Antibiotics are commonly used by dermatologists in clinical practice, primarily because of the overall track record of favorable efficacy and safety with the most commonly used agents. During the past decade, increased attention has been given to the problems associated with antibiotic resistance. This article summarizes important principles gleaned from the continued efforts of the Scientific Panel on Antibiotic Use in Dermatology; other groups working diligently in this area, such as the Centers for Disease Control and Prevention and the Canadian Antimicrobial Resistance Alliance; and from the published literature.
Key points
- •
The use of oral or topical antibiotics induces selection pressure, which favors the persistence of bacteria that are less sensitive to the antibiotic administered, and sometimes to other similar antibiotics that are susceptible to cross-resistance mechanisms.
- •
The emergent antibiotic-resistant bacteria may include commensal flora and transient pathogenic flora, including Staphylococcus aureus and Streptococcus pyogenes .
- •
In management of acne vulgaris, use of oral and topical antibiotics as monotherapy is not recommended. Concomitant use of benzoyl peroxide (BP) can reduce the emergence of antibiotic-resistant Propionibacterium acnes strains. This occurs only at anatomic sires where BP is applied and does not reduce emergence of resistant bacteria exposed to antibiotic in the mouth, gastrointestinal, and genitourinary tracts.
- •
Overall reduction in prescribing of specific antibiotics and classes in a geographic community correlates directly with a decrease in the prevalence of resistant bacterial strains.
- •
Subantimicrobial dosing of doxycycline has been shown to exhibit anti-inflammatory properties, which seem to at least partially explain efficacy in papulopustular rosacea. Efficacy and safety in patients with papulopustular rosacea and AV, and lack of antibiotic selection pressure are supported by a large body of scientific evidence.
Major premise #1: dermatologists are the most common prescribers of antibiotic therapy in the United States
Principle #1: Antibiotic therapy is most commonly used by dermatologists to treat noninfectious inflammatory dermatoses, such as acne vulgaris (AV) and rosacea.
Principle #2: Durations of therapy with antibiotic use for many inflammatory dermatoses are often prolonged over several weeks to months.
Principle #3: Antibiotic resistance is a consistent and unavoidable adverse effect associated with systemic and topical antibiotic use. The emergence of serious infections caused by bacteria that are highly resistant to many previously effective antibiotics necessitates that all clinicians consider when an antibiotic truly needs to be used and to prescribe judiciously.
Topical and oral antibiotics are commonly used by dermatologists in clinical practice, primarily because of the overall track record of favorable efficacy and safety with the most commonly used agents (ie, tetracyclines, macrolides). Among categories of physicians in the United States including primary care and specialty areas, dermatologists prescribe more oral antibiotics per practitioner than any other physician group based on data collected by the US Centers for Disease Control and Prevention (CDC). The types of antibiotics that are commonly prescribed also differ among dermatologists compared with other physician types, with approximately three-fourths of all oral antibiotic prescriptions in the United States being written for a tetracycline agent (usually doxycycline or minocycline). The higher frequency of oral antibiotic prescribing and the differences in the types of antibiotics used by dermatologists compared with other physicians are because dermatologists commonly use tetracycline agents to treat common inflammatory skin diseases, especially AV and rosacea. Importantly, when oral antibiotics are used to treat AV and rosacea, they are frequently administered for prolonged durations of therapy over several weeks to months, compared with short courses used to treat common infections, such urinary tract infections, upper respiratory tract infections, otitis media, and uncomplicated skin/soft tissue infections. The use of oral antibiotic therapy to treat AV, especially the tetracycline agents doxycycline and minocycline, remains part of published guidelines on the management of AV, and is also included among recommended therapies for treatment of papulopustular rosacea. Because antibiotic resistance is an unavoidable sequelae of their systemic or topical administration, it is important that all clinicians take this into account when considering use of and selecting antibiotic therapy.
Over the past decade, increased attention has been given to the problems associated with antibiotic resistance, especially with the emergence of methicillin-resistant Staphylococcus aureus , macrolide-resistant staphylococci and streptococci, and hospital-based pathogens, such as enterococci and Clostridium difficile , which have acquired antibiotic resistance patterns that create major therapeutic challenges. In addition, the marked decrease over the past few decades in development of antibiotics, especially new drug classes, has been a major impetus for concern. The progressive increase in concerns and challenges related to antibiotic resistance has been felt globally, with many campaigns developed by several societies and government agencies to promote more prudent prescribing, reduce unnecessary antibiotic use, and increase surveillance and detection of emerging resistance patterns within hospitals and their surrounding communities. In the United States, major steps were put into motion approximately a decade ago by the CDC with initiatives to decrease antibiotic prescribing (especially for upper respiratory tract infections that are often caused by viruses) and by the Food and Drug Administration with changes in approved product labeling with most antibiotics that attempt to address optimal antibiotic use.
Despite all of the publicity in the medical literature and in the lay press (including the Internet) about antibiotic resistance concerns, the true “wake up call” in dermatology came with the emergence of skin infections caused by community-acquired methicillin-resistant S aureus . Once community-acquired methicillin-resistant S aureus surfaced in the United States, skin infections caused by methicillin-resistant S aureus were seen by dermatologists in their offices on a daily basis, or at least several times each week or month. Having these cases in front of them on a regular basis, and seeing first hand cutaneous infections cause by strains of S aureus that are resistant to commonly used antibiotics (penicillins, cephalosporins, macrolides, clindamycin) brought greater attention among dermatologists to the clinical relevance of antibiotic resistance beyond just the hospital environment. Nevertheless, many questions remain within the general dermatology community regarding how the use of topical and oral antibiotics by dermatologists contributes to the overall impact of antibiotic resistance and whether the resistance patterns that are created are truly relevant clinically.
The first dedicated group within dermatology in the United States to formally address the subject of antibiotic use and the potential implications of antibiotic resistance in dermatology is the Scientific Panel on Antibiotic Use in Dermatology, formed in 2005. Over time, additional initiatives have been brought forward within the United States and globally by dermatology groups (eg, Global Alliance) and by pharmaceutical companies. Much more data are needed in this subject area, because many questions still remain. This article summarizes important principles gleaned from the continued efforts of the Scientific Panel on Antibiotic Use in Dermatology; other groups who are working diligently in this area, such as the CDC and the Canadian Antimicrobial Resistance Alliance; and from the published literature.
Major premise #1: dermatologists are the most common prescribers of antibiotic therapy in the United States
Principle #1: Antibiotic therapy is most commonly used by dermatologists to treat noninfectious inflammatory dermatoses, such as acne vulgaris (AV) and rosacea.
Principle #2: Durations of therapy with antibiotic use for many inflammatory dermatoses are often prolonged over several weeks to months.
Principle #3: Antibiotic resistance is a consistent and unavoidable adverse effect associated with systemic and topical antibiotic use. The emergence of serious infections caused by bacteria that are highly resistant to many previously effective antibiotics necessitates that all clinicians consider when an antibiotic truly needs to be used and to prescribe judiciously.
Topical and oral antibiotics are commonly used by dermatologists in clinical practice, primarily because of the overall track record of favorable efficacy and safety with the most commonly used agents (ie, tetracyclines, macrolides). Among categories of physicians in the United States including primary care and specialty areas, dermatologists prescribe more oral antibiotics per practitioner than any other physician group based on data collected by the US Centers for Disease Control and Prevention (CDC). The types of antibiotics that are commonly prescribed also differ among dermatologists compared with other physician types, with approximately three-fourths of all oral antibiotic prescriptions in the United States being written for a tetracycline agent (usually doxycycline or minocycline). The higher frequency of oral antibiotic prescribing and the differences in the types of antibiotics used by dermatologists compared with other physicians are because dermatologists commonly use tetracycline agents to treat common inflammatory skin diseases, especially AV and rosacea. Importantly, when oral antibiotics are used to treat AV and rosacea, they are frequently administered for prolonged durations of therapy over several weeks to months, compared with short courses used to treat common infections, such urinary tract infections, upper respiratory tract infections, otitis media, and uncomplicated skin/soft tissue infections. The use of oral antibiotic therapy to treat AV, especially the tetracycline agents doxycycline and minocycline, remains part of published guidelines on the management of AV, and is also included among recommended therapies for treatment of papulopustular rosacea. Because antibiotic resistance is an unavoidable sequelae of their systemic or topical administration, it is important that all clinicians take this into account when considering use of and selecting antibiotic therapy.
Over the past decade, increased attention has been given to the problems associated with antibiotic resistance, especially with the emergence of methicillin-resistant Staphylococcus aureus , macrolide-resistant staphylococci and streptococci, and hospital-based pathogens, such as enterococci and Clostridium difficile , which have acquired antibiotic resistance patterns that create major therapeutic challenges. In addition, the marked decrease over the past few decades in development of antibiotics, especially new drug classes, has been a major impetus for concern. The progressive increase in concerns and challenges related to antibiotic resistance has been felt globally, with many campaigns developed by several societies and government agencies to promote more prudent prescribing, reduce unnecessary antibiotic use, and increase surveillance and detection of emerging resistance patterns within hospitals and their surrounding communities. In the United States, major steps were put into motion approximately a decade ago by the CDC with initiatives to decrease antibiotic prescribing (especially for upper respiratory tract infections that are often caused by viruses) and by the Food and Drug Administration with changes in approved product labeling with most antibiotics that attempt to address optimal antibiotic use.
