Increasing numbers of men are seeking aesthetic treatments for fat reduction, skin rejuvenation, and other antiaging goals. Compared with women, however, men have distinctly different anatomy and physiologic differences that manifest in the aging process. Given that both anatomy and the aging process affect treatment strategies and clinical outcomes, there is a need for dermatologists to be acutely aware of these male-specific nuances to provide the best clinical care and patient satisfaction.
Key points
- •
The aging process in men is mainly driven by the differences in androgens.
- •
Male skin is thicker, muscle mass is greater, and subcutaneous adipose tissue is thinner than that of women.
- •
Men are less likely to engage in preventative measures to limit the effect of extrinsic factor in their aging process.
Introduction
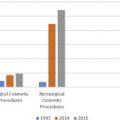
Once a female-dominated field, today aesthetics and the pursuit of youth are high priorities for men of all ages, ethnicities, and cultures. From over-the-counter gender-specific cosmetics to in-office cosmetic treatments, men are taking their appearance more seriously than ever. According to the American Society for Aesthetic Plastic Surgery, the number of cosmetic procedures performed on men has increased more than 325% since 1997, and in 2015 alone, men had close to 1.2 million procedures, making up 10% of the total number of plastic surgeries performed for the year. Statistics also reveal that men tend to seek mostly minimally invasive procedures with little or no downtime; between 2010 and 2014, the use of botulinum toxin in men increased by 84%, hyaluronic acid fillers increased by 94%, and intense pulse light treatments increased by 44%. Men and women are not created equal, however, when it comes to their motivations, goals, and their anatomy and relevant gender-specific pathophysiology that ultimately affect both treatment strategy and clinical outcomes. For the practicing dermatologist who treats this increasing male patient demographic, intimate knowledge of both anatomic differences of the male face and body and the factors underlying the pathophysiology of aging is critical for delivering the best clinical results.
Introduction
Once a female-dominated field, today aesthetics and the pursuit of youth are high priorities for men of all ages, ethnicities, and cultures. From over-the-counter gender-specific cosmetics to in-office cosmetic treatments, men are taking their appearance more seriously than ever. According to the American Society for Aesthetic Plastic Surgery, the number of cosmetic procedures performed on men has increased more than 325% since 1997, and in 2015 alone, men had close to 1.2 million procedures, making up 10% of the total number of plastic surgeries performed for the year. Statistics also reveal that men tend to seek mostly minimally invasive procedures with little or no downtime; between 2010 and 2014, the use of botulinum toxin in men increased by 84%, hyaluronic acid fillers increased by 94%, and intense pulse light treatments increased by 44%. Men and women are not created equal, however, when it comes to their motivations, goals, and their anatomy and relevant gender-specific pathophysiology that ultimately affect both treatment strategy and clinical outcomes. For the practicing dermatologist who treats this increasing male patient demographic, intimate knowledge of both anatomic differences of the male face and body and the factors underlying the pathophysiology of aging is critical for delivering the best clinical results.
Pathophysiology of aging in men
Aging regardless of gender is characterized by progressive changes associated with increased susceptibility to many diseases and is influenced by intrinsic (genetic) and extrinsic factors (lifestyle choices and environmental exposures). A study in twins found that genetics accounted for approximately 25% of the variation in longevity, and although environmental factors accounted for approximately 50%, with greater longevity (to age 90 or 100), genetic influences became more important. Several overarching physiologic principles characterize aging: loss of complexity as seen in less variability in heart rate responses, altered circadian patterns, loss of physiologic reserves needed to cope with challenges to homeostasis and compromised immune function that contributes to increased frequency of infections, malignancies, and autoimmune disorders, ultimately leading to a chronic, low-level inflammatory state. In men, a key factor that contributes to the sexual dimorphism observed with aging is the decline of testosterone (as rapidly as 0.4%–2% annually after age 30 years). Because testosterone has a critical role in the modulation of adult male reproductive health, sexual function, bone health, fat metabolism, and muscle mass and strength, its declining levels have male-specific repercussions during the aging process. Moreover, as opposed to women, who are equipped with innate antioxidant protection due to the presence of estrogen that mediates the expression of superoxide dismutase and other antioxidant molecules, men are more susceptible to the action of free radicals and suffer from higher levels of oxidative stress. These intrinsic factors together with the environment and lifestyle choices affect every organ system in men. Compared with women, men experience a steeper decline in pulmonary and aerobic function with age; studies have shown 3% to 6% decrease in peak aerobic capacity per decade in the 30s and more than 20% decrease in peak aerobic capacity per decade in the 70s and beyond.
The effects of aging on the skin are the most revealing of a person’s age, and studies have shown that men generally appear older than they actually are compared with women. The male epidermis and dermis are thicker than those of women, with higher density of hair follicles, greater sebum and sweat production, and an increased ratio of muscle to subcutaneous tissue. Due to the thicker skin and prominent facial musculature, the loss of subcutaneous adipose with age results in deeper expression lines in men compared with women, who typically develop superficial rhytides. Because androgen levels decline during aging, skin changes, with atrophy, decreased elasticity, and impaired metabolic and reparative responses the main manifestations. The epidermis becomes thinner and the dermoepidermal junction flattens, resulting in increased fragility of the skin to shear stress, decreased nutrient transfer, compromised skin barrier function of the skin, and redistribution of hair follicle. As androgens convert vellus into terminal hairs, androgen-dependent areas (chin, upper lip, chest, breasts, abdomen, back, and anterior thighs) subsequently exhibit increased vascularity; as a result, decline of hormones during aging contributes to particular atrophy in those areas. Changes in the glycosaminoglycan macromolecules in the dermis lead to loss of hydration and decreased skin resilience and the decrease in subdermal fat. This loss of support contributes to the skin wrinkling and sagging as well as to increased susceptibility to trauma.
