Devices using radiofrequency (RF) energy and electrical energy to deliver a controlled thermal injury to heat skin have proliferated within the nonablative skin treatment market since the introduction of Thermage in 2002. By delivering continuous monopolar RF energy, rather than pulsed heating, and repeatedly bringing the skin to therapeutic temperatures until maximal contraction is obtained, the Pelleve Procedure can give obvious cosmetic results confluently over all treated areas painlessly and with no downtime. In this article, the technique, mechanism of continuous RF heating, and apparent treatment requirements to produce these results are presented. Some controversies are also addressed.
The use of thermal injury to rejuvenate and repair aging facial skin has been part of the nonsurgical skin treatment for decades. Ablative light-based energies, the gold standard being full carbon dioxide laser resurfacing, offered the potential for remarkable smoothing and moderate tightening at a superficial level but came with significant pain, downtime, healing complications, and unwanted pigment-related changes. To reduce the downtime and complications, lesser-ablative and nonablative wavelengths were devised, but consistent results were still dependent on having the proper skin type, dosing, and healing response. The advent of the use of radiofrequency (RF) energy represented a change away from light-based energy, dependant on generating heat by absorption of energy by a target chromophore.
High-frequency electron flow, RF, generates heat because of the differences in impedance between tissue types ( Fig. 1 ).
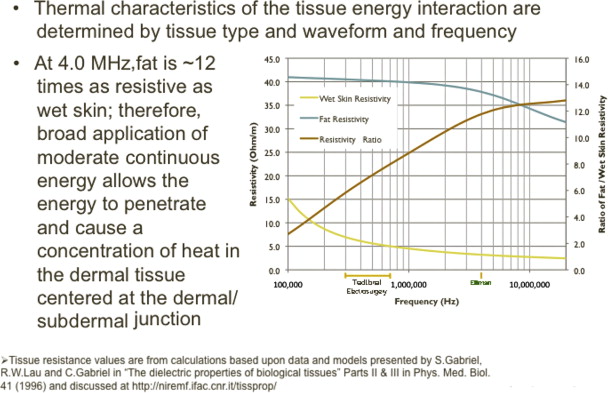
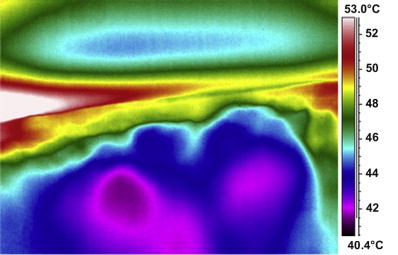
Streaming electrons flow through the low resistance of the epidermis and dermis and meet the highly resistant fat at the dermal-subdermal junction. The sudden change in impedance turns kinetic energy into thermal energy, and the surrounding tissues are heated. This method not only eliminates the problem of heating unwanted target chromophores in the skin, such as melanin, as seen with light-based lasers, but also allows the heat to be generated in the deep dermis where existing residual collagen bundles are most plentiful. Also present at the dermal-subdermal junction are the connections of subdermal connective tissue bands that run through the subdermal fat to the underlying fascia. A controlled thermal injury reaching the threshold temperature for denaturing collagen of 60°C to 65°C can cause contraction of the thinned collagen in the deep dermis immediately and trigger an inflammatory response that generates new collagen bundle reorganization and thickening evident at 12 weeks as seen on electron microscopy. Controlled thermal contraction down the deep connective tissue bands causes a vertical and 3-dimensional tissue contraction, compacting the fatty globules without injuring the fat itself ( Fig. 2 ).
This mechanism is in contrast to that of uncontrolled thermal injury in which temperatures obtained in deep tissue can reach or exceed 70°C, causing a necrotic injury, irregular wound contraction, fat loss, and atrophy, which has been reported with pulsed devices. Despite the potential benefits of deep RF dermal heating, the pain associated with the treatments and the inability to generate consistently predictable results continue to plague this technology.
The shortcomings of pulsed RF-based devices include the need to deliver a safe dose without crossing the heat threshold that results in tissue necrosis. To assure this safety, the treatment protocols are typically the same for all patients, not allowing customization of the dosing to improve treatment outcomes. However, it is obvious that not all skins respond equally to the same amount of energy, thus, the reputation for unpredictable results. Pulsed devices also raise the temperatures rapidly, which can cause pain and necessitates surface cooling to prevent superficial burns. However, without the control of the actual depth of cooling, favorable thermal effects on the dermis, such as wrinkle reduction, horizontal contraction, and shrinkage of pores, can be limited in thinned-skin individuals because of the excessive cooling of the middle to upper dermis. The need to optimize these treatment parameters of the myriad of devices available has been emphasized by many investigators who have evaluated the devices that have come into the market.