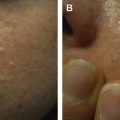
Despite all of the publicity in the medical literature and in the lay press (including the Internet) about antibiotic resistance concerns, the true “wake up call” in dermatology came with the emergence of skin infections caused by community-acquired methicillin-resistant S aureus . Once community-acquired methicillin-resistant S aureus surfaced in the United States, skin infections caused by methicillin-resistant S aureus were seen by dermatologists in their offices on a daily basis, or at least several times each week or month. Having these cases in front of them on a regular basis, and seeing first hand cutaneous infections cause by strains of S aureus that are resistant to commonly used antibiotics (penicillins, cephalosporins, macrolides, clindamycin) brought greater attention among dermatologists to the clinical relevance of antibiotic resistance beyond just the hospital environment. Nevertheless, many questions remain within the general dermatology community regarding how the use of topical and oral antibiotics by dermatologists contributes to the overall impact of antibiotic resistance and whether the resistance patterns that are created are truly relevant clinically.
The first dedicated group within dermatology in the United States to formally address the subject of antibiotic use and the potential implications of antibiotic resistance in dermatology is the Scientific Panel on Antibiotic Use in Dermatology, formed in 2005. Over time, additional initiatives have been brought forward within the United States and globally by dermatology groups (eg, Global Alliance) and by pharmaceutical companies. Much more data are needed in this subject area, because many questions still remain. This article summarizes important principles gleaned from the continued efforts of the Scientific Panel on Antibiotic Use in Dermatology; other groups who are working diligently in this area, such as the CDC and the Canadian Antimicrobial Resistance Alliance; and from the published literature.
Major premise #2: the importance of antibiotic resistance in dermatology extends far beyond Propionibacterium acnes
Principle #4: Administration of antibiotics systemically or topically causes “ecologic mischief” with collateral damage related to antibiotic resistance that is often underappreciated in the clinical setting. Antibiotic use induces the emergence of less sensitive bacterial strains among exposed commensal and transient flora, including pathogenic bacteria, through antibiotic selection pressure.
Principle #5: Systemically administered antibiotics expose bacteria present on skin and within mucosal tracts leading to the emergence of less sensitive bacterial strains and changes in the microbiome.
Principle #6: Topical antibiotics applied to facial skin induce the emergence of less sensitive bacterial strains present at the site of application, at remote skin sites where the antibiotic has not been applied, and with an increase in nasal staphylococcal carriage.
Principle #7: Resistant strains that emerge subsequent to use of an antibiotic can persist for several weeks to months after discontinuation of therapy.
In dermatology, the progressive increase in antibiotic-resistant Propionibacterium acnes has been well established, outwardly discussed for several years, and has been shown to reduce the efficacy of therapy for AV. However, it has been difficult for dermatologists to appreciate the clinical relevance of antibiotic-resistant P acnes because the use of combination regimens with other agents (eg, benzoyl peroxide [BP], topical retinoids) for AV results in improvement in most patients. Data showing that concomitant use of BP reduces the quantity and emergence of antibiotic-resistant P acnes strains at skin sites where BP is applied (ie, face) has created some comfort level with antibiotic use for AV. However, these data do not address antibiotic exposure at skin sites where BP is not applied, potential resistance patterns among bacteria other than P acnes , and resistance patterns within the oropharyngeal (OP), gastrointestinal (GI), and genitourinary/vaginal (GU-V) tracts.
Because they do not encounter the clinical sequelae of infections occurring at sites other than skin, many dermatologists have difficulty appreciating the “ecologic mischief” or “collateral damage” that oral and topical antibiotics can create by inducing resistance through antibiotic selection pressure. Selection pressure increases the emergence and quantity of bacteria that are less sensitive to the antibiotic among the normal commensal and transient flora on the skin, and within the bacterial population of the OP, GI, and GU-V tracts that are exposed to systemic (ie, oral) antibiotic therapy. Notably, topical antibiotic use on the face can induce antibiotic-resistant organisms (ie, staphylococci) on remote skin sites (eg, the back) and within the anterior nares. It is hard for many individuals to comprehend or accept that the antibiotic-resistant bacteria that develop when antibiotics are used to treat a disorder, such as AV, may be clinically relevant because they can potentially contribute to another type of infection in the individual or in others who the organisms may be spread to at a later time. At minimum, it has been established that use of oral and/or topical antibiotics for treatment of AV significantly increases OP streptococcal colonization and selects for a greater quantity of antibiotic-resistant strains. It has been shown that after discontinuation of an oral antibiotic, resistant strains that emerge can persists for weeks to months.
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree