Medial sural artery perforator (MSAP) flap is a thin, pliable, and versatile flap. It is a fasciocutaneous flap with chimeric design capacity. The donor site permits the synchronous harvesting of nonvascularized tendons and nerves. Free MSAP flap is suitable for foot, ankle, and distal one-third of the leg reconstructions. Pedicled MSAP flap is an alternative flap for knee and proximal two-thirds of leg defects, covering classical lower limb reconstruction territories of soleus, medial, and lateral gastrocnemius muscle flap. Computed tomography angiography, indocyanine green, and endoscopic-assist dissection enhances MSAP flap surgical planning and reduces its technical adversities and complications.
Key points
- •
MSAP flap is thin and pliable with moderate pedicle length. It is suitable for small to medium-sized defect reconstructions of the lower limb.
- •
MSAP flap is raised as a pedicled or a free flap for locoregional and distant defect reconstructions and is a workhorse flap capable of reconstructing all anatomic regions of the lower limb.
- •
CTA, Doppler, indocyanine green, and endoscopic-assisted dissection enhance MSAP flap surgical planning and reduce technical adversities and complications secondary to anatomic variations.
- •
Tourniquet-assisted dissection, meticulous hemostasis, and high pedicle division above the bifurcation of medial sural artery lessen the risk of arterial spasm and reduce anastomosis challenges.
Introduction
Meticulous evaluation of tissue defect components in lower extremity reconstruction is the essence of achieving satisfactory functional and aesthetic outcomes. Recent technical refinements of perforator flaps and diverse donor site availabilities permit tailored reconstruction while minimizing donor site morbidity. The medial sural artery perforator (MSAP) flap is a relatively new flap. As first described in 2001, MSAP flap was primarily indicated for lower limb reconstruction. , The versatility of the MSAP flap accompanies its growing popularity. It is thin and pliable with predictable vascular anatomy. It is raised either as a free flap or a pedicled perforator flap and used predominantly as a fasciocutaneous flap.
Comparing with the anterolateral thigh (ALT) flap, the MSAP flap has shorter pedicle, and perforators are embedded more superficially in medial gastrocnemius muscle. Thus, the intramuscular dissection is less demanding and less traumatic. Like the ALT flap, the MSAP flap can also be harvested as a chimeric flap, providing much-needed volume for the desired reconstruction.
The MSAP flap can be raised with an applied tourniquet, aiding an advantage over the ALT with the bloodless surgical field during dissection. Claimed challenges of this flap consist of anatomic variations, extended intramuscular dissection, and potential donor site morbidity. Preoperative computed tomography angiography (CTA), Doppler-assisted perforator mapping, endoscopic-assisted perforator visualization, and indocyanine green fluorescence imaging enhance MSAP flap surgical planning and reduce technical adversities and complications secondary to anatomic variations. This article describes the versatility of pedicled and free MSAP flaps for lower extremity reconstruction. Surgical indications, specific considerations, and surgical steps of MSAP flap are also examined and explored in detail.
Indications and contraindications of medial sural artery perforator flap transfers
The choice between pedicled and free MSAP flap is based on anatomic regions. Parallel to pedicled medial gastrocnemius flap, pedicled MSAP flap is indicated for knee and the proximal third of the leg reconstructions. In pedicled MSAP flap, the skeletonized vascular pedicle extended the range of flap advancement with a greater arc of rotation. These features enable MSAP flap coverage to the lateral knee and the middle third of the leg, which are traditionally unattainable with pedicled medial gastrocnemius muscle flap. MSAP flap is one of the most effective flaps for small to medium-sized defect reconstructions at all regions of the lower extremity.
The main indication for free MSAP flap in lower extremity reconstruction is resurfacing of the ankle and foot defect with exposed tendon or bone/metalware. These regions generally require a thin and pliable flap to restore the contour so that patients may comfortably wear shoes. In the rare scenario, the chimeric MSAP flap with the inclusion of partial medial gastrocnemius muscle is applied to obliterate dead spaces or augment missing tissue volume, either as a free or a pedicled flap.
The MSAP flap is contraindicated in trauma involving the proximal tibia or medial gastrocnemius muscle because the perforators may be within the zone of injury. Also, hematoma and bruise on the muscle may interfere with the precise identification of the perforator and intramuscular dissection ( Box 1 ).
- •
MSAP chimeric flap is indicated for bone and metalware coverage, and dead space obliteration.
- •
Pedicled MSAP flap is an alternative flap for knee and proximal two-thirds of leg defects.
- •
Free MSAP flap is suitable for foot, ankle, and distal one-third of the leg reconstructions.
- •
MSAP flap is contraindicated with trauma involving proximal tibia or medial calf.
Preoperative evaluation and special considerations
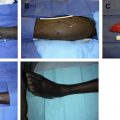
Preoperative CTA is recommended for preoperative mapping of MSAP flap vascular anatomy. CTA can identify vascular injuries and variations, and delineate the relationships between perforators and skin paddles. CTA can also map the vascular branching patterns and detect the depth, directions, and intramuscular course of the perforators. This is crucial information for surgical planning and flap design, especially if a chimeric flap is indicated ( Fig. 1 A). In the rare scenario, when medial sural artery anatomy is unfavorable for MSAP flap, CTA also facilitates the design of an alternative flap preoperatively as a backup procedure ( Fig. 1 B).
In our study, the MSAPs were found between 6 and 15 cm from the popliteal crease, and the average number of the perforators is 1.4 (1–3 perforators; n = 1 [34], n = 2 [16], n = 3 [2]). Similar to the study by Hallock, most of the vascular pedicles are located superficially within medial gastrocnemius muscle. The upper limit of the flap size in this series measured 15 × 9 cm 2 . The average pedicle length was 11.0 cm, with a maximum length of 20 cm.
Surgical procedures
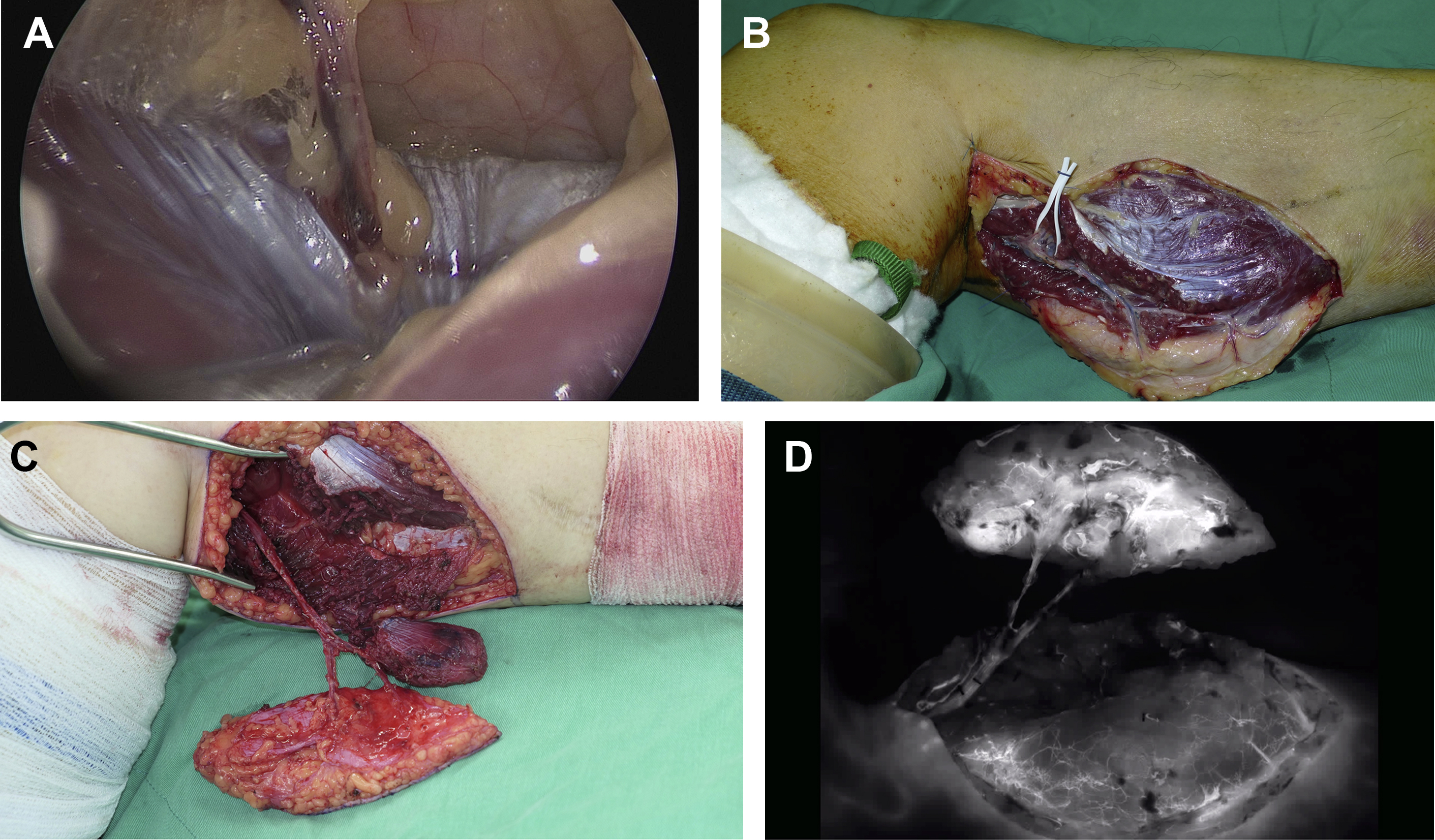
Patients were positioned in supine with abducted and externally rotated hip, and 90° flexion of the knee. Tourniquets were routinely used on the thigh. A line was drawn between the midpoint of the popliteal crease and the medial malleolus. Candidate perforators were located by handheld pencil Doppler centered over the drawn line over the midcalf. , In some of our cases, endoscopy was used to visualize the perforator locations, facilitating the design of the skin paddle ( Fig. 2 A).
Raise of a Fasciocutaneous Flap
The first skin incision was made over the anteromedial border of the designed skin paddle down to the fascia. Everting the anteromedial flap edge with gentle traction facilitates subfascial dissection and perforator identification. Because the Doppler signals of the perforators are loosely correlated with the actual perforator locations, once the perforators were identified, fine design adjustment of the MSAP flap may be needed. The chosen perforators were traced back to the medial sural artery pedicle through retrograde intramuscular dissection. The vascular pedicle was routinely traced proximally to the bifurcation of medial sural artery, because its caliber reduced abruptly after its division. This step permits the inclusion of vessels with greater caliber, reduces the risk of vasospasm, and lessens the technical challenge of the microvascular anastomosis. The posterolateral boundary of the flap was left undivided until sufficient pedicle length was yielded. This step prevents accidental perforator traction, twisting, or kinking during intramuscular dissection ( Fig. 2 B).
Raise of a Chimeric Flap
The fasciocutaneous flaps were raised mostly based on the lateral branch of the medial sural artery in our patient population. Thus, when designing a chimeric MSAP flap with gastrocnemius muscle, the muscle component was based either on the medial branch or the distal runoff of the lateral branch ( Fig. 2 C). The muscle component of the chimeric flap is designed with 1 to 2 cm of the skeletonized pedicle to enhance the degree of freedom during flap inset.
Raise of a Pedicled Flap
There are four types of pedicled MSAP flap designs to accommodate different defect sizes and locations: (1) propeller flap, (2) peninsular flap, (3) advancement flap, and (4) proximally based island flap. Accurate mapping of the perforators is critical for pedicled MSAP flap design and its subsequent success. Skeletonizing the pedicles from meticulous intramuscular dissection significantly increases the pedicle length, enhances the flap advancement, and inset flexibility. Thus, it strengthens the versatility of the pedicled flap.
Harvest of Adjacent Tissue Components
Anatomically, medial sural artery territory is surrounded by various useful donor tissues and structures. From the same donor site, tendon grafts are harvested from plantaris tenon between the medial gastrocnemius and soleus or from a split Achilles tendon. In addition, saphenous and sural nerve grafts can also be harvested via the same incision site. In our series, three flaps were raised with plantaris tendon grafts for simultaneous reconstruction of extensor hallucis longus (EHL).
Intraoperative Indocyanine Green Fluorescence Imaging
Indocyanine green fluorescence imaging is routinely used in the author’s practice. It examines the native perfusion of the flap and its angiosomes and assesses remnant muscular perfusion of medial gastrocnemius muscle ( Fig. 2 D). If generalized reduction in native flap perfusion is present, it prompts a re-examination of vascular pedicle before its division. If regional perfusion insufficiency was detected, the concerned tissue could be discarded to prevent postoperative flap necrosis.
Donor Site Management
The donor site was closed primarily (67.3%; n = 35), skin grafted (15.4%; n = 8), or via delayed primary closure with shoelace technique (17.3%; n = 9). In our experience, a 6-cm flap width is the cutoff for primary closure.
Postoperative care and expected outcome
Patients with free MSAP flap were routinely admitted to the microsurgical intensive care unit for 3 to 5 days of flap monitoring and postoperative care. No routine postoperative anticoagulant was given. Intensive flap monitoring prompts early detection, and timely re-exploration is the key to successful free flap salvage. This is particularly relevant in flaps with venous insufficiency, which is the main cause of re-explorations. In addition, the rehabilitation program starts a few days after surgery to reduce recovery delay. All of the patients were discharged with regular outpatient follow-up. In our series, the incidence of flap re-exploration showed no significant difference in patients with different age, gender, comorbidities, and timing of reconstruction after trauma.
A retrospective study was conducted for examining all patients who received MSAP flaps for lower extremity reconstruction at Chang Gung Memorial Hospital from 2007 to 2019. Fifty-two flaps were performed in total: 47 were fasciocutaneous flaps, and five were chimeric flaps incorporating medial gastrocnemius muscle. The chimeric flap was indicated for bone and metalware coverage and dead space obliteration. Among these 52 MSAP flaps, 17 were pedicled, and 35 were free flaps. In this series, knee and proximal two-thirds of the leg were reconstructed with pedicled flaps, whereas the distal third of leg (n = 3), ankle (n = 3), and foot (n = 29) were reconstructed with free flaps. Reflectively, among those 17 pedicled MSAP flaps, eight were used for knee reconstructions, four for the proximal third of the leg, and five for the middle third of the leg.
Durable soft tissue coverage without tendon/bone/metalware exposure was achieved in all patients receiving MSAP flaps. Early mobilization and physical therapy promoted optimal functional recovery of the injured extremities.
Management of complications
Surgical complications within 3 months were recorded. Data points included microvascular complications, compromised wound healing, hematoma, and wound dehiscence. Donor site morbidities were also documented.
In the pedicle flap group, the survival rate was 94.1% (16/17) as opposed to 100% in the free flap group. In this series, there were four free flap re-explorations because of venous congestion, which were all successfully salvaged. There was one complete flap failure in the pedicled group, and the defect was subsequently reconstructed by propeller ALT tensor fascia lata flap. There were two partial necroses in the pedicled group, which were managed with successive debridement and skin graft. No significant donor site morbidity was observed.
Revision or subsequent procedures
Most commonly performed revision procedures after lower extremity reconstruction with MSAP flap were single-stage flap debulking surgery (n = 12), scar revision (n = 7), and tenolysis (n = 5). All the debulking procedures were performed for patients with foot reconstruction to enhance the fitting of their shoewear.
Case demonstrations
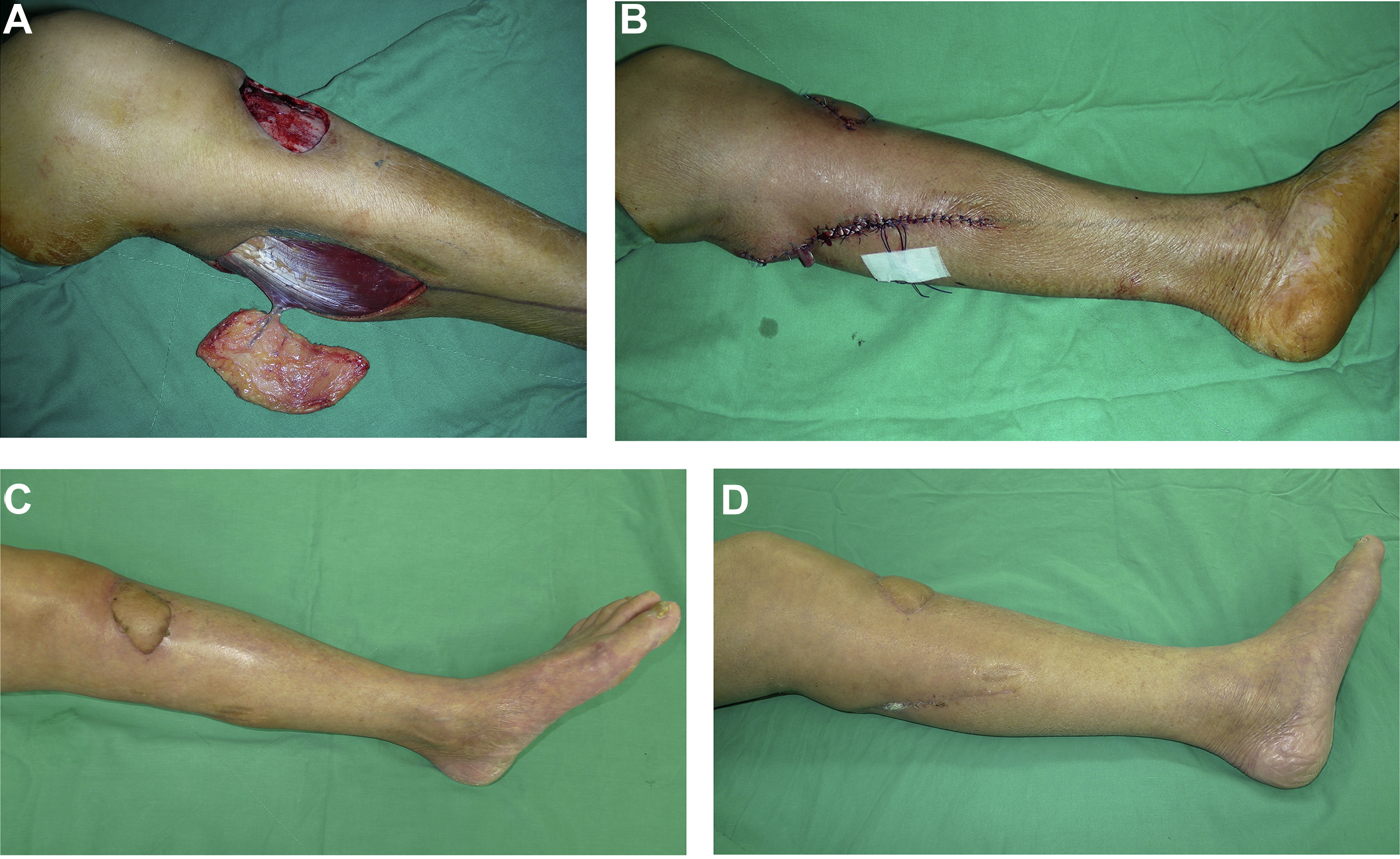
Case 1: Pedicled Medial Sural Artery Perforator Flap
A 69-year-old man was referred for necrotic left pretibial wound from a fall into a ditch. Judicious wound debridements resulted in an 8 × 6 cm 2 soft tissue defect with the exposed proximal tibia. A pedicled MSAP flap was raised based on a single perforator. The size of the flap was 13 × 7 cm 2 , with an 8-cm pedicle length. The flap was delivered to the defect through a subcutaneous tunnel. Donor site closure with shoelace sutures allowed dynamic wound closure to minimize pedicle compression from postoperative swelling. At 1-month follow-up, a sturdy pretibial wound coverage with aesthetically acceptable outcome was attained ( Fig. 3 ).