Mechanism of controlled thermal injury
The Pelleve procedure, performed using the 4.0 S5 Surgitron (Ellman International, Oceanside, NY, USA), differs from other methods of delivering RF energy because it delivers a progressive but controlled thermal injury to the dermis and subdermis and overcomes many of the shortcomings associated with pulsed and fixed dosed methods.
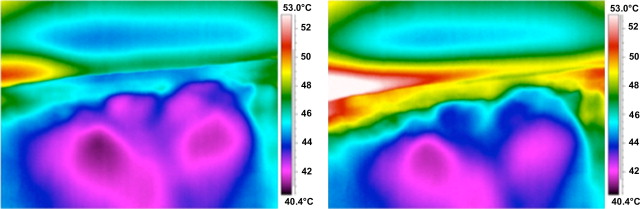
A 4.0-MHz high-frequency energy is used, so the difference in resistance between the dermal skin and underlying fat is maximal and results in heat generation and diffusion only from the dermal-subdermal junction. The energy delivery is continuous, but because of the constant movement of the electrode over the treatment area, heating is gradual, rather than sudden, allowing the procedure to be painless but thorough when performed properly. A dispersion gel is used on the skin to allow smooth movement of the electrode and immediate dispersion of the energy of the otherwise-focused flow of electrons. Because all the heat generated emanates from deep at the dermal-subdermal junction as seen on infrared images ( Fig. 3 ), no direct surface cooling is required and potentially beneficial effects to the middle and upper dermis are not compromised. In addition, because the heat conducted down connective tissue bands is also gradual and progressive, it has been demonstrated that the fat compartments are contracted, giving 3-dimensional deep tissue contraction without the fat cells reaching temperatures that could cause atrophy or necrosis.
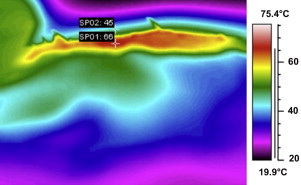
This process has been demonstrated in vivo ( Fig. 4 ). With progressive heating, the “cloud” of thermal energy rises up into the dermis and down the connective bands. Temperature levels at the surface have been documented to be approximately 20° cooler than those at the dermal-subdermal junction as seen in Fig. 3 .
The optimal threshold temperatures at, and adjacent to, the dermal-subdermal junction can be reached repeatedly in a controlled manner by monitoring the surface temperature and staying aware of the patient’s pain response, which correlates nicely with temperature levels and seems to be consistent from patient to patient.
It has been shown with the Thermage device (Solta Medical, Hayward, CA, USA) that multiple passes at lower energy levels produce more collagen contraction and new collagen production than single passes at higher energy levels.
With the gradual heating characteristic of the Pelleve procedure, the patient’s response to a threshold temperature of 40°C to 45°C at the surface correlates with a heat sensation of “just getting hot” or a heat perception level of 7 to 8 out of 10. An infrared surface temperature monitor can be used in addition to the patient’s feedback so that repeated passes can be preformed to the therapeutic threshold until clinically significant smoothing or tightening is seen in every patient without pain or unforeseeable jumps in temperature to dangerous levels. This subjective goal of repeating passes to threshold temperature until no additional contraction or smoothing is seen in each treatment session can be objectively stated to be 1 pass per decade of age plus or minus one pass depending on the anatomic area and the skin’s age and condition. In the case of the Pelleve procedure, a pass is defined as reaching threshold temperature confluently over the entire section being treated, not just covering the area with the probe passing over it, followed by forced cooling for 10 to 20 seconds. This procedure may take 30 seconds to a minute or more of persistently going over an area to bring it to the threshold temperature depending on energy output settings, the speed of the operator’s hand movement, and how much area is being treated at once. With experience, higher settings can be used comfortably and passes can be completed more efficiently, which reduces the overall treatment time. So again, a pass is defined as bringing the selected treatment area, that is, half the forehead, cheek, and periocular area, confluently to a threshold temperature of 40°C to 45°C and then cooling for 10 to 20 seconds, maximal 3-dimensional contraction is desired. One pass per decade of age plus or minus one pass in each area seems to be the amount of treatment in a given session to achieve clinically reliable and lasting results. One to 3 sessions may be required to achieve the desired degree of improvement that depends on multiple factors. These factors include age, degree of collagen loss, degree of volume loss, stage of volume loss, and genetic factors. Therefore, a session, single complete procedure, is the completion of the appropriate number of passes to all planned treatment areas. Clinically, it seems that each additional pass generates progressively greater contraction to a point to which no further benefit is seen or palpated, and this technique is what yields predictable results painlessly.
Cooling controversy
After several months’ experience, using multiple passes from 40°C to 45°C, going on to an adjacent area to allow spontaneous cooling of the treated area, and then returning to the treatment area, the possibility that the progressive swelling occurring with each pass might overcome the ability for acute tissue contraction became apparent. At that time, I began cooling the treated area directly with frozen reusable cold packs to force contraction of the solid proteins that were being heated and, at the same time, minimized the acute swelling associated with repeated heating. The immediate contraction and firming of the treated area was apparent, and it allowed repeated passes of continuing RF energy on the same areas until maximal contraction was seen without having to go to adjacent areas to allow passive cooling to occur. After only 20 to 30 seconds of cooling, the subsequent passes seemed to trigger an even more significant contraction without the swelling seen when letting the tissue cool passively. The distance between a point on the nasolabial fold and the tragus, for instance, increases after a pass of heat solely but decreases after a pass followed by cooling. The principle of physics governing cooling solids is that all solids, except water, contract with cooling. If application of cold causes even a fraction of a millimeter of additional contraction of the denatured collagen, then each subsequent pass would reach that much deeper and cause greater contraction and increase the density of the layers of deep dermal collagen. This occurrence is apparent on pinching the skin after each pass of hot and cold application.
Some investigators have suggested that heat shock proteins triggered by the injury could be adversely affected. It was shown that only cooling at or less than 5°C adversely affected the tissue’s response to injury, and cooling to that level is not advocated here.
To document what I have observed over the past several years, 10 consecutive patients were treated with one side heated to threshold temperature and then cooled for 30 seconds using an iced stainless steel roller and the other side of the face heated to threshold but left to cool passively while an adjacent area was treated. The midface was treated at a setting of 80 for 5 passes; the forced cooling for 30 seconds reduced the temperature to 20°C to 24°C. The opposite midface was treated at the same level for 5 passes but allowed to come to baseline temperature of approximately 33°C passively while an adjacent area was treated. The acute evaluation at the end of the treatment session and an evaluation 1 month later revealed significantly more contraction and lift on the side with cold applied for forced contraction at both end points. All 10 patients felt that the side with cold applied for forced contraction felt tighter at rest and felt denser when pinched relative to the passively cooled side. All patients were then treated the opposite way, and, at the end of the second month, all felt equally tight. The acute response at the end session was the same, the cooled side felt tighter and denser. All 10 patients also felt that the 2 treatments gave significant firmness and tightening to their skin, greater with the second treatment, and each could see an obvious contraction through the midface relative to their pretreatment photos.
Cooling controversy
After several months’ experience, using multiple passes from 40°C to 45°C, going on to an adjacent area to allow spontaneous cooling of the treated area, and then returning to the treatment area, the possibility that the progressive swelling occurring with each pass might overcome the ability for acute tissue contraction became apparent. At that time, I began cooling the treated area directly with frozen reusable cold packs to force contraction of the solid proteins that were being heated and, at the same time, minimized the acute swelling associated with repeated heating. The immediate contraction and firming of the treated area was apparent, and it allowed repeated passes of continuing RF energy on the same areas until maximal contraction was seen without having to go to adjacent areas to allow passive cooling to occur. After only 20 to 30 seconds of cooling, the subsequent passes seemed to trigger an even more significant contraction without the swelling seen when letting the tissue cool passively. The distance between a point on the nasolabial fold and the tragus, for instance, increases after a pass of heat solely but decreases after a pass followed by cooling. The principle of physics governing cooling solids is that all solids, except water, contract with cooling. If application of cold causes even a fraction of a millimeter of additional contraction of the denatured collagen, then each subsequent pass would reach that much deeper and cause greater contraction and increase the density of the layers of deep dermal collagen. This occurrence is apparent on pinching the skin after each pass of hot and cold application.
Some investigators have suggested that heat shock proteins triggered by the injury could be adversely affected. It was shown that only cooling at or less than 5°C adversely affected the tissue’s response to injury, and cooling to that level is not advocated here.
To document what I have observed over the past several years, 10 consecutive patients were treated with one side heated to threshold temperature and then cooled for 30 seconds using an iced stainless steel roller and the other side of the face heated to threshold but left to cool passively while an adjacent area was treated. The midface was treated at a setting of 80 for 5 passes; the forced cooling for 30 seconds reduced the temperature to 20°C to 24°C. The opposite midface was treated at the same level for 5 passes but allowed to come to baseline temperature of approximately 33°C passively while an adjacent area was treated. The acute evaluation at the end of the treatment session and an evaluation 1 month later revealed significantly more contraction and lift on the side with cold applied for forced contraction at both end points. All 10 patients felt that the side with cold applied for forced contraction felt tighter at rest and felt denser when pinched relative to the passively cooled side. All patients were then treated the opposite way, and, at the end of the second month, all felt equally tight. The acute response at the end session was the same, the cooled side felt tighter and denser. All 10 patients also felt that the 2 treatments gave significant firmness and tightening to their skin, greater with the second treatment, and each could see an obvious contraction through the midface relative to their pretreatment photos.
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree





