapter, but in others the etiology of this fluid extravasation from vessels remains to be elucidated. The controversy also involves the mechanism by which the dermal edema fluid enters the epidermis.6. and 7. One concept is that an osmotic gradient develops towards the epidermis, drawing fluid into it. 6 The opposing view suggests that hydrostatic pressure leads to the epidermal elimination of dermal edema. 8 The latter explanation does not satisfactorily explain the absence of spongiosis in pronounced urticarial reactions. Perhaps both mechanisms are involved to a varying degree. The spongiotic tissue reaction is a dynamic process. 9 Vesicles come and go and they can be situated at different levels in the epidermis. 9 Parakeratosis forms above areas of spongiosis, probably as a result of an acceleration in the movement of keratinocytes towards the surface, although disordered maturation may contribute. 10 Small droplets of plasma may accumulate in the mounds of parakeratosis, contributing to the appearance of the collarettes of scale mentioned above. 10
There are several categories of disease in which casual histological examination may show a simulation of the spongiotic reaction pattern: they are excluded from consideration here. 1 Diseases that present a lichenoid reaction pattern with obscurement of the dermoepidermal interface (such as pityriasis lichenoides, erythema multiforme and fixed drug eruption) or prominent vacuolar change (variants of lupus erythematosus) may show some spongiosis above the basal layer. They are not included among the diseases considered in this chapter.
Certain viral exanthems and morbilliform drug eruptions show mild epidermal spongiosis, but it is usually limited to the basal layer of the epidermis. Other viral diseases, such as herpes simplex and herpes zoster, show ballooning degeneration of keratinocytes with secondary acantholysis. Some spongiosis is invariably present but it is overshadowed by the other changes. Primary acantholytic disorders leading to vesiculation are also excluded. Mild spongiosis is seen overlying the dermal papillae in early lesions of psoriasis, but again this disease is not usually regarded as a spongiotic disorder.
The accumulation of acid mucopolysaccharides in the follicular infundibulum in follicular mucinosis may simulate spongiosis. Stains for mucin, such as the colloidal iron stain, will confirm the diagnosis, if any doubt exists.
Finally, the Pautrier microabscesses of mycosis fungoides may be simulated by the collections of mononuclear cells that sometimes accumulate in spongiotic dermatitis (Fig. 5.3). In spongiotic dermatitis, the cellular collections often assume a vase-like shape, with the lips of the vase situated at the interface between the granular and cornified layers. 11 The intraepidermal collections of mononuclear cells express CD1a, S100 protein, CD36, and CD68. They lack CD14, which is found on mature Langerhans cells. Their phenotype suggests derivation from circulating monocytes and differentiation into mature Langerhans cells. 12
A Pautrier simulant in a spongiotic dermatitis. There were numerous Langerhans cells within the vesicle. (H & E)
There are five special patterns of spongiosis which can be distinguished morphologically from the more usual type. These special patterns are neutrophilic spongiosis, in which there are numerous neutrophils associated with epidermal spongiosis, eosinophilic spongiosis, characterized by the presence of numerous eosinophils within the spongiotic foci, miliarial spongiosis, in which the edema is centered on the acrosyringium, follicular spongiosis, in which there is involvement of the follicular infundibulum, and pityriasiform spongiosis, in which there are spongiotic microvesicles containing lymphocytes ± Langerhans cells. Sometimes serial sections are required before it is appreciated that the spongiosis is related to the acrosyringium or acrotrichium. Diseases in these special categories will be discussed first, followed by a description of the more usual type of spongiotic disorders. The histopathological features of the pityriasiform and other spongiotic diseases are included in Table 5.6 at the end of the chapter.
Neutrophilic spongiosis is characterized by the presence of neutrophils within spongiotic foci in the epidermis (Fig. 5.4). The term spongiform pustular dermatitis can be used for a severe form of neutrophilic spongiosis in which pustules can be seen clinically and histologically. Subcorneal pustules are excluded from this category. Ackerman states that neutrophils are absent in ‘authentic’ spongiotic dermatitides, 13 but a case can be made for including the following conditions in this histological pattern:
• pustular psoriasis
• prurigo pigmentosa
• Reiter’s syndrome
• pemphigus foliaceus
• IgA pemphigus
• herpetiform pemphigus
• infantile acropustulosis
• acute generalized exanthematous pustulosis
• palmoplantar pustulosis
• staphylococcal toxic shock syndrome
• neisserial infections
• dermatophytoses
• candidosis
• beetle (Paederus) dermatitis
• pustular contact dermatitis
• glucagonoma syndrome
• amicrobial pustulosis associated with autoimmune diseases
• erosive pustular dermatosis of the legs
• amicrobial pustulosis of the folds
• periodic fever syndromes.
Neutrophilic spongiosis characterized by the presence of neutrophils within spongiotic vesicles. (H & E)
Reiter’s syndrome (see p. 83) shares histological features with pustular psoriasis. It will not be considered further. If spongiosis occurs in pemphigus foliaceus it is usually of eosinophilic type. Neutrophilic spongiosis has been reported in a case that evolved into an atypical pemphigus phenotype. 14 In infantile acropustulosis (see p. 131) there are variable numbers of eosinophils admixed with the neutrophils. In palmoplantar pustulosis (see p. 133) large vesicles are the dominant feature with only some neutrophilic spongiosis at the edges. This tissue reaction can also be seen in the staphylococcal toxic shock syndrome (see p. 550) and in infections with Neisseria sp. (see p. 556). Pustular contact dermatitis is considered later in this chapter (see p. 107). The glucagonoma syndrome is considered in Chapter 18 (see p. 489). Amicrobial pustulosis associated with autoimmune diseases and herpetiform pemphigus are discussed in Chapter 6 (see pp. 134 and 129 respectively). Erosive pustular dermatosis of the legs is discussed in Chapter 6 (see p. 134). Amicrobial pustulosis of the folds, and the periodic fever syndromes are included in Chapter 8 (see pp. 219 and 219 respectively).
Prurigo pigmentosa is an inflammatory dermatosis characterized by the sudden onset of pruritic erythematous papules, usually involving the trunk and neck, that coalesce to form reticulated, mottled patches. 15 Vesicles and bullae are uncommon. Because it resolves leaving mottled or reticulate hyperpigmentation it is discussed further in Chapter 10, page 296.
In the established papular phase there is variable spongiosis, acanthosis, exocytosis of lymphocytes, and a few neutrophils with isolated apoptotic keratinocytes. In early stages of the disease there is neutrophilic spongiosis with some apoptotic keratinocytes at all levels of the epidermis. There is a mild superficial perivascular infiltrate of lymphocytes and neutrophils and a few eosinophils in the earlier stages. Pigment incontinence is a conspicuous feature of late lesions.
IgA pemphigus is a vesiculobullous disease (see p. 130) with a variable expression, accounting for the many titles applied to this condition in the past. There are subcorneal and/or intraepidermal pustules with usually only mild acantholysis. IgA is deposited in the epidermis in an intercellular position.
Acute generalized exanthematous pustulosis is a rapidly evolving pustular eruption (see p. 132), usually associated with the ingestion of drugs, particularly antibiotics. There are subcorneal and superficial intraepidermal pustules. Subepidermal pustules are sometimes present with prominent neutrophil exocytosis and neutrophilic spongiosis.
Neutrophilic spongiosis can be found with dermatophyte infection and also with the yeast Candida. The presence of neutrophils in the epidermis and/or overlying stratum corneum should always lead to the performance of a PAS stain.
Vesicular dermatitis, characterized by areas of neutrophilic spongiosis, results from contact with various beetles (order Coleoptera).16.17. and 18. Bullae and small pustules may even result. The term Paederus dermatitis is used for the reaction produced by the genus Paederus, of which there are several hundred species capable of producing a form of acute irritant contact dermatitis. 17 The irritant substance is pederin, a highly toxic alkaloid produced by members of this genus. Localized erythema occurs first, followed by blisters after 2–4 days, associated with increasing pain. 16 Lesions are commonly linear due to crushing of the beetle on the skin, followed by its wiping off the skin. The delay in the appearance of the lesions may lead to lack of recognition of the causal event.
Early lesions show neutrophilic spongiosis leading to vesiculation and eventual reticular necrosis of the epidermis. This is followed by confluent epidermal necrosis, usually with a surviving layer of suprabasal cells. Scattered acantholytic cells may be present. The large number of intraepidermal neutrophils, combined with areas of confluent necrosis and reticular degeneration, are characteristic. Older lesions show irregular acanthosis and pallor of superficial keratinocytes, with overlying parakeratotic scale containing a neutrophil exudate. 16
A similar spongiotic and vesicular dermatitis, with the addition of vasculitis, has been produced by the hide beetle, Dermestes peruvianus. 19
Eosinophilic spongiosis is a histological reaction pattern characterized by the presence of epidermal spongiosis associated with the exocytosis of eosinophils into the spongiotic foci. 20 Microabscesses, containing predominantly eosinophils, are formed.
Eosinophilic spongiosis is found in a heterogeneous group of dermatoses, 21 most of which are considered elsewhere. It can be seen in the following conditions:
• pemphigus (precursor lesions)
• pemphigus vegetans
• herpetiform pemphigus
• bullous pemphigoid
• cicatricial pemphigoid
• herpes gestationis
• idiopathic eosinophilic spongiosis
• eosinophilic, polymorphic, and pruritic eruption
• allergic contact dermatitis
• atopic dermatitis
• arthropod bites
• eosinophilic folliculitis (Ofuji’s disease)
• incontinentia pigmenti (first stage)
• drug reactions
• ‘id’ reactions
• Still’s disease22
• Wells’ syndrome.
Eosinophilic spongiosis may occur in the preacantholytic stage of both pemphigus foliaceus and pemphigus vulgaris.20.23.24. and 25. In these early stages, direct immunofluorescence demonstrates the presence of IgG in the intercellular areas of the epidermis. 23 In those patients whose disease evolves into pemphigus foliaceus, the initial clinical presentation may resemble dermatitis herpetiformis.24. and 26. Some of these cases have been reported in the literature as herpetiform pemphigus.27. and 28.
The pattern is that described for eosinophilic spongiosis (Fig. 5.5). Acantholysis and transitional forms between eosinophilic spongiosis and the usual histological findings in pemphigus may be present.
Eosinophilic spongiosis as a precursor of pemphigus foliaceus. (H & E)
Eosinophils are often prominent within the vesicles of pemphigus vegetans. Acantholysis, epidermal hyperplasia, and the absence of spongiosis adjacent to the suprabasal vesicles usually allow the diagnosis of pemphigus vegetans to be made.
Eosinophilic spongiosis is an uncommon finding in the urticarial stage of bullous pemphigoid and in erythematous patches adjacent to characteristic bullae in later stages of the disease. 29 In one case, the eosinophilic spongiosis preceded the diagnosis of bullous pemphigoid by 13 years. 30 There is usually a prominent dermal infiltrate of eosinophils, and IgG is demonstrable along the basement membrane zone.
Eosinophilic, polymorphic, and pruritic eruption, associated with the use of radiotherapy, particularly for carcinoma of the breast, has not been well characterized.33.34. and 35. Similar cases have been reported in the past, often without histological confirmation, under several different designations, including erythema multiforme and bullous pemphigoid after radiation therapy. 33 The rash is widespread, polymorphic, and intensely pruritic, commencing during radiotherapy and lasting several weeks or months. The lesions are usually erythematous papules, measuring 3–10 mm in diameter. Wheals, vesicles, and tense subepidermal blisters are less common. The eruption often develops in areas well away from the radiated area. 36
The variable histological appearances reflect the polymorphic nature of the rash. There is usually spongiosis with focal spongiotic vesiculation. There may be some acanthosis in lesions of longer duration and secondary changes of rubbing and scratching. The dermal infiltrate is usually superficial and deep and of moderate severity. Extension into the subcutis sometimes occurs. Eosinophils are always present. There is usually some eosinophilic spongiosis; an eosinophilic panniculitis is much less common. If bullae are present, they usually resemble bullous pemphigoid. There are no features of erythema multiforme, despite the earlier publications attributing this condition to erythema multiforme.
Eosinophilic spongiosis may be seen in allergic contact dermatitis (see p. 104).
Eosinophilic spongiosis is occasionally seen in the reaction to the bite of certain arthropods, particularly the scabies mite (see p. 656).
In eosinophilic folliculitis (Ofuji’s disease – see p. 403) the eosinophilic spongiosis involves the follicular infundibulum; sometimes the immediately adjacent epidermis is also involved.
In the first stage of incontinentia pigmenti (see p. 297) there is prominent exocytosis of eosinophils into the epidermis and foci of eosinophilic spongiosis (Fig. 5.6). Occasional dyskeratotic keratinocytes may also be present.
Eosinophilic spongiosis in the first stage of incontinentia pigmenti. (H & E)
Miliarial spongiosis is characterized by intraepidermal edema centered on the acrosyringium. It is characteristic of the various clinical forms of miliaria.
The miliarias are a clinically heterogeneous group of diseases which occur when the free flow of eccrine sweat to the skin surface is impeded. Three variants of miliaria have been defined according to the depth at which this sweat duct obstruction occurs.
Miliaria crystallina (miliaria alba), which results from superficial obstruction in the stratum corneum, is characterized by asymptomatic, clear, 1–2 mm vesicles which rupture easily with gentle pressure. 37 Congenital onset is exceedingly rare.38. and 39. Onset in the first week of life is not uncommon. 40 It has also been reported in adult patients in an intensive care setting. 41 It may have been caused by drugs producing enhanced α-adrenergic stimulation of sweat gland myoepithelium. 41 Isotretinoin can also cause miliaria crystallina. 41 It is a self-limited condition that resolves without complications over a period of several days.
Miliaria rubra (prickly heat) consists of small, discrete, erythematous papulovesicles with a predilection for the clothed areas of the body. 42 The lesions are often pruritic. In severe cases, with recurrent crops of lesions, anhidrosis may result. 43 Occasionally, pustular lesions (miliaria pustulosa) may coexist. Both miliaria rubra and pustular miliaria rubra have been reported in infants and children with type I pseudohypoaldosteronism.44.45. and 46. Miliaria rubra can also occur in Morvan’s syndrome, a form of generalized myokymia (OMIM 160120). 47
Miliaria profunda refers to the development of flesh-colored papules resembling gooseflesh, associated with obstruction of the sweat duct near the dermoepidermal junction.48. and 49. It usually follows severe miliaria rubra and is associated with anhidrosis. A case has been reported in which large white plaques with an erythematous border were present. 50 The lesions expanded centrifugally until they were several centimeters or more in diameter. They were localized to sites at which occlusive tape had been applied. 50
Although it has been presumed since the 19th century that obstruction of the eccrine duct is involved in the pathogenesis of the miliarias, the nature of this obstruction and its etiology have been the subject of much debate. 48 The first demonstrable histological change is the accumulation of PAS-positive, diastase-resistant material in the distal pore, 48 although this has not always been found. 51 This material has been designated ‘extracellular polysaccharide substance (EPS)’. 52 It is likely that there is an earlier stage of obstruction, which cannot be demonstrated in tissue sections. After several days, a keratin plug forms as part of the repair process, leading to further obstruction of the duct, often at a deeper level. Various factors may contribute to the initial duct obstruction.53. and 54. These include changes in the horny layer related to excess sweating, the presence of sodium chloride in more than isotonic concentration, 51 and lipoid depletion. In many cases there is an increase in the number of resident aerobic bacteria, particularly cocci.48.55.56. and 57. Certain strains of Staphylococcus epidermidis produce the PAS-positive material known as EPS (see above) and these organisms may play a central role in the pathogenesis of miliaria. 52 Miliaria have also developed at the site of previous radiotherapy; there was associated keratotic plugging of the eccrine orifices. 58
In miliaria crystallina there is a vesicle within or directly beneath the stratum corneum. There is often a thin, orthokeratotic layer forming the roof of the vesicle and a basket-weave layer of keratin in the base. A PAS-positive plug may be seen in the distal sweat pore.
Miliaria rubra is characterized by variable spongiosis and spongiotic vesiculation related to the epidermal sweat duct unit and the adjacent epidermis (Fig. 5.7). There is a small number of lymphocytes in the areas of spongiosis. An orthokeratotic or parakeratotic plug may overlie the spongiosis. 42 Sometimes there is edema in the papillary dermis adjacent to the point of entry of the eccrine duct into the epidermis. A mild lymphocytic infiltrate is usually present in this region. If the edema is pronounced, leading to subepidermal vesiculation, then miliaria profunda is said to be present. Miliaria pustulosa is characterized by neutrophils beneath the stratum corneum and/or in the epidermal sweat duct (Fig. 5.8).
Miliaria rubra. (A) The spongiosis is related to the acrosyringium. (B) There is edema in the wall of the eccrine duct as it enters the epidermis and also in the adjacent papillary dermis. (H & E)
Miliaria pustulosa. The pustule often extends well beyond the limits of the involved acrosyringium, making the diagnosis difficult. (H & E)
Less commonly, there is only slight spongiosis in the region of the acrosyringium in miliaria rubra associated with dilatation of the terminal eccrine duct. 42 It should be remembered that not all eccrine ducts are involved.
The secretory acini show few changes in the miliarias. 42 They may be mildly dilated. Often there is slight edema of the connective tissue between the secretory units. Lymphocytes are not usually present, unless there is a prominent inflammatory cell infiltrate elsewhere in the dermis.
Follicular spongiosis refers to the presence of intercellular edema in the follicular infundibulum (Fig. 5.9). It occurs in a limited number of circumstances:
• infundibulofolliculitis
• atopic dermatitis (follicular lesions)
• apocrine miliaria
• eosinophilic folliculitis.
Follicular spongiosis. The patient had follicular lesions on the trunk as a manifestation of atopic dermatitis. (H & E)
Infundibulofolliculitis, also known as disseminate and recurrent infundibulofolliculitis, presents as a follicular, often pruritic, papular eruption with a predilection for the trunk and proximal parts of the extremities of young adult males.59.60.61. and 62. It occurs almost exclusively in black patients. Although the lesions resemble those seen in some cases of atopic dermatitis, the individuals studied so far have not been atopic. 63
There is spongiosis of the follicular infundibulum with exocytosis of lymphocytes (Fig. 5.10). A few neutrophils are sometimes present. There is widening of the follicular ostium and focal parakeratosis of the adjacent epidermis. Occasional follicles contain a keratin plug. 63The follicular infundibulum is often hyperplastic. There is usually a slight infiltrate of lymphocytes around the follicles and around the blood vessels in the superficial part of the dermis. Mast cells may be increased.
Infundibulofolliculitis. There is follicular spongiosis, focal parakeratosis and a mild inflammatory cell infiltrate in the dermis. (H & E)
Some patients with atopic dermatitis develop small follicular papules, often on the trunk.
There is spongiosis of the follicular infundibulum with exocytosis into this region of the epidermis. Usually no neutrophils are present. The adjacent epidermis may show mild acanthosis and sometimes focal parakeratosis. The histopathology resembles that seen in infundibulofolliculitis.
Apocrine miliaria (Fox–Fordyce disease) presents as a chronic papular eruption, usually limited to the axilla (see p. 436). It results from rupture of the intra-infundibular portion of the apocrine duct.
Serial sections may be required to demonstrate the spongiosis of the follicular infundibulum adjacent to the point of entry of the apocrine duct. There may be a few neutrophils in the associated inflammatory response. Periductal foam (xanthoma) cells are often present.
Eosinophilic folliculitis (Ofuji’s disease) is characterized by eosinophilic spongiosis centered on the follicular infundibulum. It is discussed in detail on page 403.
Pityriasiform spongiosis is characterized by the presence of microvesicles within areas of spongiosis that contain lymphocytes, histiocytes, and Langerhans cells. It is a distinctive pattern when well developed. It is seen in the following conditions:
• pityriasis rosea
• pityriasiform drug reaction
• erythema annulare centrifugum
• nummular dermatitis (some cases)
• lichen striatus (uncommon).
The spongiosis in miliaria may mimic pityriasiform spongiosis but the vesicles are often larger, and they are always related to an acrosyringium. The ‘inverted flask’-like lesions sometimes seen in allergic contact dermatitis are better defined microvesicles, with a different shape to pityriasiform lesions. They also contain a predominance of Langerhans cells.
The various diseases will be discussed in order, but nummular dermatitis (see p. 108), and lichen striatus (see p. 45) are considered in more detail elsewhere.
Pityriasis rosea is a common, acute, self-limited dermatosis in which oval, salmon-pink, papulosquamous lesions develop on the trunk, neck and proximal extremities. 64 Lesions often follow the lines of skin cleavage, giving a ‘Christmas tree’ pattern. 65 A scaly plaque 2–10 cm in diameter, the ‘herald patch’, may develop on the trunk 1–2 weeks before the other lesions. Pityriasis rosea has been reported at all ages, 66 but the majority of patients are between 10 and 35 years. 67 Clinical variants include those with acral68 or facial involvement, 66 oral lesions, 69 a unilateral or local distribution,70. and 71. or the presence of pustular, purpuric or vesicular lesions.64.72.73.74. and 75. Pityriasis rosea developing in the first 15 weeks of pregnancy is associated with premature delivery and miscarriages. 76
As atypical cases of pityriasis rosea are fairly common,77. and 78. Chuh has drawn up a list of diagnostic criteria for pityriasis rosea.79. and 80.Essential features for the diagnosis include: (i) discrete circular or oval lesions; (ii) scaling on most lesions; 81 and (iii) peripheral collarette scaling with central clearance of at least two lesions. Optional clinical features of which one must also be present include: (i) truncal and proximal limb distribution, with less than 10% of lesions distal to the mid-upper arm and mid thigh; (ii) distribution of most lesions along the ribs; and (iii) a herald patch appearing at least 2 days before the generalized eruption. 79 Interestingly, histopathological features were not added to the criteria ‘because they are non-specific in PR’. 79 Pityriasis rosea must be distinguished from secondary syphilis.79. and 82. Ackerman has proposed that pityriasis rosea and erythema annulare centrifugum are clinical variations of a single pathological process, and that pityriasis rosea gigantea is pityriasis rosea concurrent with erythema annulare centrifugum. 83
The etiology is unknown, but an infectious etiology, particularly a virus, has long been suspected. This is supported by a history of a preceding upper respiratory tract infection in some patients, 84 occasional involvement of close-contact pairs, 67 case clustering,85. and 86. modification of the disease by the use of convalescent serum or erythromycin,74. and 87. and the development of a pityriasis rosea-like eruption in some cases of infection by ECHO 6 virus, enterovirus, or Mycoplasma.64. and 88. There has been recent interest in the role of human herpesvirus-6 (HHV-6) and -7 (HHV-7) in the etiology of pityriasis rosea. While HHV-6 and HHV-7 may play a role in some patients,89.90.91.92. and 93. the low detection rate of HHV-7 DNA sequences argues against a causative role for this virus.94.95.96.97. and 98. In the case of HHV-6, reactivation of the virus during the early stages of the disease might explain its detection in some cases. 99 Herpesvirus-like particles were detected in lesional skin in 71% of patients with pityriasis rosea in one study. 100 Pityriasis rosea is not associated with HHV-8 infection, 101 or with HSV-1 or HSV-2 infection. 102 Particles resembling togavirus or arenavirus have been found on electron microscopy of a herald patch, 103 suggesting that this might be the inoculation site. No virus has ever been cultured. 104 Immunological reactions, 105 particularly cell-mediated, have also been regarded as important.106. and 107. Certain HLA subtypes may confer a susceptibility to the disease in certain races. 108
A pityriasis rosea-like eruption has also been recorded as a complication of graft-versus-host reaction, following bone marrow transplantation, 109 and in patients with acute myeloid leukemia110 or Hodgkin’s disease. 78 A long-lasting pityriasis rosea-like eruption has been described in association with AIDS. 82 The occurrence of a pityriasis rosea-like eruption in a patient with indeterminate cell histiocytosis may have resulted from an isotopic response in healed lesions of pityriasis rosea. 65
It is debatable whether active intervention is warranted to modify the disease course. 111 Patients should be reassured that the rash, if left alone, should resolve spontaneously within 4–8 weeks. 82 The quality of life in children with pityriasis rosea is minimally affected. 111 A double-blind placebo-controlled study reported a benefit of erythromycin. 87 A recent study using high-dose acyclovir (aciclovir) produced much earlier clearance of lesions compared with a placebo group. 112 It has most effect when used as early as possible in the course of the disease. There is insufficient evidence to support the use of UV phototherapy. 82 Corticosteroids have been used in severe cases, but they may even exacerbate the disease. 82 Ampicillin, just as in infectious mononucleosis, may exacerbate the disease producing more lesions, an abnormal distribution of lesions, and a more prolonged course. 113
Although the lesions are clinically papulosquamous, microscopy shows a spongiotic tissue reaction. The histopathological features are not pathognomonic, although in most cases they are sufficiently characteristic to allow the diagnosis to be made, even without a clinical history. The epidermis often has a vaguely undulating appearance. There is usually focal parakeratosis, sometimes with the formation of parakeratotic mounds. Sometimes these mounds partly lift from the epidermis giving a tilted appearance to the mound. 116 There is a diminution of the granular layer and focal spongiosis of pityriasiform type with lymphocyte exocytosis (Fig. 5.11). Small spongiotic vesicles, sometimes simulating Pautrier microabscesses because of the aggregation of lymphocytes within them, are a characteristic feature; they are present in most cases if several levels are examined. Dyskeratotic cells may be seen at all levels of the epidermis; they are more common in the herald patch. Apoptotic keratinocytes are present in the lower epidermis in lesions undergoing involution. Multinucleate epidermal cells are uncommon. Focal acantholytic dyskeratosis has been reported once. 117
Pityriasis rosea. (A) A typical case with pityriasiform spongiosis. (B) A more ‘florid’ case with several foci of pityriasiform spongiosis and subepidermal edema. (C) In this case the dermal inflammation is quite mild. (H & E)
The papillary dermis shows some edema and sometimes homogenization of collagen. There may be some melanin incontinence. Red cell extravasation is common in the upper dermis and may extend into the lower layers of the epidermis. There is a mild to moderate lymphohistiocytic infiltrate in the upper dermis, with some eosinophils in the infiltrate in older lesions.
Ultrastructural examination has confirmed the presence of dyskeratotic cells in some patients. 118 These cells show aggregation of tonofilaments, some cytoplasmic vacuoles, and intracytoplasmic desmosomes. 119 Cytolytic degeneration of keratinocytes adjacent to Langerhans cells has been reported in a herald patch. 120 Virus-like particles have been seen in several studies.100. and 118.
Pityriasiform (pityriasis rosea-like) drug reaction presents as an eruption that resembles to varying degrees pityriasis rosea, usually within weeks of commencing one of the drugs listed in Table 5.1. There are usually fewer lesions in drug-related cases than in pityriasis rosea itself. They are often larger than in pityriasis rosea with scaling involving the entire lesion. 64 Drug-related cases usually lack a herald patch. 121 Furthermore, oral lesions are more common, as is the development of postinflammatory hyperpigmentation. 82
Many drugs have been implicated in the etiology of these eruptions, 64 including gold, bismuth, arsenicals, ketotifen, clonidine, barbiturates, omeprazole, 121 tiopronin, terbinafine, benfluorex, 122pyribenzamine, penicillamine, isotretinoin, metronidazole, 123 captopril, 124 lisinopril, 125 imatinib mesylate, 126 and adalimumab. 127 The latter case cleared 2 weeks after the cessation of the drug, making this diagnosis more likely than pityriasis rosea associated with lowered immunity from the drug. 127
There is pityriasiform spongiosis with variable resemblance to pityriasis rosea itself. Eosinophils are invariably present, but they may also be found in later lesions of pityriasis rosea. Apoptotic keratinocytes are features in both conditions, but only in later lesions of pityriasis rosea. Subepidermal edema may also be present in drug-related cases.
Erythema annulare centrifugum is a pityriasiform dermatosis that in some stages of its evolution is indistinguishable from pityriasis rosea. There are one or more annular, erythematous lesions which may spread outwards or remain stationary. A fine scale is sometimes present inside the advancing edge giving a so-called ‘trailing scale’ (see p. 229). The annular erythema of Sjögren’s syndrome is sometimes spongiotic. 129
Until recently, erythema annulare was included with other erythemas in the lymphocytic vasculitides, although this was always regarded as unsatisfactory. The detailed studies of Weyers and colleagues delineated the histological appearances of this entity. 130 For various reasons, the main discussion of this entity remains in Chapter 8, page 229.
A biopsy through the advancing edge will show focal spongiosis and parakeratosis with an underlying superficial perivascular infiltrate of lymphocytes, often with a ‘coat-sleeve’ appearance. There are some similarities to pityriasis rosea, although a biopsy taken at right angles to the edge of erythema annulare centrifugum will show a much more localized process. A ‘variant’ without spongiosis and with a deep as well as superficial inflammatory infiltrate also occurs. This is probably a different entity. 130
Most of the other diseases in which the spongiotic reaction pattern occurs show spongiosis distributed randomly through the epidermis with no specific localization to the acrosyringium or follicular infundibulum, which indeed are often spared.
It is sometimes quite difficult to make a specific histopathological diagnosis of some of the diseases in this category. Often a diagnosis of ‘spongiotic dermatitis consistent with …’ is as specific as one can be.
Miscellaneous diseases that may sometimes show epidermal spongiosis include Still’s disease, 131 prurigo pigmentosa (it is often neutrophilic in type – see p. 296), and dermal hypersensitivity reaction (see p. 942). The spongiosis is rarely of eosinophilic type in adult-onset Still’s disease. 22
Irritant contact dermatitis is an inflammatory condition of the skin produced in response to the direct toxic effect of an irritant substance. 132 It accounts for approximately 80% of occupational skin diseases. 133 The most commonly encountered of these irritants include detergents, solvents, acids, and alkalis.132.134. and 135. Other agents include wool fibers, 136 fiberglass,136.137. and 138. air bags, 139 topical anesthetic agents, 140 sunscreen preparations, 141 propylene glycol, 142 and plants, 143 particularly the milky sap of members of the family Euphorbiaceae.144. and 145. Garlic applied to the skin may produce a severe irritant dermatitis resembling a chemical burn. 146 Even airborne substances in droplet, particulate, or volatile form can cause this type of dermatitis. 147 Chemically induced irritant contact dermatitis is a leading cause of occupational disease with important economic consequences; 148 accordingly protective creams are being developed and evaluated to assist in the control of this important problem.149. and 150. Protective gloves can also be used, but selection of gloves made of appropriate material is necessary to avoid exacerbation of the original process. 151
Our knowledge of irritant contact dermatitis is limited in spite of the fact that it is more common than allergic contact dermatitis (although this has been challenged recently), from which it may be difficult to distinguish.152. and 153. Irritant reactions vary from simple erythema to purpura, eczematous reactions, vesiculobullous lesions, and even epidermal necrosis with ulceration. Lesions are often more glazed than allergic reactions and subject to cracking, fissuring, and frictional changes. 134 Irritant reactions occur at the site of contact with the irritant; in the case of airborne spread, the eyelids are a common site of involvement.147. and 154. Pustular reactions have been reported with heavy metals, halogens and other substances.155. and 156. These responses are assumed to be irritant in type. Acute ulceration is a severe reaction that may follow contact with alkalis, including cement.157. and 158. Ten clinical subtypes of irritant contact dermatitis were listed in the review of this topic by Rosemary Nixon and colleagues in 2008. 153 They are listed in Table 5.2.
Chronic hand dermatitis (eczema) has many subtypes. Storrs, based on her extensive experience, recognizes six categories: (1) allergic, (2) irritant, (3) nummular, (4) dyshidrotic, (5) chronic vesicular,159. and 160. and (6) hyperkeratotic. 161 Hybrid forms with overlapping features of different types are common. A scoring system for the severity of hand eczema has been proposed. 162 Patch testing is vital in the diagnostic work-up of patients with hand dermatitis.161. and 163. The most common allergens involved in one series of patients with allergic contact dermatitis of the hands were preservatives, metals, fragrances, topical antibiotics, and rubber additives. 163 Wet work and genetic factors also play a role. 164 Fungal infection (tinea manuum) should also be excluded. The role of an atopic diathesis in the etiology of irritant hand dermatitis is mentioned below.
This can be difficult. Potential allergens should be identified and avoidance measures taken. Topical steroid ointments and tars are the mainstays of therapy. 161 A recent trial found that clobetasol combined with zinc sulfate cream was more effective than clobetasol alone. 165 Salicyclic acid (5%) can be added for the hyperkeratotic variant. Short courses of systemic steroids may be required for pompholyx and the chronic vesicular form of the disease. 161 Recapitulating the natural lipid barrier of the epidermis with topical ceramides may be a useful adjunct in therapy but, rarely, they may be a cause of a contact dermatitis. 161 An overview of 90 studies on the treatment of hand eczema was published in 2004. 166 It concluded that even the randomized controlled trials included in their review were not adequate to guide clinical practice. 166 About 5% of cases of hand eczema are resistant to all forms of treatment, resulting in long sick-leave periods, sick pensions, and changes of occupation.167. and 168. A recent trial of cases refractory to topical corticosteroids found that clearing of the severe chronic hand eczema occurred with oral alitretinoin (9-cis retinoic acid). 169 Treatment of irritant contact dermatitis at other sites is considered further below.
Irritant contact dermatitis appears to have a predilection for the vulva. 170 Irritating substances include antiseptics, douches, lubricants, contraceptives, and sanitary pads. 170 Friction and overheating also play a role in exacerbating any inflammatory process. The histological appearance often mimics that of allergic contact dermatitis. 170
A special variant of irritant contact dermatitis is seen in association with urostomies. Encopresis is another cause of this disorder. 171 Eventually pseudoverrucous papules and nodules may develop in the perianal region. 172 Other stomas may also be associated with irritant reactions. 173 Granuloma gluteale infantum (a misnomer because there are no granulomas) is a diaper-related irritant dermatitis in which Candida albicans may also play a role (see p. 589). 174 It is now thought that granuloma gluteale, pseudoverrucous papules, and Jacquet’s erosive diaper dermatitis are parts of a disease spectrum that may be multifactorial in origin, but with a primary irritant etiology. 175 A similar erosive papulonodular dermatosis has resulted from the topical use of benzocaine. 175
Susceptibility to irritant dermatitis is variable, although approximately 15% of the population have heightened sensitivity of their skin which appears to result from a thin, permeable stratum corneum. 152 There are differences in skin sensitivity in different regions of the body.176. and 177. Atopic individuals are more susceptible, 178 and both irritants and an atopic diathesis have been incriminated in the etiology of occupational dermatitis of the hands.152.179.180. and 181. Loss-of-function polymorphisms in the filaggrin gene (FLG) are associated with an increased susceptibility to chronic irritant contact dermatitis. 182 African American skin appears to have superior barrier function to irritants than white skin. 133 Cumulative irritancy, in which multiple subthreshold damage to the skin occurs, may also be seen with agents in cosmetics, for example.134.148. and 183. Delayed irritancy is another variant of irritant contact dermatitis in which the clinical changes are not manifest until 8–24 hours after the exposure. 184 Susceptibility to irritants is also more common in the winter months, apparently as a result of changes in the barrier functions of the stratum corneum. 185 Low humidity due to air-conditioning can result in an irritant contact dermatitis of the face and neck in office workers due to drying out of the skin. 186 Physical friction is also an important contributor to contact dermatitis, particularly the irritant type. 187 Minor frictional trauma may cause enhanced penetration of allergens. 187
Irritants may act in several different ways. They may remove surface lipids and water-holding substances (as with surfactants contained in household cleaning products),188. and 189. damage cell membranes or denature epidermal keratins. 190 They may have a direct cytotoxic effect. Some irritants are also chemotactic for neutrophils in vitro, while others may lead to the liberation of cytokines and other inflammatory mediators; tumor necrosis factor has been implicated as an important cytokine in irritant reactions. 183 The pathogenesis of irritant contact dermatitis continues to be poorly understood, although evidence is emerging that a very complex reaction pattern occurs, involving immunoregulatory processes.153.191. and 192. Irritancy may also lead to allergic contact dermatitis. 193
Cytokine expression in allergic and irritant contact reactions differs surprisingly little. 194 They are similar at 72 hours after the application of the respective experimental contactant although, at 6 hours, the irritant reaction expresses higher levels. 195 Cytokines that are increased include IL-1α, IL-1β, IL-2, IL-6, IFN-γ, and TNF-α.194. and 195. The chemokine CCL21, produced by dermal lymphatic endothelial cells, is up-regulated in irritant contact dermatitis. 153 It facilitates the migration of naive T lymphocytes, resulting in a skin inflammatory response. Apoptosis of epidermal Langerhans cells is produced by some irritants but not others. 196
Avoiding exposure to irritants, the use of protective equipment, and the use of moisturizing creams are the bases of treatment. 153 A systematic review of the treatment and prevention of irritant contact dermatitis was published in 2005. 197 It found that barrier creams containing dimethicone or perfluoropolyethers, cotton liners, and softened fabrics prevent irritant contact dermatitis. Lipid-rich moisturizers both prevent and treat this condition. 197 Topical corticosteroids and macrolide immunomodulators have been used in the treatment of irritant contact dermatitis but the systematic review, already mentioned, made no recommendation as to their use. 197 Recent work suggests that topical corticosteroids may compromise barrier function. 153 Cumulative irritant contact dermatitis has been treated by phototherapy. 153
The changes observed in irritant contact dermatitis vary with the nature of the irritant, including its mode of action and its concentration.190. and 198. A knowledge of these factors helps to explain the conflicting descriptions in the literature. 199 Furthermore, many of the histopathological studies have been performed on animals, which are particularly liable to develop epidermal necrosis and dermoepidermal separation with neutrophil infiltration when exposed to high concentrations of irritants.198. and 200. In humans, high concentrations of an irritant will produce marked ballooning of keratinocytes in the upper epidermis with variable necrosis ranging from a few cells to confluent areas of the epidermis.201.202. and 203. Neutrophils are found in the areas of ballooning and necrosis, and mild spongiosis is also present in the adjacent epidermis (Fig. 5.12). 203
(A) Irritant contact dermatitis with superficial epidermal necrosis, edema, and some neutrophils. (B) There is focal ballooning and necrosis of keratinocytes in the upper epidermis together with spongiosis and a mild infiltrate of neutrophils. (C) There is full thickness epidermal necrosis with subepidermal clefting. (H & E)
If low and medium concentrations of an irritant are applied, the histopathological spectrum of the reactions produced often mimics that seen in allergic contact dermatitis, with epidermal spongiosis, mild superficial dermal edema, and a superficial, predominantly perivascular infiltrate of lymphocytes (Fig. 5.13).198.199. and 204. The lymphocytes are of helper/inducer type. 132 Langerhans cells are found diffusely through the upper dermis from day 1 to day 4 following contact with the irritant; this is in contrast to allergic contact dermatitis in which these cells are more perivascular in location and persist in the dermis for a longer period. 132 Occasional apoptotic keratinocytes may be seen in the epidermis in irritant reactions.205. and 206. In the recovery phase of irritant dermatitis mild epidermal hyperplasia is often present. Psoriasiform hyperplasia may develop in chronic irritant reactions.
Mixed irritant and allergic contact dermatitis. (H & E)
Pustular reactions show subcorneal vesicles with neutrophils, cellular debris, and a fibrinous exudate. There are also some neutrophils in the upper dermal infiltrate.
A detailed study using various irritants and human volunteers has confirmed the marked variability in histopathological responses, depending on the chemical used. 190 For example, propylene glycol produced hydration of corneal cells and a prominent basket-weave pattern. 190 Nonanoic acid resulted in tongues of eosinophilic keratinocytes with shrunken nuclei in the upper epidermis; croton oil caused a spongiotic tissue reaction resembling allergic contact dermatitis. 190 Sodium lauryl sulfate produced a thick zone of parakeratosis; dithranol caused some basal spongiosis and pallor of superficial keratinocytes; benzalkonium resulted in mild spongiosis, sometimes accompanied by foci of necrosis in the upper spinous layers. 190 The ultrastructural changes also varied widely with the different irritants. 190 It is obvious that further studies using other potential human irritants are needed to increase our understanding of the diversity of irritant reactions.
Allergic contact dermatitis is an important dermatological disease with considerable morbidity and economic impact. 207 It is an inflammatory disorder which is initiated by contact with an allergen to which the person has previously been sensitized.132. and 184. The prevalence of contact dermatitis (both irritant and allergic) in the general population in the United States has been variably estimated to be between 1.5% and 5.4%. 152 It is uncommon in children.208. and 209. Allergic contact dermatitis has always been thought to be less frequent than irritant dermatitis, but recent studies show the reverse to be the case. 210 Both are a significant occupational problem.211. and 212. Hairdressers are one of the largest groups affected by occupational contact dermatitis. 213 This risk is heightened if underlying atopy is present. 214 The use of hair dyes is an important contributor to this problem. 215 Veterinarians are prone to develop contact dermatitis on the hands and forearms. 216 Athletes are another group of individuals that confront a range of irritants and allergens. This subject was reviewed in 2007. 217 Pool toes, a sports-related dermatosis of swimmers, is an allergic contact dermatitis to cement. 218 Jogger’s nipples, an eczematous disease of the nipples occurring in joggers, has a multifactorial etiology, including underlying atopy. 219
Clinically, there may be erythematous papules, small vesicles or weeping plaques, which are usually pruritic. The lesions develop 12–48 hours after exposure to the allergen. In the case of cosmetic reactions, the face, eyelids, and neck are commonly involved, but the lesions may extend beyond the zone of contact, in contrast to irritant reactions.220. and 221. Eyelid dermatitis is a multifaceted clinical problem, but allergic contact dermatitis is a common cause, even among those with atopic eczema. 222 Eye drops containing phenylephrine hydrochloride have also resulted in a contact reaction of the eyelids. 223 Cheilitis is another regional dermatitis which may be due to constituents of mouthwash224 and lipstick. 225 Anogenital dermatitis is another localized form of contact dermatitis.226. and 227. With occupational exposures, the hands are frequently involved.161.228. and 229. An uncommon cause of hand dermatitis is contact with the smoking equipment nargile (hubble-bubble). 230 Stasis dermatitis of the lower parts of the legs is particularly susceptible to allergic contact reactions. 231 Contact sensitivity is also increased in patients with past or present leg ulcers. 232 Rarely reported allergic reactions include follicular or pustular lesions,233. and 234. systemic contact reactions, and urticarial, 235 granulomatous, 236 leukodermic237 or erythema multiforme-like lesions.238.239. and 240. Pustular contact dermatitis has developed on the scalp following the use of topical minoxidil. 234 Purpuric lesions, which may go on to resemble pigmented purpuric dermatosis, are a rare manifestation of contact allergy. They usually result from contact with resins or textile dyes, particularly Disperse Blue.241.242. and 243. Resolution of allergic contact dermatitis usually occurs 2–3 weeks after the withdrawal of the relevant allergen or cross-sensitizing agent.
Two patients have been reported with long-standing pustular psoriasis who developed coexistent allergic contact dermatitis. 244
Numerous agents, including more than 3000 chemicals, 245 have been incriminated in the etiology of allergic contact dermatitis. 246 They include cosmetics, 247 foodstuffs, plants,248. and 249. topical medicaments, and industrial chemicals. 250 Reactions to cosmetics may result from the fragrances, 251 preservatives,252.253.254. and 255. or lanolin base.220.256.257.258.259.260.261.262.263.264.265.266.267. and 268. An expired moisturizer (sorbolene cream) has also been incriminated, probably due to the development of degradation products in the cream. 269 Cinnamic aldehyde in deodorants is an important cause of axillary dermatitis. 270 A substantial number of reactions occur to the four fragrance chemicals cinnamal/cinnamic alcohol and isoeugenol/eugenol.271.272. and 273. Kumkum, a colored cosmetic used by Hindu women, is an important cause of a contact dermatitis.214. and 274. Another constituent of fragrances, oxidized citrus oil (R-limonene), is a frequent skin sensitizer in Europe. 275Foodstuffs that have been implicated include flavorings, spices, 276 animal and fish proteins, olive oil, 277 flour additives, 278 citrus fruits, 279 shiitake mushrooms,280. and 281. macadamia nuts, 282 mangos,283. and 284. cinnamon, 285 onions, spinach, 286 broccoli, 287 asparagus, 288 garlic, and chives.289.290.291. and 292. Preservatives used in animal feed and in other industries may produce an occupational dermatitis.293. and 294. The plants include poison ivy,295.296.297.298.299.300. and 301. other species of Rhus, 302 various members of the Compositae family,295.303.304.305.306. and 307. melaleuca (tea tree) oil,308.309. and 310. the latex of mangrove trees, 311Agave americana, 312 tulips, 313 hydrangea, 314 sunflower, 315 and Alstroemeria (Peruvian lily).316. and 317. Botanical ingredients, such as lichens, used in personal care products such as deodorants, are an underreported cause of allergic contact dermatitis. 318 Plant particles and some chemicals may give rise to contact reactions by airborne spread.154.319.320. and 321. In the past, topical medicaments such as penicillin, sulfonamides, mercurials, and antihistamines were the most common sensitizers. 322 Currently neomycin and other topical antibiotics, 323 benzocaine, ethylenediamine (a stabilizer), parabens preservatives, and propylene glycol are common causes of such reactions.142.322.324. and 325. Other sensitizers, mostly industrial based, include potassium dichromate, gold,326.327. and 328. mercury, 329 nickel salts (see below), cobalt,330. and 331. chromate,331. and 332. formaldehyde, 333 formaldehyde-releasing preservatives, 334 phenol-formaldehyde resin, 335 chemicals in rubber,336.337.338.339.340. and 341. natural rubber latex,213.342. and 343. color film developers, 344 acrylic and epoxy resins,345.346.347.348.349. and 350. acrylates in artificial nails,351. and 352. cyanoacrylate in topical skin adhesives, 353 immersion oil,319. and 354. coloring agents, henna,355. and 356. ‘paint-on’ tattoos,357.358.359.360.361. and 362. textile dyes,363.364.365.366.367.368. and 369. disposable gloves,370.371. and 372. sanitary pads, 373 baby wipes, 334 cinnamic aldehyde, 270 compound tincture of benzoin, 374 quarternium-15, 375 and phenylenediamine.376. and 377. Less common causes include doxepin cream,378. and 379. ciclopirox olamine (topical antifungal), 380 topical calcipotriol, 381 vitamin E preparations, 322 lanolin, 382 topical corticosteroids,383.384.385.386.387.388.389.390.391.392.393.394.395.396.397.398.399.400. and 401. non-steroidal anti-inflammatory drugs (NSAIDs),402. and 403. tacrolimus ointment, 404 pimecrolimus, 405 infliximab, 406 bacitracin, 407 mupirocin, 408 topical minoxidil, 234 enoxolone, 409 lanoconazole, 410 miconazole, 411 propacetamol, 412 surgical adhesive materials,353.413. and 414. thiourea in a neoprene knee brace, 415 topical amide anesthetics,416.417.418.419. and 420. idoxuridine, 421 tefillin (phylacteries), 422 Unna boots, 423 other footwear,424.425. and 426. laundry detergents, 427 benzalkonium chloride, 428 pentylene glycol, 429 plastic banknotes, 430 air bags, 139 cellular phones, 431 oils used in aromatherapy,432.433. and 434. antiseptic bath oils,435.436. and 437. anethole in spearmint flavored toothpaste, 438 tear gas (2-chloroacetophenone),439. and 440. fluorouracil, 441 5-aminolevulinic acid methylester used in photodynamic therapy, 442 and psoralens. 443 Xylitol, a sweetener in chewing gum, can cause an oral erosive ‘eczema’. 444 Allergic contact dermatitis can be provoked or intensified by chemically related substances. These cross-sensitization reactions are an important clinical problem. 322 Inhalation of corticosteroids in the treatment of asthma may reactivate allergic contact dermatitis in individuals with prior skin reactions to topical corticosteroids. 445 Information on contact dermatitis and the Contact Allergen Replacement Database can be obtained at the American Contact Dermatitis Society website at www.contactderm.org. 245 The European Surveillance System of Contact Allergies (ESCA) collects data and monitors the situation in Europe. 446
Nickel allergy is an important cause of morbidity, especially from hand dermatitis.447.448.449.450.451.452.453.454. and 455. Loss-of-function mutations in the filaggrin (FLG) gene, which are also seen in atopic dermatitis, may represent a risk factor for contact sensitization to various allergens, including nickel. 456 The prevalence of nickel allergy is much lower in men; there is evidence to suggest that ear piercing followed by the use of nickel-containing earrings accounts for this difference.448.457. and 458. Nickel allergy is important in children. Belt buckles may produce an umbilical dermatitis, sometimes associated with a papular id reaction.459.460. and 461. Nickel-containing coins have also been incriminated as a risk factor for allergic contact dermatitis of the hands.462.463. and 464. Avoidance of skin contact with and dietary intake of nickel is difficult to achieve. 451 A European Union directive to reduce nickel release in consumer products has had a beneficial effect. Nickel exposure from inexpensive earrings in the United States where no such directive exists is an important source of nickel exposure. 465 Cosensitizations to copper, 466 cobalt, and chromate are sometimes present. 467 Chromium-related dermatitis has an onset in later working life and often affects those in the building trades. 331 In contrast cobalt-related dermatitis has an earlier onset and may affect a wide range of employments. 331 Allergy to metal implants is an increasing clinical problem. It is discussed with systemic contact reactions (see p. 117).
The specific allergen responsible for allergic contact dermatitis can be identified using a patch test.468.469.470.471.472. and 473. However, these reactions are not always reproducible at sequential or concomitant testing. In the United States, the commonly used patch test procedure is the TRUE (Thin-layer Rapid Use Epicutaneous) Test. 207 Analysis of results produced by these tests has shown that nickel (14.7% of tested patients), thimerosal (5.0%), cobalt (4.8%), fragrance mix (3.4%), and balsam of Peru (3.0%) are the most prevalent allergens. 207 By contrast, the North American Contact Dermatitis Data Group (NACDG) data show that the most prevalent allergens are nickel (14.3%), fragrance mix (14%), neomycin (11.6%), balsam of Peru (10.4%), and thimerosal (10.4%). 207 The prevalence of allergy to cobalt in this database is 9.2%. 207 Reactions to fragrances, rubber accelerators, pesticides, and formaldehyde may be missed with the TRUE Test. 474 There is some evidence that constituents of the patch test panel may sometimes produce active sensitization. 475 Confocal reflectance microscopy has been used to study allergic and irritant contact dermatitis.476. and 477. Initial studies are promising, but it is an adjunctive tool, rather than a substitute for clinical evaluation. 478
Allergic contact dermatitis is a special type of delayed hypersensitivity reaction.479. and 480. In cases produced by chemicals, an associated irritant reaction is often present. 481 Furthermore, an irritant contact dermatitis facilitates allergic contact sensitization. 482 The compound responsible for the allergic reaction is usually of low molecular weight (a hapten) and lipid soluble. 483 After penetrating the skin, the hapten becomes bound to a structural or cell surface protein, usually by a covalent bond, thus forming a complete antigen.152.484. and 485. This antigen is processed by Langerhans cells, other dendritic cells, 486 and possibly macrophages, 487 and then presented to T lymphocytes.488. and 489. The actual way in which the Langerhans cells interact with the antigen and lymphocytes is not known, although the dendritic nature of Langerhans cells obviously assists in their antigen-presenting role.152.490. and 491. Various regulatory proteins also influence the function of these dendritic cells. 492 Keratinocyte-derived cytokines influence this initial phase of the response. 493 Keratinocytes can mature functionally and become potent antigen-presenting cells in the same way that Langerhans cells do. 494 This induction phase is followed by migration of T lymphocytes to the regional lymph nodes where there is clonal expansion of specifically sensitized lymphocytes. 447 On second and subsequent exposures to the allergen, the elicitant response occurs with proliferation of T lymphocytes in both the skin and regional lymph nodes.407.483. and 495. There is activation of T cells of both CD4+ Th1 and CD8+ Tc1 types. 496 The homing of lymphocytes to the antigen-exposed skin involves various cell adhesion molecules, such as lymphocyte function-associated antigen-1 (LFA-1).489.497. and 498. Natural killer T cells are also present. 499 Fibronectin is expressed in dermal vessels in positive patch test reactions; it may contribute to the recruitment of leukocytes to the site. 486 Lymphocytes liberate various cytokines in the affected area of skin, 479 including IL-1α, IL-1β, IL-2, IL-4, IL-6, IFN-γ, and TNF-α,194.195. and 451. leading to a further influx of inflammatory cells, particularly non-sensitized lymphocytes and some eosinophils. These cytokines trigger the release of secondary chemokines such as CCL20 and CXCL8 that further contribute to the trafficking of immune cells to the affected site. 500 The role of IL-12, produced by keratinocytes subject to stimulation with allergens, needs clarification in further studies. 501 Basophils may play a role in a very limited group of circumstances.484. and 502. Epidermal proliferation is also stimulated. 503 The actual pathogenesis of the spongiosis still requires elucidation but it may be due to a reduction in keratinocyte membrane E-cadherin with retention of desmosomal cadherins. 504 Hypersensitivity to an allergen may persist for prolonged periods, although in a proportion of cases it subsides or disappears with time. 505
A systematic review of the treatment of contact dermatitis published in 2005 found that potent or moderately potent steroids effectively treat allergic contact dermatitis. 197 Isolated studies have supported this finding. 506 The review suggested that the use of non-steroid medications to treat allergic contact dermatitis needs closer examination. 197 The study also found that rhus dermatitis can be prevented by a skin protectant or quaternium 18 bentonite (organoclay). 197 Diethylenetriamine pentaacetic acid (chelator) cream prevents nickel, chrome, and copper dermatitis. 197 The topical application of antioxidants in guinea pigs had some beneficial effect in reducing the sensitization to the experimental allergen. 507 Tacrolimus ointment has been used successfully to treat the eczematous condition know as ‘jogger’s nipples’ (see above.). 219
Allergic contact dermatitis is characterized in the very early stages by spongiosis, which is most marked in the lower epidermis. This is followed by the formation of spongiotic vesicles at different horizontal and vertical levels of the epidermis. This often has a very ordered pattern (Fig. 5.14 and Fig. 5.15). When present, it allows a distinction to be made from nummular dermatitis, which may, at times, closely mimic allergic contact dermatitis histopathologically (see below). Vertical spongiosis, in which keratinocytes are oriented, and somewhat elongated, in a vertical plane is sometimes seen, but it can also be seen in other spongiotic disorders, such as drug reactions.
Allergic contact dermatitis. (A) There is spongiotic vesiculation. (B) Another case due to an allergic contact reaction to a plant in a florist. (H & E)
Allergic contact dermatitis with exocytosis of eosinophils and lymphocytes into the spongiotic epidermis. (H & E)
The upper dermis contains a mild to moderately heavy infiltrate of lymphocytes, macrophages and Langerhans cells, with accentuation around the superficial plexus. Multinucleate dendritic–fibrohistiocytic cells are present in the upper dermis. 510 Eosinophils are usually present, but in some cases only in small numbers. 511 There is exocytosis of lymphocytes and sometimes eosinophils. Eosinophil exocytosis is fairly characteristic of allergic contact dermatitis or a drug reaction. It can also occur in conditions characterized by eosinophilic spongiosis, which is an uncommon pattern in allergic contact dermatitis despite the finding of Wildemore et al. 510 In contrast, exocytosis of eosinophils is uncommon in nummular dermatitis, although exocytosis of lymphocytes and occasional neutrophils is characteristic.
In lesions that persist, scale crust and epidermal hyperplasia develop and the dermal inflammatory cell infiltrate becomes denser. Chronic lesions may show little spongiosis but prominent epidermal hyperplasia of psoriasiform type. 511 Mild fibrosis may develop in the papillary dermis.
Marker studies have shown that the lymphocytes are predominantly helper-T cells with CD4 (Leu 3) positivity. 512 The cells are often positive for Leu 8 and 9, markers which are uncommon in the lymphocytes in mycosis fungoides. 512 The CD1a stain shows an increased number of Langerhans cells in the epidermis. 513
There are several histologically distinct variants of contact dermatitis, some of which may involve an irritant rather than an allergic mechanism. Urticarial (see p. 203) and systemic contact (see p. 117) variants are discussed elsewhere. The status of the erythema multiforme-like pattern,238. and 239. and a personally studied lichenoid reaction resulting from contact with chemicals in the wine industry is uncertain. The various types of contact dermatitis are shown in Table 5.3.
Allergic
Dermal
Erythema multiforme-like
Follicular
Granulomatous
Ichthyosiform
Irritant
Leukodermic
Lichenoid
Lymphomatoid
Photoallergic
Phototoxic
Protein
Purpuric
Pustular
Systemic
Urostomy-associated
Urticarial
Pustular contact dermatitis shows exocytosis of neutrophils and the formation of subcorneal pustules. 233 Neutrophilic spongiosis is sometimes present. Contact with cement may produce this pattern.
Purpuric contact dermatitis, from contact with textile dyes and resins (see above), usually shows a mild lymphocytic vasculitis with red cell extravasation. 241 With time, many cases go on to resemble one of the pigmented purpuric dermatoses (see p. 232) with the accumulation of hemosiderin in the upper dermis. In one case of acute purpuric dermatitis from contact with Agave americana, a leukocytoclastic vasculitis was present. 514
Dermal contact dermatitis, another special variant of allergic contact reaction, has been poorly documented. Mild edema of the papillary dermis can be seen in many cases of the usual type of allergic contact dermatitis, but more pronounced edema may result from exposure to topical neomycin and to zinc and nickel salts. Such cases are called dermal contact dermatitis (Fig. 5.16). Autoeczematization (see p. 115) produces a similar pattern.
Allergic contact dermatitis with prominent edema of the papillary dermis. Certain specific contactants are usually associated with this pattern (see text). It also resembles the reaction seen in autosensitization. (H & E)
Photoallergic contact dermatitis is considered with the photosensitivity disorders (see Ch. 21, p. 535). The histopathological changes may resemble those seen in allergic contact dermatitis. In cases of some months’ duration there is often telangiectasia of superficial vessels, increased and more deeply extending elastotic fibers, deep perivascular extension of the infiltrate, and stellate cells in the upper one-third of the dermis.
Granulomatous contact dermatitis refers to the presence of granulomas in the dermis resulting from a contactant. Sarcoidal granulomas have been found at the sites of ear piercing with gold earrings. 236 Dermal granulomas have resulted from the use of propolis, a resinous beehive product used in folk medicine. 515 In the papular lesions that result from penetration of the allergen into the dermis in ‘bindii’ (Soliva pterosperma) dermatitis, there is a mixed dermal infiltrate with some foreign body giant cells.516. and 517. Marked edema of the papillary dermis is usually present and draining sinuses may form. 516
Lymphomatoid contact dermatitis is a poorly understood variant of allergic contact dermatitis in which the histological appearances may simulate cutaneous T-cell lymphoma.518.519. and 520. There is a heavy infiltrate of lymphocytes in the upper dermis in a so-called ‘T-cell pattern’ of distribution. Most of the reported cases have resulted from contact with chemicals or metals, such as nickel or gold.521.522. and 523. The author has seen a recurrent case (Fig. 5.17), with a heavy superficial dermal infiltrate, that resulted from contact with Noogoora burr (Xanthium occidentale). Drugs have occasionally been implicated. 524 This latter case has since progressed to T-cell prolymphocytic leukemia, throwing into doubt the original diagnosis. 525
(A) Lymphomatoid contact dermatitis. (B) A dense infiltrate of lymphocytes, some mildly atypical, fill the upper dermis. The eruption developed on several occasions after contact with Noogoora burr. (H & E)
Leukodermic contact dermatitis is characterized by hypopigmentation occurring at sites of allergic contact dermatitis, as a consequence of postinflammatory melanin incontinence. It results, uncommonly, from the destruction of melanocytes or from a reduction in melanin synthesis. Betel chewing and contact with lubricants can rarely produce a vitiligo-like leukoderma as a consequence of melanocyte destruction.237. and 413. This is strictly an irritant rather than an allergic contact mechanism.
Follicular contact dermatitis has been reported following contact with formaldehyde and polyoxyethylene laurylether (used in cosmetics). 526 The papules show follicular spongiosis.
Ichthyosiform contact dermatitis has been reported following the use of cetrimide. It is regarded as an acquired form of ichthyosis.
Protein contact dermatitis usually presents as a chronic eczema with episodic acute exacerbations a few minutes after contact with the offending agent. 527 The lesions are usually confined to the hands and forearms because occupational allergens are usually involved. Patch testing is usually negative when read at 48 hours. Approximately 50% of those involved are atopic.
It appears that a combined type I and IV immunological reaction is present. The causative ‘protein’ is either a fruit, vegetable, plant, animal protein, grain, or enzyme.527.528.529.530.531. and 532.
No distinguishing histological features have been recorded for this variant of contact dermatitis. There may be more edema of the papillary dermis than in allergic contact dermatitis.
Nummular dermatitis (nummular eczema) commences with tiny papules and papulovesicles that become confluent and group themselves into coin-shaped patches which may be single or multiple.533. and 534. The surface is usually weeping or crusted and the margins are flat. Central clearing may occur. Sites of predilection include the dorsum of the hands, the extensor surface of the forearms, the lower part of the legs, the outer aspect of the thighs, and the posterior aspect of the trunk. 534 The course is usually chronic with remissions and exacerbations.533. and 535.
The etiology is unknown but numerous factors have been implicated over the years, often with very little basis. External irritants, cold, dry weather, and a source of infection are factors which may aggravate nummular dermatitis.535. and 536. In one series, all the cases were said to be related to varicose veins and/or edema of the legs, suggesting stasis with autoeczematization as an etiological factor. 537 Several drugs, such as methyldopa, latanoprost eye drops, 538 gold and antimycobacterial drugs in combination, and interferon alfa-2b in combination with ribavirin, 539 appear to provoke nummular eczema. 540 Mercury in dental fillings has also been implicated. 541 There is no evidence for an atopic basis, as once thought.533.534. and 542.
Little has been written recently on the treatment of nummular dermatitis. In one study, hydration (soaking) for 20 minutes before bedtime followed by the application of corticosteroid ointment to wet skin produced good results. 543
The appearances vary with the chronicity and activity of the lesion. In early lesions there is epidermal spongiosis and sometimes spongiotic vesiculation associated with some acanthosis and exocytosis of inflammatory cells, including lymphocytes and occasional neutrophils. The spongiotic vesicles sometimes contain inflammatory cells, 537 simulating Pautrier microabscesses. There is progressive psoriasiform epidermal hyperplasia but this is not always as uniform as in allergic contact dermatitis (see above), which otherwise closely mimics nummular dermatitis. Scale crust often forms above this thickened epidermis. There is a superficial perivascular infiltrate in the dermis composed of lymphocytes, some eosinophils and occasional neutrophils and plasma cells. Nummular dermatitis often has an ‘untidy appearance’ microscopically (Fig. 5.18).
(A) Nummular dermatitis. (B) There is spongiosis, irregular acanthosis and exocytosis of inflammatory cells. (C) Often nummular dermatitis has an ‘untidy’ appearance. (D) A chronic case with superimposed lichen simplex chronicus. (H & E)
Progressive rubbing and scratching of individual lesions lead to ulceration or the superimposed changes of lichen simplex chronicus.
A rare entity, of doubtful status, Sulzberger–Garbe syndrome is also known as ‘the distinctive exudative discoid and lichenoid chronic dermatosis of Sulzberger and Garbe’.545. and 546. ‘Oid-oid disease’ has also been used as a designation in the past. It is regarded by some as a variant of nummular dermatitis, 544 although there are clinical differences. These include larger lesions, intense pruritus, a high prevalence of penile and facial lesions, and a predilection for Jewish males. 547
The histological changes are usually indistinguishable from those of nummular dermatitis. Scattered apoptotic keratinocytes are usually present in the basal layer. Dilatation of superficial vessels with endothelial swelling and perivascular edema have been regarded as characteristic features, 545 although not universally accepted. 544 If this disease is a variant of nummular dermatitis, it follows that apoptotic keratinocytes are also an acceptable finding in nummular dermatitis.
Seborrheic dermatitis is a chronic dermatosis of disputed histogenesis. It has a prevalence of 1–3% in the general population.548. and 549. It consists of erythematous, scaling papules and plaques, sometimes with a greasy yellow appearance, with a characteristic distribution on the scalp, ears, eyebrows, eyelid margins, and nasolabial area – the so-called ‘seborrheic areas’.548. and 550. Less commonly, it may involve other hair-bearing areas of the body, particularly the flexures and pectoral region. Males are more commonly affected. 548 Seborrheic dermatitis is not usually seen until after puberty; the exact nosological position of cases reported in infancy (infantile seborrheic eczema) is uncertain551 and their occurrence may represent another variant of the atopic tendency.552.553.554.555. and 556. The prevalence of seborrheic dermatitis was 10% in an Australian study of pre-school children. The incidence was highest in the first 3 months of life, decreasing rapidly by the age of 1 year. 557
Seborrheic dermatitis is one of the most common cutaneous manifestations of the acquired immunodeficiency syndrome (AIDS), affecting 20–80% of patients.558.559. and 560. In these circumstances, it is often quite severe and atypical in distribution. It has been reported in association with alopecia following combination antiretroviral therapy. 561 Seborrheic dermatitis is also seen with increased frequency in association with a number of medical disorders which include Parkinson’s disease, 562 epilepsy, congestive heart failure, obesity, chronic alcoholism, Leiner’s disease (exfoliative dermatitis of infancy), and zinc deficiency.550. and 558. It has been reported after decompression of a Chiari I malformation; its distribution was unilateral. 563 A seborrheic dermatitis-like rash that evolved into erythroderma has been reported as a paraneoplastic phenomenon. 564 The high prevalence of seborrheic dermatitis in mountain guides (16%) may be the result of UV-induced immunosuppression from the occupational sun exposure. 565 Seborrheic dermatitis may occur as a reaction to arsenic, gold, chlorpromazine, methyldopa, 550 and cimetidine. 566
Pityriasis amiantacea consists of asbestos-like sticky scales, which bind down tufts of hair, involving localized areas of the scalp.567.568. and 569. Scarring alopecia is a rare complication. 570 Seborrheic dermatitis is often present, although it is uncertain whether the two conditions are related. 568 Pityriasis amiantacea is best regarded as a particular reaction pattern of the scalp to various inflammatory scalp diseases, particularly seborrheic dermatitis and psoriasis. 571
Dandruff is an extremely common affliction of the scalp; its presence can lead to loss of self-esteem and a negative social image. 572 Dandruff has been regarded as a mild expression of seborrheic dermatitis by some and as a completely separate disorder by others.548.573. and 574. It is sometimes used for any flaking of the scalp, regardless of origin. A resurgence in interest in the role of Malassezia yeasts in the development of both seborrheic dermatitis and dandruff has led to the view that these two conditions are differing severity manifestations of the same condition.196.572. and 575.M. globosa and M. restricta are the species most closely related to both dandruff and seborrheic dermatitis. 572
Traditionally, seborrheic dermatitis has been regarded as a dysfunction of sebaceous gland activity, often associated with an oily complexion. This view was supported by its localization to the ‘seborrheic areas’ of the body. A more recent study has shown, however, that the sebum excretion rate is not increased in patients with seborrheic dermatitis. 576 The role of Malassezia sp. (Pityrosporum) in the etiology is also controversial.577.578. and 579. This organism is usually quantitatively increased in both seborrheic dermatitis and dandruff but there is dispute about whether this is causal or a secondary event related to the increased keratin scale.580.581.582. and 583. There has been a recent resurgence of interest in the role of this organism in the pathogenesis of seborrheic dermatitis. 584 Its role in HIV-related cases is doubted; 585 no quantitative differences are usually observed in the number of yeasts in HIV-related and non-HIV-related seborrheic dermatitis. 583 There is some evidence favoring an abnormal immune response to Malassezia furfur and possibly other organisms as well, although this has been refuted in recent studies.586.587.588.589. and 590. Other possible explanations include the production of an inflammatory mediator or alterations in lipase activity by Malassezia. 589Malassezia furfur seems to play no role in the pathogenesis of the infantile form, further evidence that it may be a different disease. 591 A reclassification of the various species of Malassezia took place some years ago (see p. 592). Using the new classification it appears that M. globosa and M. restricta are most closely related to seborrheic dermatitis, although other species (which are the most culturally robust) have also been isolated.572. and 592. Using DNA-based detection methods, M. globosa and M. restricta were the usual species isolated. 572
Seborrheic dermatitis can be treated with various keratolytic agents, some of which are available over the counter. Selenium sulfide is one such preparation. It is available as a shampoo to treat scalp disease, including dandruff. Tar products, lithium succinate ointment, benzoyl peroxide, and propylene glycol have also been used. 584 Anti-inflammatory products, such as topical corticosteroids, have some effect. 593 Specific antifungal agents, both topical and oral, including zinc pyrithione (it has keratolytic activity as well), the azoles, and allylamines are other therapies. 584 Ciclopirox olamine, used as a shampoo or cream, is another effective treatment. 584 Recently, pimecrolimus cream 1% has been used successfully to treat moderate to severe facial seborrheic dermatitis. 593 Mild to moderate disease has been successfully treated with Sebclair, a novel steroid-free cream containing multiple active ingredients. 594
The changes are those of an acute, subacute or chronic spongiotic dermatitis depending on the age of the lesion biopsied (Fig. 5.19). In acute lesions there is focal, usually mild, spongiosis with overlying scale crust containing a few neutrophils; the crust is often centered on a follicle. The papillary dermis is mildly edematous; the blood vessels in the superficial vascular plexus are dilated and there is a mild superficial perivascular infiltrate of lymphocytes, histiocytes, and occasional neutrophils. 597 There is some exocytosis of inflammatory cells but this is not as prominent as it is in nummular dermatitis.
Seborrheic dermatitis. (A) Spongiosis is not a feature in this biopsy. There is psoriasiform hyperplasia of the epidermis and focal parakeratosis. (B) Spongiosis is quite widespread in this subacute case. (H & E)
In subacute lesions there is also psoriasiform hyperplasia, initially slight, with mild spongiosis and the other changes already mentioned. Numerous yeast-like organisms can usually be found in the surface keratin.
Chronic lesions show more pronounced psoriasiform hyperplasia and only minimal spongiosis. Sometimes the differentiation from psoriasis can be difficult but the presence of scale crusts in a folliculocentric distribution favors seborrheic dermatitis.
The seborrheic dermatitis related to AIDS shows spotty cell death of keratinocytes, increased exocytosis of leukocytes, and some plasma cells and neutrophils in the superficial dermal infiltrate. 559
There are no spongiotic or inflammatory changes in dandruff, but only minute foci of parakeratosis scattered within the thickened orthokeratotic scale. 597 Electron microscopy of scalp tape strips shows that dandruff scalp possesses abnormal ultrastructure of the stratum corneum which is improved with zinc pyrithione shampoo. 598
Atopic dermatitis (atopic eczema) is a chronic, pruritic, inflammatory disease of the skin which usually occurs in individuals with a personal and/or family history of atopy (asthma, allergic rhinitis and atopic dermatitis).599.600.601.602.603.604.605.606.607. and 608. It is a common disorder with an incidence of approximately 1–2%; 600 its prevalence appears to be increasing in children, 609 particularly in the Western world, where incidences as high as 15–20% have been recorded.610.611.612.613.614.615.616.617.618.619.620.621.622. and 623. Onset is usually in infancy or childhood.602. and 624. It is associated with considerable morbidity and resource use. 625 Insufficient attention has been given to a major cause of this morbidity – itch.626. and 627.
The diagnosis of atopic dermatitis is made on the basis of a constellation of major and minor clinical features.628.629.630.631.632. and 633. Its distinction from infantile seborrheic dermatitis is sometimes difficult.552.604.634.635. and 636. Major criteria for the diagnosis of atopic dermatitis include the presence of pruritus, chronicity, and a history of atopy, as well as lesions of typical morphology and flexural distribution.601. and 628. Boys are more often atopic than girls. 637 In infants and young children there is an erythematous, papulovesicular rash with erosions involving the face and extensor surfaces of the arms and legs. 638 The involvement of the scalp, forehead, ear, and neck has been described as a ‘balaclava’ distribution. 639 These early lesions are followed by more typical lesions involving the flexures of the extremities. 639 This progresses with time to a scaly, lichenified dermatitis. 640 Involvement of the hands and feet may occur at a later stage. Adult-onset atopic dermatitis is a recently introduced subgroup. 641 In addition to the typical lichenified/exudative lesions of the flexures, a non-flexural distribution may also occur. 642 Nummular and prurigo-like lesions may develop in adults. 642 The vulva and nipples are sometimes involved.643.644. and 645. Itchy follicular papules on the trunk are quite common in Oriental and black patients.646. and 647. A patient with linear distribution of the lesions has been reported. 648 In another, there was increased severity along a line of Blaschko. 649
Minor clinical features599.601. and 650. include xerosis, which may be focal or generalized, elevated IgE which is allergen specific, 651 interleukin-2 receptor (IL-2R), 652 eosinophil cationic protein (ECP),653.654. and 655. E-selectin656.657.658. and 659. and IgG4 in the serum,640.660. and 661. increased colonization of the skin with Staphylococcus aureus,662.663. and 664. a greater risk of viral and fungal infections of the skin, 665 pityriasis alba, 638 rippled hyperpigmentation, 666 reduced numbers of melanocytic nevi, 667 keratosis pilaris, cheilitis, nipple eczema, food intolerance,668. and 669. orbital darkening, white dermatographism, and an increased incidence of dermatitis of the hands, including pompholyx and irritant dermatitis.670. and 671. Although one study found an increased risk of malignancy, albeit of borderline statistical significance, 672 another study has reported a lower risk. 673 Hypertension is also rare in adult patients with atopic eczema. 674 Patients with severe disease have low basal serum cortisol levels, a finding previously attributed to the use of potent topical corticosteroids. 675 The ethnic background of the patient appears to influence the phenotype and the relative incidence of the various minor clinical features in atopic dermatitis. 676
A distinctive clinical variant of atopic dermatitis (lichenoid atopic dermatitis) has been reported in nearly 10% of patients presenting to one institution in the United States. 677 Lesions were almost indistinguishable clinically from lichen planus but without the pathological findings of lichen planus. 678 All patients were heavily pigmented (Fitzpatrick skin types V and VI) persons. 677 The lesions were spongiotic with mild lymphocyte exocytosis and only scattered apoptotic keratinocytes. 677
Atopic dermatitis-like skin lesions (atopiform dermatitis) can be seen in a number of genodermatoses, 651 the most important of which is ichthyosis vulgaris. 638 They also occur in the Wiskott–Aldrich syndrome,679. and 680. in X-linked agammaglobulinemia, 681 in ataxia-telangiectasia, in IPEX syndrome, 682 in Andogsky syndrome (atopic dermatitis with cataracts), 683 and in some patients with phenylketonuria. 638 Atopic dermatitis is also a feature of Job’s syndrome (see p. 942).684.685. and 686. An atopic diathesis is also found in Netherton’s syndrome (see p. 253), due to a defect in the SPINK5 gene at 5q31–q32. 687 Polymorphisms in this gene have been associated with atopic dermatitis in one Japanese study. 687 The incidence is probably not increased in Down syndrome. 688
The term atopiform dermatitis has been used in the past for the atopic dermatitis-like eruptions associated with some genodermatoses (see above). It is now being used for the ‘intrinsic’ type of atopic dermatitis, which is characterized by the absence of allergen-specific IgE. 689 This group has female predominance, absence of atopic diseases, later onset of the disease, and milder clinical severity; it may be a distinct disease. 689
Two cases of an atopic dermatitis-like rash have been reported in psoriasis patients treated with infliximab. 690 Patchy pityriasiform lichenoid eczema, characterized by scaly follicular papules forming larger plaques, is another variant of atopic dermatitis. 691
The course of atopic dermatitis is one of remissions and exacerbations; the symptom-free periods tend to increase with age. 601 There is also a tendency towards spontaneous remission in adult life, although some recent studies have shown lower remission rates than previously thought. 692 Sleep disturbance is common in patients with atopic dermatitis. 693 Outcome studies, including the response to various treatments,694.695.696.697.698.699.700.701. and 702. rely on consistency in the measurement of disease activity/severity. Unfortunately, there is less consistency than is desirable between the various severity scales. 703 The serum levels of IL-16, IL-18, IgE, and cutaneous T-cell attracting chemokine (CTACK) are a good reflection of disease severity.704.705.706. and 707. Some children with atopic dermatitis will develop allergic respiratory diseases later in childhood. 708 Positive skin-prick tests to food allergens, severe skin disease and a high serum IgE level are risk factors for the later development of allergic respiratory disease. 709
Although the etiology and pathogenesis of atopic dermatitis are still unclear, evidence suggests that IgE-mediated late phase responses, as well as cytokine imbalances and cell-mediated reactions (T-lymphocyte activation), contribute in some way.710.711.712.713.714.715.716.717.718.719.720.721.722.723. and 724. Expressed more specifically, there is an expansion of the skin-homing type 2 cytokine-secreting T cells (Th2), leading to increased levels of interleukin-4, -10, -13, and -16, and of IgE.725.726.727.728.729.730.731.732. and 733. There is a corresponding decrease in interferon-γ (IFN-γ).694.725.726. and 734. There is a strong expression of the suppressor of cytokine signaling 3 (SOCS3) in the skin of patients with atopic dermatitis. 735 It may mediate a Th2 regulatory response through negative regulation of Th1 pathways. 735 The expression of CD43 is increased. 736 Keratinocytes are a source of the chemokines that result in the influx of both Th2 cells, and eosinophils. 737 As the disease progresses, there is a switch from Th2 responses to a Th1 profile.
The IgE-mediated reactions may be to ingested food640.738.739.740. and 741. or to inhaled or contactant aeroallergens742.743. and 744. such as human dander, 745 environmental tobacco smoke, 746 grass pollens, 747 disperse clothing dyes, 748 and house dust and other mites.749.750.751.752.753.754.755.756.757.758.759. and 760. Dust mite elimination was thought to have a beneficial effect on the control of atopic dermatitis,756. and 761. but more recent studies have failed to confirm any benefit of dust mite elimination. 762 A recent (2006) systematic review of factors causing worsening of ‘eczema’ found some evidence that certain foods (particularly eggs763), house dust mite, stress,764.765. and 766. and seasonal factors were implicated in certain subgroups. 767 Another review of etiological factors in atopic dermatitis found an inverse relationship between atopic dermatitis and endotoxins, early day care, and animal exposure. 768 There was a positive association between atopic dermatitis and infections in early life, measles vaccination, and antibiotic use.768. and 769. There are significant associations with the presence of dampness in the home, the use of radiators to heat the child’s bedroom, the use of synthetic pillows, 770 and a privileged socio-economic status.771. and 772. Breast-feeding reduces the incidence of atopic dermatitis during childhood in children with a family history of atopy. 773 This effect is negligible in children without first-order atopic relatives. 773 Recent studies have failed to demonstrate any clear relationship between this disease and indoor aeroallergens in early life. 762 There is no association with furry pets. 774 Nevertheless, endotoxin exposure is not only important during the maturation of the immune system early in life but it may influence the development of an allergic disease, such as asthma and atopic dermatitis, in a predisposed individual. 775 Antigens of Staphylococcus aureus and other bacteria, as well as the yeast Malassezia,776.777.778. and 779. have been considered as possible stimulants of the IgE response.725.780.781.782. and 783. Defects in toll-like receptor 2 signaling may be a cause of the reduced ability to clear S. aureus from the skin. 784 About 10% of patients have normal serum IgE levels (non-allergic or intrinsic atopic dermatitis). 785 Studies of this group have shown a lack of interleukin-13-induced B-cell activation, resulting in decreased IgE production. 786
Cellular changes in atopic dermatitis, in addition to the increase in Th2 lymphocytes, include an increase in inflammatory dendritic cells in the epidermis (either altered Langerhans cells or cells derived from the CD34 subset of dendritic cells) 606 and dermis, 787 and an increased life span of eosinophils. 606 Eosinophils are increased in the subgroup of patients with so-called extrinsic disease, in which IgE levels are increased. 788 Langerhans cells appear to be hyperstimulatory.716.789.790. and 791. Langerhans cells and inflammatory dendritic cells express the high affinity receptor for IgE (FcεRI). 792 Such cells are not found in normal skin. Skin fibroblasts produce increased amounts of inducible protein-10 (IP-10), although the significance of this finding is currently unknown. 793
Changes in mediators and receptors occur, 794 but there have been conflicting results depending on the model used and the method of measurement. No single cytokine can be said to have a pivotal role. Increased expression of Fc receptors for IgG795 and of integrins is present. 658 Serotonin, 796 leukotriene E4, 797 nerve growth factor and substance P,765.798. and 799. and matrix metalloproteinase-9 levels are all increased. Prostaglandins may not be as important as previously thought. 800
Patients with atopic dermatitis have a reduced itch threshold801 and greater skin ‘irritancy’.802. and 803. It appears that mast cell mediators other than histamine are involved in the pruritus.804. and 805. These findings may be explained by a more recent study that found that the sensitization for itch in atopic dermatitis may be in the spinal cord rather than in primary afferent neurons. 806 This has implications for treatment and suggests that antipruritic therapy should also focus on these central mechanisms of pruritus. 806
Genetic factors also appear to be involved in the pathogenesis of atopic dermatitis in some way.807.808. and 809. This is confirmed by the frequent presence of a family history of atopy and the high concordance in twins.807.810.811. and 812. There is some allelic association with chromosomes 11q13, 13q12–q14, and 5q31–q33.813. and 814. Interestingly, the gene for the beta subunit of FcγRI, the high affinity receptor for IgE, has been localized to chromosome 11q12–q13. 721 Polymorphisms in the interleukin-13 (IL-13) gene are not associated with atopic dermatitis. A single nucleotide polymorphism in the GATA3 gene is associated with atopic dermatitis. 815 Another candidate gene on chromosome 16p11–p12 is associated with the IL-4R gene. 816 Polymorphisms within the CTLA4 gene at 2q33 have been associated with early-onset disease. 817 It encodes the inhibitory CTLA4 receptor, an important regulator of T cells and cytokine secretion. 817 Single-nucleotide polymorphisms in the eotaxin gene have recently been found in patients with the extrinsic form of atopic dermatitis. 818 Nevertheless cytokine gene polymorphisms may be markers of inflammatory skin diseases in general, rather than specific markers of atopic dermatitis.819.820. and 821.
Finally, impaired skin barrier function plays a key role in the development of atopic disease.822.823.824. and 825. An early study found a reduction in ceramide in the stratum corneum, 826 but in 2006 two loss-of-function variants in the gene encoding the epidermal barrier protein filaggrin (FLG) at 1q21 were reported.824. and 827. Other studies have since confirmed this finding.828. and 829. These genetic variants are found in approximately 9% of people of European origin. There is also a significant association with asthma occurring in the context of atopic dermatitis. 824
The management of patients with atopic dermatitis involves the use of several strategies: avoidance of provocation factors, the use of antimicrobial therapy in cases in which colonization of the skin with bacteria or yeasts has become problematic, and the use of emollients830 and topical corticosteroids. 608 These strategies, and also other treatments, will be discussed below.
Avoidance of potential allergens, and other provocation factors such as wool, 831 certain clothing dyes, and peanut protein-containing skin care products (that damage skin barrier function) is the first step in the management of atopic dermatitis. Silver-coated textiles have been used to control bacterial colonization of the skin. 832 Topical antibacterial agents have been used successfully in patients whose skin is colonized with bacteria.833. and 834. Antifungal therapy has been suggested for patients with head and neck disease in whom Malassezia are found in the skin. 778 While it may be beneficial in certain patients with head and neck disease, antifungal therapy was of no value in a double-blind trial in flexural atopic dermatitis. 835
The mainstay of treatment has been the combination of emollients (used immediately after bathing) with topical corticosteroids.836.837.838. and 839. The use of systemic anti-inflammatory therapy should be kept to a minimum. 840 Their use has been recently reviewed. 841 Some patients benefit from the use of antihistamines for the accompanying itch. 840
Because of the side effects of topical corticosteroids, particularly skin atrophy and telangiectasia, topical calcineurin inhibitors have been used as second-line therapy for head and neck disease in which atrophy has become troublesome.842.843.844. and 845. They have also been used for routine cases. 846 Tacrolimus and pimecrolimus should probably not be used for children under 3 years. 847 They can be quite effective in older children. 848 Tacrolimus ointment is effective in reducing flares when used as maintenance therapy. 849 So too is pimecrolimus cream. 850 A recent study concluded that there was no increased risk of malignancy or skin cancer associated with the use of these drugs as initially thought. 843
Infliximab monotherapy has been used in the treatment of refractory, severe atopic dermatitis but improvement was not maintained during maintenance therapy. 851 Another monoclonal antibody, efalizumab, produces clinical improvement with a decrease in the inflammatory infiltrate but further trials are needed. 852 Alefacept produced a response in only two of the nine patients in a recent trial. 853 High-dose intravenous immunoglobulin has also been used in severe resistant cases. 854 It is more effective in children than in adults, and when used as adjunctive rather than monotherapy. 854
Other therapies used have included leflunomide, recombinant interferon gamma, adjuvant UVA therapy, heliotherapy, 855 hypnotherapy, and probiotics. 832 Pulsed-dye laser treatment improves localized areas of chronic atopic dermatitis. 856 A prospective, randomized control trial found no beneficial effect from the intake of Lactobacillus rhamnosus. 857
Finally, the peroxisome proliferator-activated receptor ligand rosiglitazone (approved for the treatment of type 2 diabetes) has been used recently (2008) as adjunctive therapy in the treatment of severe disease, but further controlled trials are needed to establish its efficacy. 858
Atopic dermatitis presents the typical spectrum of acute, subacute, and chronic phases as seen in some other spongiotic (eczematous) processes. 861 As such, the biopsy appearances may be indistinguishable from those seen in nummular dermatitis and allergic contact dermatitis. Subtle features, to be listed below, may sometimes allow the diagnosis to be made on biopsy, although most often the dermatopathologist is restricted to describing the findings as ‘consistent with atopic dermatitis’.
Acute lesions show spongiosis and some spongiotic vesiculation, 862 even though some authorities deny the presence of spongiosis in atopic dermatitis. There is usually some intracellular edema as well, leading to pallor of the cells in the lower epidermis. 860 Exocytosis of lymphocytes is usually present, although it is never a prominent feature. There is a perivascular infiltrate of lymphocytes and macrophages around vessels of the superficial plexus, but there is no significant increase in mast cells or basophils in acute lesions. 860 The mast cells present are in different stages of degranulation, indicating activation of these cells. 718 Occasional eosinophils may be present.
Subacute lesions show irregular acanthosis of the epidermis with eventual psoriasiform hyperplasia. With increasing chronicity of the lesion, the changes of rubbing and scratching become more obvious and the spongiosis less so.
Chronic lesions show hyperkeratosis, moderate to marked psoriasiform hyperplasia and variable, but usually only mild spongiosis. Mast cells are now significantly increased in the superficial perivascular infiltrate.859. and 860. Eosinophils are also present. 863 Small vessels appear prominent due to an increase in their number and a thickening of their walls which involves both endothelial cells and the basement membrane. 860 Demyelination, focal vacuolation, and fibrosis of cutaneous nerves are also observed.859. and 860. Epidermal keratinocytes produce increased amounts of neurotrophin-4 in the chronic pruriginous lesions of atopic dermatitis. It may be responsible for the nerve hypertrophy that is sometimes seen. 864 Langerhans cells are increased in both the epidermis and the dermis.865.866. and 867. With further lichenification of the lesions, there is prominent hyperkeratosis and some vertical streaking of collagen in the papillary dermis, the changes recognized as lichen simplex chronicus. Collagen types I and III increase in the dermis following PUVA therapy. 868 Lichenified lesions have an increased number of mast cells in the dermis. 869
If dry skin is biopsied in patients with atopic dermatitis there is usually focal parakeratosis, mild spongiosis, and a mild perivascular infiltrate involving the superficial plexus. 870 There is focal hypergranulosis in those with dry skin alone, 871 but a reduced granular layer in those who have concurrent ichthyosis vulgaris. 870
The nature of the ‘angiohistiocytoid papules’ reported in two patients with atopic dermatitis from Japan is unclear. 872 They consisted of increased vascularity surrounded by histiocytoid cells that expressed factor XIIIa, but not CD68. 872
The rippled hyperpigmentation (‘dirty neck’) seen in approximately 2% of atopics results from melanin incontinence (see p. 299). Amyloid-like material has been seen on electron microscopy, but not on light microscopy, using the Congo red stain. 873
Infective dermatitis, a recently delineated entity in children and young adults, has similar clinical and histopathological features (see p. 630). It appears to be caused by infection with human T-lymphotropic virus type 1 (HTLV-1).
As already mentioned, there are several morphological features which, if present, favor the diagnosis of atopic dermatitis over the other spongiotic dermatitides which it closely resembles. The assessment of these features is somewhat subjective and, in some, it involves the use of techniques that are not routine. Features favoring the diagnosis of atopic dermatitis include prominence of small blood vessels in the papillary dermis, atrophy of sebaceous glands (this change is usually present only in those who have concomitant ichthyosis vulgaris), 870 and an increase in epidermal volume without psoriasiform folding of the dermoepidermal interface (Fig. 5.20). 874 This latter change is a useful clue to the diagnosis of atopic dermatitis. Eosinophils and basophils are usually more prominent in the infiltrate of allergic contact dermatitis than in atopic dermatitis. Despite this relative paucity of eosinophils in atopic dermatitis, eosinophil major basic protein has been reported in the upper dermis in a fibrillar pattern. 875 It may also be found at other levels of the dermis. 876 The diagnostic value of this feature requires further study, as do the findings of perivascular IgE877 and intercellular epidermal staining for IgE, HLA-DR, and CD1a in atopic dermatitis. 878 This also applies to the finding of a predominantly T-helper-cell (CD4+) infiltrate in atopic dermatitis866.867. and 879. and a T-suppressor-cell (CD8+) infiltrate in allergic contact dermatitis; 877 the latter finding does not accord with the results of other studies. 512
(A) Atopic dermatitis. (B) There is an increase in epidermal volume which is associated with only partial psoriasiform folding. Focal parakeratosis is also present. (H & E)
Papular dermatitis (subacute prurigo, ‘itchy red bump’ disease) presents as a pruritic papular eruption with superimposed secondary changes due to excoriation. 880 The lesions tend to be symmetrically distributed on the trunk, the extensor surfaces of the extremities, face, neck, and buttocks.
The etiology is unknown, although some patients have an atopic background. The earlier view that this may be a form of Cheyletiella dermatitis is no longer tenable (see p. 657).
There is variable epidermal spongiosis and focal parakeratosis. Excoriation and changes of rubbing and scratching are usually present. There is a mild superficial perivascular infiltrate of lymphocytes with a few eosinophils. These changes are not diagnostically specific, being present in other endogenous dermatitides.
Pompholyx (acral vesicular dermatitis, dyshidrotic eczema) is a common, recurrent, vesicular eruption of the palms and soles which is one of several clinical expressions of so-called ‘chronic hand dermatitis’.881. and 882. It consists of deep-seated vesicles, often with a burning or itching sensation, most commonly involving the palms, volar aspects of the fingers, and sometimes the sides of the fingers. 882 In one study, lesions were palmar in 70%, plantar in 10%, and palmoplantar in 20% of patients. 883 The mean age of patients in this series was 35 years (range, 7–72 years), and there was a slight female predominance. 883 Excluded from this series were cases with erythema associated with the vesicles (thus eliminating contact eczemas), and cases that did not exhibit a cyclic pattern of recurrent short-term attacks.159. and 883. Lesions usually resolve after several weeks, leading to localized areas of desquamation.
The term ‘dyshidrotic eczema’ was introduced because of a mistaken belief that the pathogenesis of this condition involved hypersecretion of sweat and its retention in the acrosyringia. 884 The term should be avoided. Pompholyx is a spongiotic dermatitis, the expression of which is modified by the thickened stratum corneum of palmar and plantar skin which reduces the possibility of rupture of the vesicles. Episodes may be precipitated by infections, including dermatophyte infections at other sites (‘id reaction’ –p. 115), 885 contact sensitivity to various allergens such as medicaments, shower gel, food (paprika, orange juice and crustaceans), mercury in amalgam fillings, 541 nickel, 885 chromium, and emotional stress. 886 Smoking is a rare triggering factor, 883 but it may have been responsible for four cases of painful lower leg ulceration that developed in patients with pompholyx. 160 In one series of 120 patients, 67.5% were regarded as allergic contact pompholyx, with cosmetic and hygiene products as the main factor, followed by metals. 883 Five patients in whom pompholyx was photoinduced have been reported. 887 About 15% of cases are idiopathic, but nearly all these patients are atopic.883.888. and 889.
Pompholyx is characterized by spongiosis of the lower malpighian layer with subsequent confluence of the spongiotic foci to form an intraepidermal vesicle (Fig. 5.21). The expanding vesicles displace acrosyringia at the outer margin of the vesicles. There is a thick, overlying stratum corneum, characteristic of palms and soles. Other changes include a sparse, superficial perivascular infiltrate of lymphocytes with some exocytosis of these cells. Some persons develop pompholyx-like vesicles that soon evolve into pustules with histopathological features of pustulosis palmaris (see p. 133). A PAS stain should always be performed on vesicular lesions of the palms and soles, particularly if there are any neutrophils within the vesicles or stratum corneum, as dermatophyte infections may mimic the lesions of pompholyx (Fig. 5.22).
Pompholyx. A unilocular vesicle is present within the epidermis. There is no spongiosis in the adjacent epidermis. (H & E)
Dermatophyte infection of the hands. There are only scattered neutrophils in the spongiotic vesicle, testimony to the necessity to keep a fungal infection in mind when the spongiotic reaction pattern is present on the hands or feet. (H & E)
Allergic contact dermatitis of the palms and soles may also be difficult to distinguish from pompholyx. In the former condition, mild spongiosis may be present adjacent to the vesicles, and there are sometimes eosinophils in the inflammatory infiltrate.
Little attention has been given in the literature to the significant number of patients who have an eczematous process that does not fit the criteria for any known type. Clinicians have usually used the term endogenous dermatitis (eczema) for these cases. As the histological appearances of many categories of spongiotic (eczematous) dermatitis are not characteristic of a specific disease process, particularly after treatment, and secondary changes such as scratching are taken into account, dermatopathologists have usually diagnosed ‘spongiotic dermatitis’. A recent (2008) report from China has reviewed 655 such patients with ‘unclassified eczema’. 890 The authors concluded that unclassified eczema is a common type of eczema with a very poor prognosis. 890 An accompanying Editorial titled ‘Addition of Nonspecific Endogenous Eczema to the Nomenclature of Dermatitis’ stressed that this was a diagnosis of exclusion. 891
A somewhat neglected entity, hyperkeratotic dermatitis of the palms (eczema keratoticum) is a clinical variant of chronic hand dermatitis.881. and 892.It presents as a sharply marginated, fissure-prone, hyperkeratotic dermatitis which is limited usually to the palms and occurs chiefly in middle-aged persons. 893 Involvement of the volar surfaces of the fingers is quite common. Plantar lesions are rare. The cause of the condition is unknown; some cases may be related to psoriasis. 893
Various treatments have been used including emollients, keratolytic agents, tar, topical corticosteroids in an ointment base combined with a keratolytic agent such as salicylic acid, or PUVA therapy. 893 Acritretin and etretinate have been used for refractory cases. 893
The appearances are those of a chronic spongiotic dermatitis with spongiosis and psoriasiform hyperplasia of the epidermis, although the elongation of the rete ridges is usually not as regular as in psoriasis. There is overlying compact orthokeratosis with small foci of parakeratosis. There is a moderately heavy chronic inflammatory cell infiltrate in the papillary dermis, predominantly in a perivascular location. Lymphocyte exocytosis is quite prominent in the epidermis, but there are usually no neutrophils. The amount of spongiosis allows a distinction to be made from psoriasis.
Juvenile plantar dermatosis is a condition which affects children between the ages of 3 and 14. 894 It presents as a shiny, scaly, erythematous disorder of weight-bearing areas of the feet. 895 Fissuring subsequently develops. Sometimes the hands, particularly the fingertips, are also affected. Most cases improve over the years.
The etiology is uncertain, with conflicting evidence on the role of atopy and of footwear.896. and 897.Dermatitis palmaris sicca is a related lesion of the palms. 898
Juvenile plantar dermatosis shows variable parakeratosis and hypogranulosis overlying psoriasiform acanthosis. A distinctive feature is the presence of spongiosis, mild spongiotic vesiculation, vacuolization of keratinocytes and exocytosis of lymphocytes, localized to the epidermis surrounding the acrosyringium. 895 Lymphocytes are present in the upper dermis around the sweat ducts at their point of entry into the acrosyringium. 895 Ducts and acrosyringia are not dilated. 899
A subacute spongiotic dermatitis has been recorded in several patients at the site from which a saphenous vein graft was removed. 901 There was a sensory peripheral neuropathy in the distribution of the dermatitis. Other changes reported at donor sites include the presence of localized myxedema in Graves’ disease, and the formation of an indurated linear plaque resulting from cutaneous sclerosis (see p. 316). Cellulitis of the lower leg is another complication.
Stasis dermatitis (hypostatic dermatitis) is a common disorder of middle-aged and older individuals. It is a consequence of impaired venous drainage of the legs. 902 In the early stages, there is edema of the lower one-third of the legs, which have a shiny and erythematous appearance. Subsequently, dry and scaly or crusted and weeping areas may develop. 902 Sometimes the changes are most prominent above the medial malleoli. Affected areas become discolored, due in part to the deposition of hemosiderin in the dermis. Ulceration is a frequent complication of stasis dermatitis of long standing. 902 Stasis dermatitis of the abdominal wall has been reported in the Budd–Chiari syndrome. 903 The patches of eczema that developed in a port-wine stain of the arm were regarded as analogous to stasis dermatitis. 904
Affected skin is unusually sensitive to contactants and, not infrequently, topical medications applied to these areas result in an eczematous reaction which can be quite widespread. This process of ‘autoeczematization’ is poorly understood (see below).
Stasis dermatitis is unlikely to be biopsied unless complications such as ulceration, allergic contact dermatitis or basal cell carcinoma arise. In stasis dermatitis, the spongiosis is usually mild, although spongiotic vesiculation may develop if there is a superimposed contact dermatitis. Focal parakeratosis and scale crusts may also be present.
The dermal changes are usually prominent and include a proliferation of small blood vessels in the papillary dermis. This neovascularization may lead occasionally to the formation of a discrete papule. There is variable fibrosis of the dermis which can be quite prominent in cases of long standing. Abundant hemosiderin is present throughout the dermis. It is not localized to the upper third of the dermis, as occurs in the pigmented purpuric dermatoses (see p. 233). The veins in the deep dermis and subcutis are often thick walled.
Autoeczematization (autosensitization) is characterized by the dissemination, often widespread and quick, of a previously localized ‘eczematous’ process. 906 The term is often used with less precision to apply to other autosensitization reactions, whereby an inflammatory dermatitis develops at a site distant to the original inflammatory process or insult. The term ‘id reaction’ has also been applied to this latter group, which now seems less common than previously.
Included in the broad concept of autosensitization/autoeczematization are the distant reactions to localized dermatophyte infections (e.g. pompholyx of the hands in response to dermatophyte infection elsewhere), to localized bacterial infections, scabies, burns and ionizing radiation, 906 and also to stasis dermatitis (see above). Generalization of a localized cutaneous eruption has been reported following the use of systemic prednisolone. 907 The development of recalcitrant eczema in patients with lymphoma or leukemia may result from a similar mechanism. 908 Some of the lesions that developed after an iguana bite were thought to represent autoeczematization. 909 The superantigen id reaction, as described by Crowson and Magro (see p. 193), was regarded as an immunological response to arthropathy-associated microbial pathogens. Although mostly resembling interstitial granulomatous dermatitis, some lesions were spongiotic.
The mechanism responsible for these reactions involves an abnormal immune response to autologous skin antigens. 910 Activated T lymphocytes appear to mediate this response.911. and 912.
The histopathological reactions have not been widely studied. In cases of dissemination of an originally localized process, the changes will usually mimic those seen in the initial lesions. In other instances, the generalized reaction is that of a spongiotic process of variable intensity. In the author’s experience, there has often been some edema of the superficial papillary dermis with some large (presumably activated) lymphocytes in the upper dermis. These two features may also be seen in spongiotic drug reactions (see p. 116) and dermal, systemic, and protein contact dermatitis (see p. 107). Dermal edema may also be seen in the pompholyx associated with this process of autoeczematization (see p. 114). However, when epidermal spongiosis is associated with subepidermal edema and a history of rapid generalization of an initially localized lesion, autoeczematization will usually be present (Fig. 5.23).
Autoeczematization. This case shows spongiosis and characteristic subepidermal edema. (H & E)
Papular acrodermatitis of childhood (Gianotti–Crosti syndrome) is an uncommon, self-limited disease of low infectivity characterized by the triad of an erythematous papular eruption of several weeks’ duration, localized to the face and limbs, mild lymphadenopathy, and acute hepatitis which is usually anicteric.913.914. and 915. The skin lesions are flat-topped papules 1–2 mm in diameter, which sometimes coalesce. An isomorphic response (Koebner phenomenon) is often present. 916 The lesions may be mildly pruritic. Hepatitis B surface antigen is often present in the serum.917.918. and 919.
It is now apparent that other viral infections, in particular infection with the Epstein–Barr virus,920. and 921. coxsackie virus A16, 922 parainfluenza virus, hepatitis A virus, 923 hepatitis C virus, 924 human immunodeficiency virus, 925 and cytomegalovirus, 926 are occasionally associated with a similar acral dermatitis;927. and 928. hepatitis and lymphadenopathy are not commonly present in these circumstances.927. and 928. Gianotti used the term ‘papulovesicular acrorelated syndrome’ for these cases.915. and 929. Although infections associated with these other viruses often pursue a longer course and may have tiny vesicular lesions, individual cases occur which closely resemble those associated with the hepatitis B virus. Accordingly, it seems best to group all these virus-related disorders under the term Gianotti–Crosti syndrome.
In the author’s experience, there is an increasing incidence of cutaneous reactions to viral and presumptive viral infections, ranging from those resembling Gianotti–Crosti syndrome at one end of the spectrum to others with histological features of mild pityriasis lichenoides. The clinical expression and distribution of these changes is somewhat variable, making the delineation of a specific clinicopathological entity a difficult task.
Although the changes are not diagnostically specific, they are often sufficiently characteristic at least to suggest the diagnosis. The appearances at low magnification often suggest that three tissue reactions – lichenoid, spongiotic, and vasculitic – are simultaneously present. 927 On closer inspection there is prominent exocytosis of mononuclear cells into the lower epidermis. This is usually associated with some basal vacuolar change, but cell death is not a conspicuous feature. 931 The spongiosis is usually mild, but small spongiotic vesicles, containing a few inflammatory cells and resembling those of pityriasis rosea, may be present (see above). Although most observers specifically deny the presence of a vasculitis, because of the absence of fibrin, 913 there is always a tight perivascular infiltrate of lymphocytes associated with variable endothelial swelling. In many instances the changes merit a diagnosis of lymphocytic vasculitis. 927 The inflammatory infiltrate not only fills the papillary dermis and extends into the epidermis, but it usually involves the mid and even the lower dermis to a lesser extent. There is often some edema of the papillary dermis. Epidermal spongiosis is less prominent in cases related to the hepatitis B virus.
Spongiotic reactions to drugs occur in several different clinical and pathogenetic settings, although in some instances the precise mechanism that results in the spongiosis is unknown (see Table 5.4). A delayed hypersensitivity response is usually suspected. 932 The three major categories of spongiotic drug reactions are provocation of an endogenous dermatitis, systemic contact reactions, and a miscellaneous group. Excluded from this discussion are the spongiotic reactions resembling pityriasis rosea produced by gold, 933 captopril124 and other drugs, the phototoxic and photoallergic reactions produced by a variety of drugs,934. and 935. and allergic contact dermatitis resulting from the topical application of various substances. Although there is mild spongiosis in the exanthematous (morbilliform) eruptions, these are histopathologically distinct from the other spongiotic reactions.
Reactions resembling seborrheic or nummular dermatitis have been reported following the use of latanoprost eye drops for lowering intraocular pressure, 538 and the ingestion of various drugs including cimetidine, methyldopa, 540 interleukin-2, 936 and antituberculous therapy. 540 The combination of interferon alfa-2b plus ribavirin, used in the treatment of hepatitis C infection, has also produced a generalized nummular dermatitis.539. and 937. This is assumed to be a provocation reaction in an individual with a predisposition to the development of an endogenous dermatitis. 540 An atopic dermatitis-like eruption has been precipitated by infliximab. 938 A reaction that mimics a spongiotic drug reaction has been reported in the complete DiGeorge syndrome. 939
Systemic contact dermatitis results from the administration of an allergen to an individual who has been sensitized to that agent by previous contact with it or with a related substance. 932 Systemic contact dermatitis may present as an exacerbation of vesicular hand dermatitis, as an eczematous flare at sites of previously positive patch tests, or as a systemic eczematous eruption with a predisposition for the buttocks, genital areas, elbow flexures, axillae, eyelids, and side of the neck. 940 The term ‘baboon syndrome’ was coined for this eruption. 940 This is an important category of spongiotic drug reaction in which numerous drugs have been incriminated. In some parts of the world inhalation of mercury vapor from a broken thermometer accounts for the majority of cases presenting as the ‘baboon syndrome’. 941 Other causes include antibiotics used topically as well as systemically, such as neomycin, erythromycin, 942 ampicillin, amoxicillin, 943 roxithromycin, 944 synergistins, 945 and gentamicin, as well as procaine, quinine, chloral hydrate, cetuximab, 946 cimetidine, 947 clonidine, minoxidil, codeine, disulfiram, thiamine, isoniazid, cinnamon oil, balsam, 948 hydroxyurea, 949 mercury vapor, 950 papaya juice, 951 ingested mango flesh, 952 aminophylline (crossreacting with ethylenediamine, a stabilizer in creams), 953 and certain oral hypoglycemic agents, diuretics and sweetening agents which crossreact with sulfonamides.940.954. and 955. Ingestion of derivatives of the lacquer tree (Rhus), used in traditional (folk) medicine, 956 and the intravenous infusion of immunoglobulins957.958. and 959. are two additional causes of systemic contact dermatitis. Zinc and other alloys in dental fillings are another cause.960. and 961. Metal sensitivity in patients with orthopedic implants is probably a related condition.962. and 963. It is becoming an increasing clinical problem. Patch testing before implantation may help guide the choice of device to be implanted. 964
The miscellaneous category of drugs producing the spongiotic tissue reaction undoubtedly includes agents that should be more appropriately included in other categories. For example, thiazide diuretics are usually included among the agents that produce photosensitive eruptions but it appears that, on occasions, an eruption is produced which is not confined to sun-exposed areas.965. and 966. Other drugs in this miscellaneous category include calcium channel blockers (such as nifedipine), 967 ACE inhibitors, 968 calcitonin, sulfasalazine, 966 indomethacin, 966 etanercept, 969 infliximab,938.970. and 971. epoprostenol, 972 fluoxetine (Prozac), 973 paroxetine (Aropax), allopurinol, 966 piroxicam, 974 tamoxifen, alcohol excess, 975 methadone, 976 and phenytoin sodium (sensitivity reaction). 977 The subcutaneous injection of heparin, semisynthetic heparinoids (such as danaparoid) or vitamin K1 may produce an eczematous plaque.978.979.980. and 981. Whenever treatment with the causative agent is continued, a generalized maculopapular rash may develop in addition to the localized plaque.982. and 983. Cross-reactivity to related agents is not uncommon. 982 The infusion of IL-2 or human immune globulin984 and the subcutaneous injection of either IL-6 or granulocyte-monocyte colony-stimulating factor (GMCSF) have been associated with a spongiotic tissue reaction.985.986.987. and 988. The palmoplantar erythrodysesthesia produced by various chemotherapeutic medications, most commonly doxorubicin, docetaxel, fluorouracil, and cytarabine, is usually mildly spongiotic. A similar reaction is produced by the epidermal growth factor receptor inhibitors such as sunitimib. 989 Interferon-alfa and ribavirin, used in the treatment of hepatitis C, may produce ‘eczema-like’ lesions;561. and 990. so too may smallpox vaccination. 991 Gold, in addition to causing a pityriasis rosea-like reaction, also produces an eczematous eruption which may last for up to 12 months after the cessation of gold therapy.992. and 993. Estrogen and progesterone (usually endogenous) have been associated with a spongiotic reaction (see below).994.995.996. and 997.
The incidence of spongiotic drug reactions is difficult to assess. Some reports make no mention of this type of reaction. One study reported that approximately 10% of cutaneous drug reactions were of ‘eczematous’ type. 998 In addition to generalized papules and eczematous plaques, a fixed eczematous eruption can also occur, the agents responsible usually being antibiotics.
By definition, there is epidermal spongiosis: this may occur at all levels of the epidermis. Spongiotic vesiculation is sometimes present. A characteristic feature is the presence of exocytosis of lymphocytes and occasionally of eosinophils. Often there is more exocytosis than would be expected for the amount of spongiosis in the region (Fig. 5.24). Rare Civatte bodies (apoptotic cells) are almost invariably present, but a careful search is usually necessary to find these cells (Fig. 5.25). Small spongiotic vesicles containing lymphocytes are a characteristic feature of pityriasis rosea-like eruptions. In exanthematous eruptions the spongiosis and exocytosis are confined to the basal layers of the epidermis in a rather characteristic pattern. 999 Other epidermal changes in spongiotic drug reactions include variable parakeratosis and, in chronic lesions, some acanthosis.
(A) Spongiotic drug reaction. (B) There is more exocytosis of inflammatory cells in spongiotic drug reactions than in most other spongiotic diseases. (H & E)
Spongiotic drug reaction.The spongiosis is minimal in this area of the biopsy. Note the exocytosis of lymphocytes and an apoptotic keratinocyte. (H & E)
The papillary dermis shows mild to moderate edema and there is a predominantly perivascular infiltrate of lymphocytes. Eosinophils are usually present, but this is not invariable. Some of the lymphoid cells appear to be larger than the usual mature lymphocyte. In a study of gold-induced reactions the lymphocytes were characterized as T-helper cells (CD4+). 993 Another feature of the infiltrate is its tendency to extend into the mid dermis, somewhat deeper than is usual with other spongiotic disorders. Red cell extravasation is sometimes present in the upper dermis. 993 Pigment incontinence is uncommon. Photospongiotic drug reactions are surprisingly common in Australia (Fig. 5.26). Thiazides and calcium channel blockers are often responsible for this pattern (see p. 535).
Photospongiotic drug reaction. (A) There is epidermal spongiosis and subepidermal edema. (B) There are many eosinophils in the perivascular infiltrate. (H & E)
Autoimmune progesterone dermatitis is a rare disorder characterized by recurrent cyclic eruptions during the luteal phase of the menstrual cycle.1000. and 1001. It presents as a pruritic, erythematous eruption with urticarial lesions, eczematous plaques, and erythema multiforme-like lesions. Pustular lesions have been described. Petechiae, palpable purpura, and dermatitis herpetiformis-like lesions are rare manifestations. 1002 The lesions resolve or partly improve after the menses. Lesions localized to the genital area have been described. 1001 Onset of the disease may be from the menarche to the fifth decade. Hormone therapy and infertility treatment may precipitate the disease. Some cases are worsened during pregnancy.
This condition is thought to be an autoallergic/delayed hypersensitivity reaction to endogenous progesterone. Provocation test with intramuscular or oral progesterone can be used. Positive skin tests result from the intradermal injection of progesterone. Serum progesterone antibodies are sometimes detected. 1002 Progesterone-sensitive interferon-γ-producing cells can be detected by the ELISpot assay. 1001
Treatment with estrogen preparations can be used.
Autoimmune progesterone dermatitis may show a range of histological appearances from a non-specific picture to one that mimics specific dermatoses such as erythema multiforme or urticaria. 1003 Epidermal spongiosis is commonly present with acanthosis and rare apoptotic keratinocytes as seen in other spongiotic drug reactions. There is a superficial perivascular infiltrate of lymphocytes, eosinophils, and sometimes neutrophils. The infiltrate is moderately heavy. Pigment-containing melanophages are often present in the papillary dermis.
Eruptions similar to autoimmune progesterone dermatitis have been reported in women secondary to a hypersensitivity reaction to exogenous or endogenous estrogen. Estrogen dermatitis was first reported by Shelley and colleagues in 1995. 994 Patients present with a cyclical exacerbation, before each menstrual period, of papulovesicular lesions, urticaria, eczematous lesions, or generalized pruritus. 1004 The diagnosis cannot be made without a clinical history. All patients have a positive skin test reaction to estrogens.
Treatment has been successful with a progestin-only pill. 1005 Antiestrogen therapy with tamoxifen can also be used.
The eczematous lesions are characterized by epidermal spongiosis with variable vesiculation depending on the severity of the process. 1004 There is subepidermal edema and a mild to moderately severe superficial perivascular infiltrate of lymphocytes and a few eosinophils. Urticarial lesions will usually be devoid of any spongiosis (Fig. 5.27).
Estrogen dermatitis. There is massive urticarial edema. There is no significant spongiosis. (H & E)
Chronic superficial dermatitis (persistent superficial dermatitis, small plaque parapsoriasis, 1006 digitate dermatosis1007) is characterized by well-defined, round to oval patches with a fine ‘cigarette-paper’ scale, usually situated on the trunk and proximal parts of the extremities.1006. and 1008. Individual lesions measure 2–5 cm in diameter, although larger patches, sometimes with a digitate pattern, may be found on the lower limbs, particularly the thighs. 1009 The lesions usually have a reddish-brown color, although the hue is yellowish in a small number of cases. 1010 The term ‘xanthoerythrodermia perstans’ was applied in the past to these latter cases.1007. and 1011.
Onset of the disease is usually in middle life and there is a male predominance. The lesions are mostly asymptomatic and persistent, although a minority clear spontaneously. 1012 Chronic superficial dermatitis, unlike large plaque parapsoriasis, with which it has been confused in the past, does not appear to progress to lymphoma, 924 despite the recent findings of a dominant T-cell clone in some cases. 1013 For various reasons, Ackerman and colleagues regard it as an early stage of mycosis fungoides.1014. and 1015. Others have called it an ‘abortive’ lymphoma1016. and 1017. or a distinct disorder ‘only weakly associated with mycosis fungoides’. 1018 Until the clinical significance of clonality and the chain of events leading to tumor progression are better understood, the true nature of this process will remain speculative. The risk of progression to mycosis fungoides is small.
Although chronic superficial dermatitis is classified with the spongiotic tissue reaction, it must be emphasized that in this condition the spongiosis is usually only focal and mild. There is usually focal parakeratosis or focal scale crust formation, implying preceding spongiosis. The epidermis is usually acanthotic and, in older lesions, there may be psoriasiform hyperplasia.
A mild infiltrate of lymphocytes and occasional histiocytes is present around blood vessels in the superficial plexus. Cells often extend high in the papillary dermis, a characteristic feature. Exocytosis of these cells is common, but mild (Fig. 5.28). There are no interface changes as in pityriasis lichenoides chronica and no atypical lymphoid cells as may occur in mycosis fungoides.
Chronic superficial dermatitis. The epidermis is only mildly spongiotic and there is focal exocytosis of mature lymphocytes into the epidermis. (H & E)
In 1990, Grosshans and Marot described an adult male with acquired, unilateral, relapsing inflammatory lesions, in a linear arrangement along Blaschko’s lines. 1019 The designations ‘acquired relapsing self-healing Blaschko dermatitis’ and ‘blaschkitis’1020 have since been applied. 1021 The etiology is unknown, but genomic mosaicism has been suggested as the explanation for the distribution. The histopathology is characterized by an acute or subacute spongiotic dermatitis with spongiotic vesiculation. 1021 It appears that lichen striatus and blaschkitis are related linear dermatoses forming a spectrum of lesions. 1022
Spongiosis can occur in the early stages of psoriasis associated with lymphocyte exocytosis. It can be seen in established lesions of psoriasis on the palms and soles, leading to difficulties in distinguishing these cases from allergic contact dermatitis. The presence of mounds of scale crust, regularly distributed within the cornified layer (akin to the mounds of parakeratosis containing neutrophils at their summits seen in psoriasis elsewhere on the body), is characteristic of psoriasis on volar surfaces. 13 There are multiple parakeratotic foci, arranged vertically, and alternating with orthohyperkeratosis. Spongiosis is often present in erythrodermic psoriasis, and in psoriasis of the flexures.
Rarely, an established case of psoriasis will show mild spongiosis, sometimes associated with features seen in the glucagonoma syndrome (see p. 489), such as mild epidermal vacuolation and intracorneal neutrophils.
Finally, there are rare cases of psoriasis in which mild spongiosis is a feature in initial and subsequent biopsies, so-called ‘spongiotic psoriasis’. The variants of psoriasis with spongiosis are listed in Table 5.5.
Epidermal spongiosis may be seen in photoallergic dermatitis (see p. 535), phototoxic dermatitis (see p. 533), the so-called ‘eczematous’ form of polymorphic light eruption, and certain persistent light reactions such as actinic reticuloid (see p. 539).
Photoallergic and phototoxic reactions are akin to allergic contact and irritant contact reactions respectively. They may be morphologically indistinguishable, although in some photoallergic reactions the inflammatory cell infiltrate extends deeper in the dermis. There is usually a superficial and deep perivascular infiltrate of lymphocytes in the papulovesicular form (so-called ‘eczematous’ type) of polymorphic light eruption. The epidermis shows variable spongiosis leading to spongiotic vesiculation.
Actinic reticuloid may have a mildly spongiotic epidermis. However, the diagnosis is usually made on the basis of the dense, polymorphous infiltrate in the upper dermis which includes some large lymphoid cells with hyperchromatic nuclei and stellate fibroblasts.
Dermatophyte infections can present with a spongiotic dermatitis, and clinically they can mimic a range of ‘eczematous’ dermatitides.
In addition to the spongiosis, the stratum corneum is usually abnormal, with compact orthokeratosis or parakeratosis sandwiched between orthokeratotic layers or the presence of neutrophils in the stratum corneum. Sometimes spongiotic pustules are present. The presence of neutrophils within the epidermis or stratum corneum warrants a careful search for hyphae, including the use of the PAS stain.
Epidermal spongiosis is a common finding in certain arthropod bite reactions, particularly scabies. Vesicles and rarely bullous lesions may develop in response to some arthropods. The spongiosis is usually of eosinophilic type (see p. 97), but certain beetles can produce neutrophilic spongiosis. Contact with moths of the genus Hylesia is said to cause vesicular lesions. Although not arthropod related, mention should be made here of cercarial dermatitis (see p. 646), which can mimic a bite reaction.
There is variable spongiosis, sometimes leading to spongiotic vesiculation. Bullae are uncommon (Fig. 5.29). Exocytosis of eosinophils through the epidermis may be present, but eosinophilic spongiosis is quite uncommon. The dermis contains a superficial and deep perivascular infiltrate of lymphocytes and eosinophils; characteristically, there are interstitial eosinophils.