As individuals age, muscle mass decreases in relation to body weight by approximately 30% to 50% in a nonlinear manner, that is, the loss is accelerated with advancing age. One major cause of this muscle mass loss is the decline of anabolic hormones, such as testosterone, dehydroepiandrosterone, and growth hormone, which results in a katabolic effect on muscles and bones. Although men have significantly more skeletal, facial mimetic and fat-free muscle mass compared with women, studies have reported a decreased muscle protein synthesis rate in older men compared with women with similar age/weight. This decreased muscle function affects the male metabolism and lends susceptibility to increased accumulation to adipose tissue. Moreover, the loss of facial muscle mass and function with aging manifests in deep lines in men and a different wrinkle pattern.
The proinflammatory environment together with the loss of minerals and change in hormones leads to increased probability of bone fractures and slower rate of repair, once fracture occurs. Bone loss has physical consequences in the face, because it provides the structural framework where soft tissues rest; men have prominent supraorbital ridges, greater glabellar projection, larger orbital size, and a wider chin contributing to the angular features of the aging male face. With bone loss in the aging face, there is ptosis of tissues manifesting as undesirable sagging that motivates men for aesthetic interventions.
Fat mass and adipose tissue are also influenced by age in a gender-specific way. Body fat is redistributed and accumulates in the trunk and lower body while subcutaneous adipose tissue decreased. Although men have less fat than women (10% to 15% in men compared with 18% and 20% in women of body weight), during aging its distributed more specifically in the abdominal region, lending susceptibility to cardiovascular disease and diabetes. In the face, men have a distinctly different adipose compartment distribution compared with women. The subcutaneous adipose layer is thinner overall and in areas, such as the malar areas, 3-D CT studies have demonstrated that men have less soft tissue and as much as 3 mm less subcutaneous tissue compared with women. Moreover, the ratio of medial to lateral cheek thickness is 1.5:1 in women and 1.1:1, which clinically manifests as the flat and angular malar regions of men. In other facial regions, such as the orbital region, the orbital fat is larger compared with women, and depletion of the orbital fat pads with aging leads to lower eyelid prominence.
Extrinsic factors, lifestyle choices, and environmental exposures accelerate the aging process. Prolonged and repeated exposure to solar radiation leads to premature skin aging, known as photoaging, that superimposed on the changes caused by chronologic aging is responsible for most of the age-associated features of skin appearance. The mechanisms underlying the UV-mediated damage to the skin connective tissue involve the formation of reactive oxygen species (ROS), cell surface receptor-initiated signaling, protein oxidation, and mitochondrial damage. Salient clinical features of photoaging include fine and coarse wrinkles, dyspigmentation, actinic keratoses, telangiectasias, and loss of elasticity. Sun-induced cutaneous changes vary among individuals, depending on age, gender, geographic location, and skin type, reflecting intrinsic differences in vulnerability and repair capacity. Male gender has been shown a risk factor for photoaging for behavioral and biological reasons. Although photodamage can be partially prevented and reversed with proper sun protection (sunscreens and protective clothing), men tend not comply to these measures. One study found that 41% of men never apply sunscreen. A recent multicenter cross-sectional study using a population-based survey of 416 individuals over the age of 18 years showed that men were more than twice less likely to put on sunscreen every day compared with men. The reduced innate antioxidant capacity of men’s skin translates into increased susceptibility to the catastrophic consequences of ROS accumulation. Beyond the undesirable cosmetic effects, the increased incidence in men of skin cancer, both benign and malignant, stand testament to the detrimental impact of photoaging.
Tobacco use is another lifestyle factor that accelerates the aging process, and men hold the lead when it comes to smoking. In 2012, the worldwide prevalence of smoking in men was 31.1% and 10.6% in women, while, according to the latest statistics, the age-standardized prevalence of daily smoking was 25% for men and 5% for women. Smoking has detrimental effects to many organs because it contains several carcinogenic compounds and is a known cause of several diseases, such as cancer, asthma, and so forth. Smoking also has profound effects on the skin and aggravates cutaneous aging. A clinical study found cigarette smoking an independent risk factor for the development of accelerated facial wrinkling and that the risk was dose dependent to smoking exposure. Although the mechanism via which smoking affects the skin is not completely understood, factors include vasoconstriction, increased oxidative damage, and altered connective tissue metabolism. Peripheral blood flow decreases by 30% to 40% within minutes after smoke inhalation, compromising tissue oxygenation, whereas inhibition of fibroblast activity and up-regulation of matrix metalloproteinase leads to decreased collagen synthesis and accumulation of ROS. Smoking is strongly associated with the development of facial elastosis and telangiectasias in men. Elastotic skin is less elastic, dryer, darker, and more erythematous than normal skin.
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree