The treatment of the obtuse, full neck is particularly challenging, and a defined jawline and cervicomental angle often requires manipulation of the deeper, subplatysmal neck structures. The causes of a full neck are multifactorial stemming from inadequate bone support, excess fat and skin and muscle laxity, and robust soft tissues. There are a wide variety of choices in rejuvenation of the jaw line, and this decision is based on anatomic knowledge, a thorough examination, sound surgical principles, as well as an understanding of the typical aging changes anticipated at various milestones.
Key points
- •
An obtuse neck can be challenging to rejuvenate in a facelift patient.
- •
Realistic expectations must be addressed prior to surgery.
- •
The causes if a challenging neck are multifactorial, inculding factors from the tissue layers of skin , muscle, fat and bone.
The lower face and neck exhibit some of the earliest and most telltale signs of aging with the start of jowls, loose neck skin, unwanted sub-mental fat deposits, and an obtuse profile. Five factors are critical in achieving an aesthetically pleasing neck including a defined lower mandibular border with no overhanging jowls, a subhyoid depression, visible thyroid cartilage, visible anterior border of the sternocleidomastoid muscle, and a cervicomental angle of approaching between 105 and 120° degrees [ ]. Many patients seek correction of undesirable aging changes of the lower face and neck, as witnessed by an increase face and neck lift procedures in recent years [ ] . The popularity of these procedures has been catapulted into the mainstream by both social media and the destigmatization of celebrities receiving elective surgery. This has created a unique challenge for surgeons as only the best and not the average results are shown on social media. The margin for error is small when performing an elective procedure such as a facelift and a full discussion of both the risks and benefits is critical. There are a myriad of factors that make some patients a challenging facelift candidate.
Meeting expectations is the most crucial aspect of performing any elective procedure. Understanding patient desires and pre-operatively discussing goals will enhance the chances of a successful outcome. Reviewing realistic outcomes are important prior to embarking with surgery. Many younger patients are heavily influenced by photographs that are altered by filters on social media, and these are often unobtainable results. Matching the correct procedure with the patient will ensure a more successful outcome. Also, some patients have body dysmorphic disorder and seek repetitive, unnecessary surgery in an attempt to reach an unattainable goal. These patients can be difficult, should be screened out, and counseled that surgery is not a good option.
The mantra of first do no harm should be foremost when assessing any patient for elective surgery. Pre-operative screening for non-compliant patients is important and any potential patient that does not take surgery seriously, understands and accepts the risks, or will not comply to a standard post-operative plan should be avoided. A patient should agree to take 3 to 4 weeks post operatively off with restrictions including no exercise, heavy exertion, sun exposure, or nicotine use. Facelift is an elective surgery that is for a healthy patient, and any potential candidate should receive clearance from their doctor if their medical history dictates. Anesthesia risks should be discussed with surgical candidates and those with poor airways or sleep apnea should be identified, and an anesthesia assessment performed prior to performing surgery to maximize safety.
Patients should discontinue all forms of nicotine use for 2 weeks prior and continue for 2 weeks after face and neck lift surgery. The author requires patients to sign a form that they will abstain from nicotine use, including vaping and smoking. This is done for patient safety and to improve healing and limit potential skin necrosis from nicotine-induced vascular compromise. Some authors feel a deep plane approach is safer in smokers as the flaps have a more robust, intact blood supple [ ]. Recently marijuana use has increased with legalization in some states, and although it does not appear to affect healing with moderate use; there are concerns of intraoperative reactive airway secretions and even possible increased nicotine levels [ ]. For this reason, marijuana use should be stopped prior to facelift surgery.
A thorough medical history is required to optimize a patient prior to surgery. All conditions that can impair healing should be considered and addressed. This includes blood sugar management in diabetic individuals to ensure an adequate healing response. If a delayed healing response is anticipated, then either deferring surgery or a more conservative approach with limited skin undermining is preferred. Any patient with potential for slow or delayed healing is encouraged to undergo post-operative hyperbaric oxygen treatments to enhance healing.
Cessation of blood thinners prior to surgery will also reduce the risk of a hematoma post operatively. Both antiplatelet and anticoagulant drugs should be stopped with guidance from a cardiologist if necessary. The recent inclusion of tranexamic acid, either intravenously or with local anesthesia, has proved beneficial in reducing bleeding, bruising and potentially decreasing the adverse event of a hematoma [ ].
Blood pressure control is paramount in the healing phase to avoid an unwanted hematoma, and intraoperative blood pressure management may be required to limit bleeding. Pre-operative oral clonidine may be beneficial to lower blood pressure. Patients that are overweight should be counseled on weight loss, and surgery should be delayed until a desirable and acceptable weight is reached. This is done not only to ensure a safer procedure under anesthesia, but also a better long-term result. Significant or massive weight loss after surgery can lead to excess loose skin that does not recoil with a smaller facial shape [ , ]. Recently, injectable weight loss drugs, which limit gastric emptying, such as semaglutide, have gained wide acceptance and patients should be counseled to stop them 3 weeks prior to surgery to limit the risks under anesthesia such as aspiration and pneumonia [ ].
Any patient that has undergone prior facial surgery, whether elective or reconstructive also poses an additional challenge to the facelift surgeon [ ]. Prior anatomy has been altered and blood supply has the potential to be compromised, leading to poor healing [ , ]. Particular challenges are present in post-parotidectomy patients as the facial nerve has been manipulated, increasing a potential risk of motor nerve injury [ ]. A thorough pre-operative examination incudes facial nerve function and any pre-existing palsies should be identified and identified prior to surgery. Obtaining prior surgical records is important in understanding what procedure was performed and if the tissue necessary to healing has been utilized or manipulated.
Patients who have undergone facial radiation for cancer can be poor candidates for facelift surgery as the blood supply necessary for healing has been compromised. The author prefers a deep plane approach in patients with radiation, as this avoids a thinner skin flap. The thicker deep plane flap incorporates a more substantial medial blood supply to enhance flap healing [ ].
Gender is a factor in respect to creating challenges for facelifts. Male patients in general are more challenging for several reasons [ ]. They have a larger body mass, require more drugs, and have larger heads necessitating more dissection. This requires more skin undermining, and the face and neck hairs of the beard have a significant blood supply. This causes more bleeding and a higher risk of hematoma. The author has experienced increased bleeding in male patients taking supplemental testosterone, and cessation of testosterone is recommendation 2 weeks prior to surgery. Popular male enhancement drugs, such as sildenafil, are arteriole dilators should be stopped 1 week prior to surgery to limit bleeding.
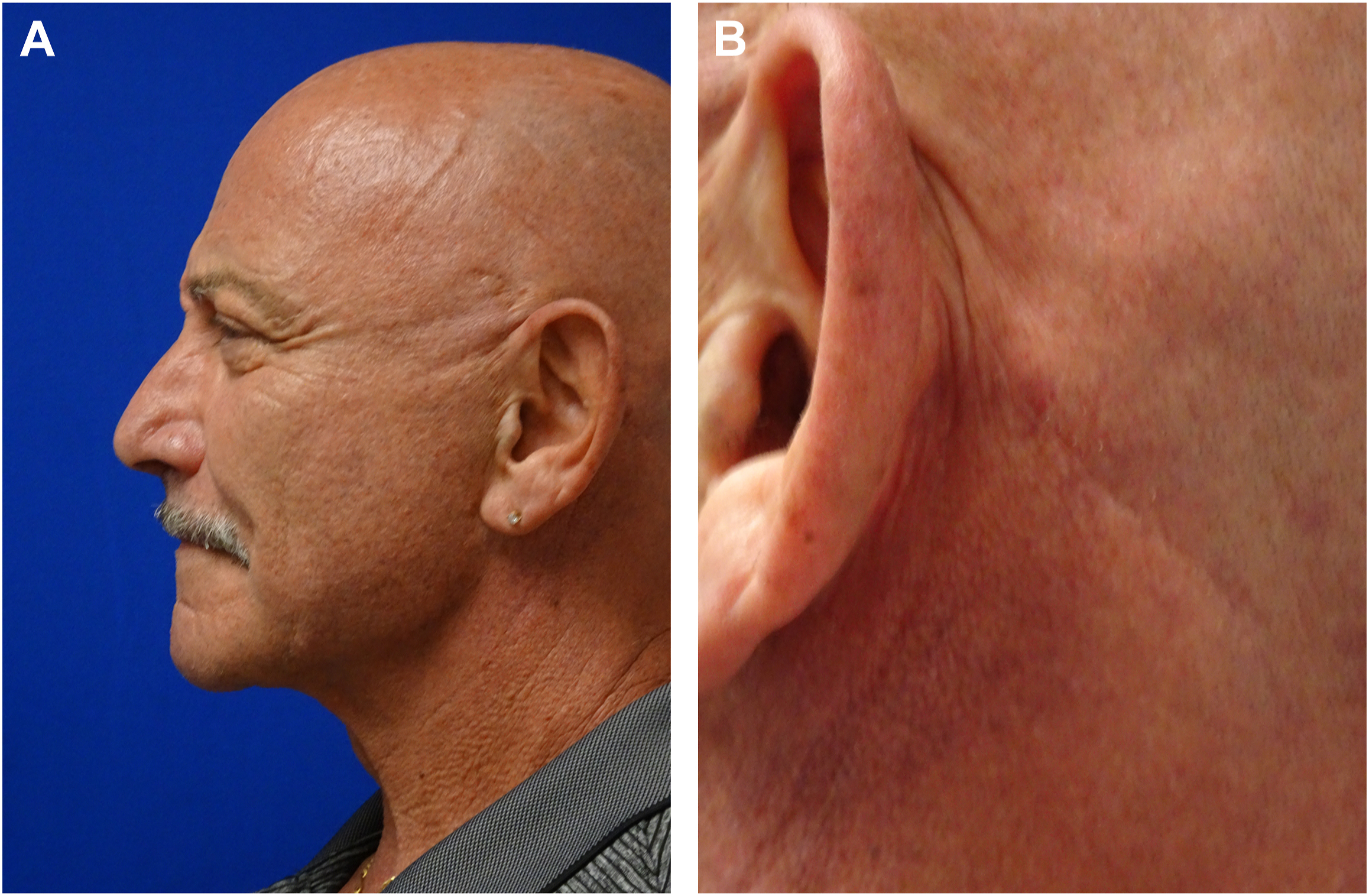
Many men have male pattern baldness, and some patients have alopecia and complete baldness, making scar camouflage more challenging [ ]. ( Fig. 1 ) A discussion about scar placement and scar visibility should be discussed with the patient in the surgical consult. Limiting skin tension on wounds, placing incisions in hidden creases around the ears and under the chin, as well as layered closure can be beneficial. Post-surgical scar modification may be necessary with laser skin resurfacing, 5-Flourouracil injections and silicone sheets, or gel. Keloid formers should be avoided, and hypertrophic scar formers should be identified pre-operatively and managed cautiously to achieve minimal scarring.
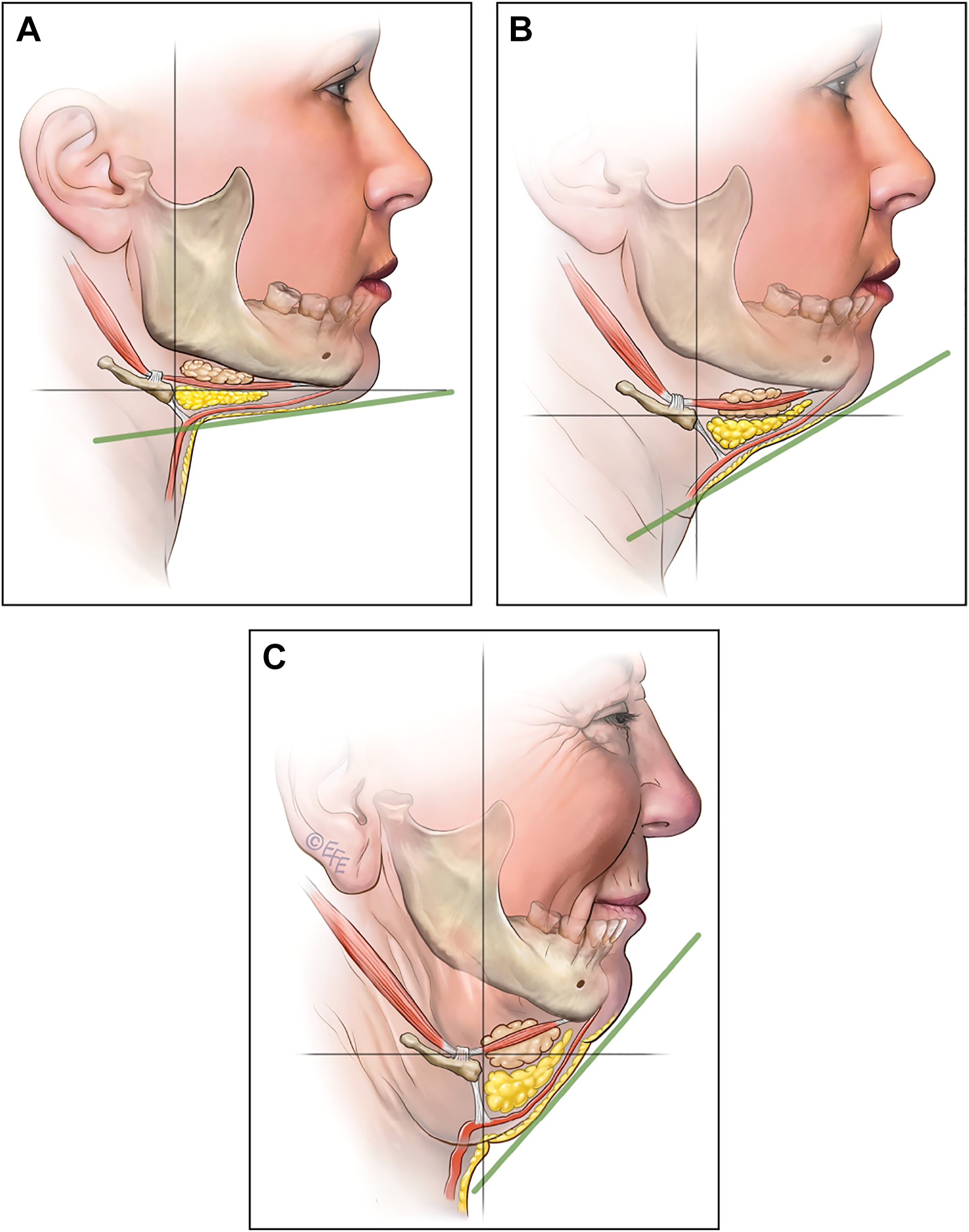
The treatment of the obtuse, full neck is particularly challenging, and a defined jawline and cervicomental angle often requires manipulation of the deeper, subplatysmal neck structures [ ]. The causes of a full neck are multifactorial stemming from inadequate bone support, excess fat and skin and muscle laxity, and robust soft tissues ( Figs. 2 and 3 ). Correction of the heavy neck must address all components contributing to the full neck, and intimate knowledge of anatomy and pathological aging changes of the face is crucial. An anatomically short, thick neck can be one cause of a full neck [ ]. Short necks can stem from underlying vertically short, horizontally wide cervical bones, along with more robust soft tissues ( Fig. 4 ). These patients are typically more endomorphic in their body habitus and are more difficult to correct surgically than thinner ectomorphic patients with long, lean necks. Patients with short, thick necks often have fuller faces, and buccal fat removal may be required to slim a round face.

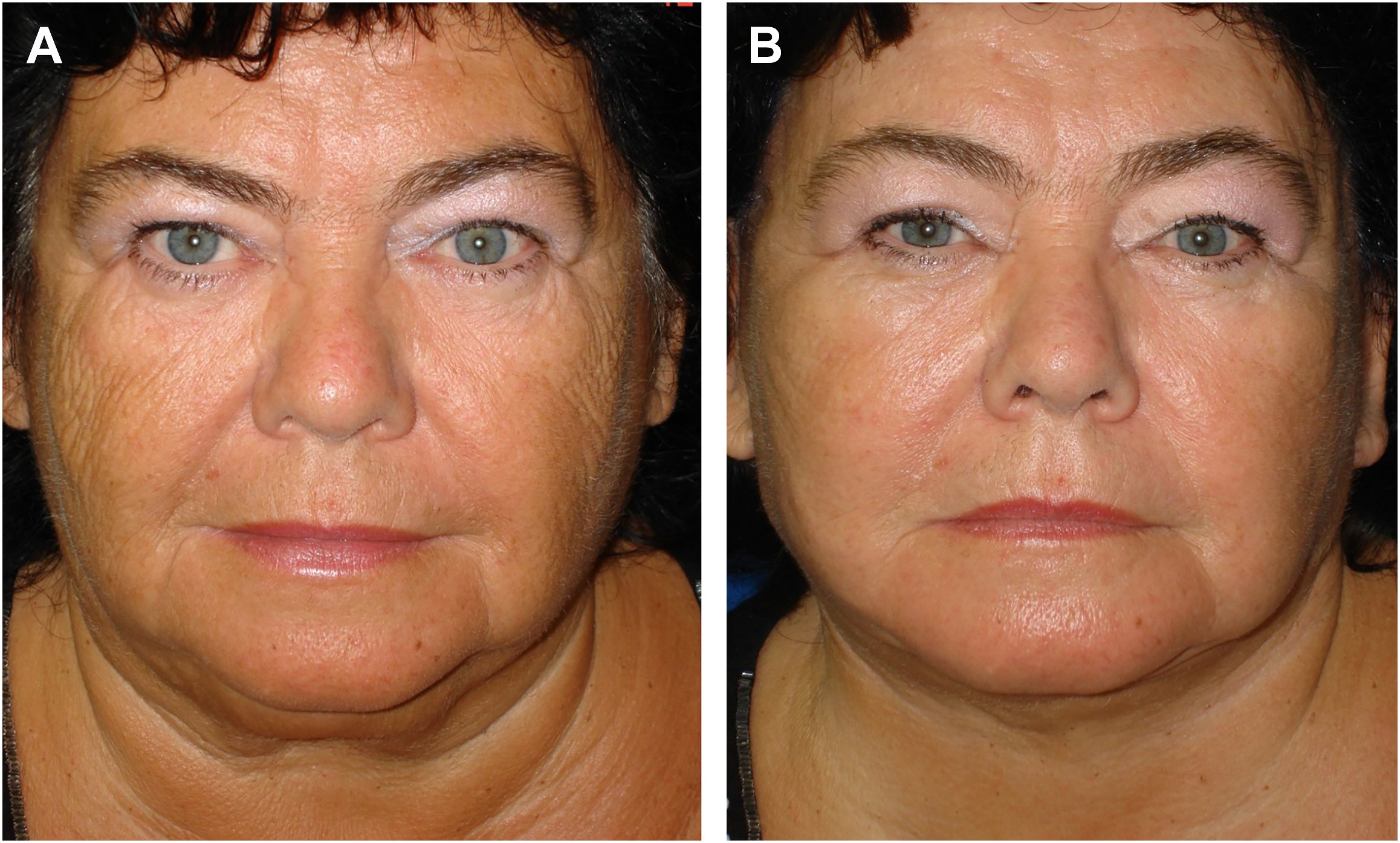
Clinical examination of the lower face should include assessment of the facial shape on a front view. Skin tone and laxity in addition to the amount and location of facial and neck fat are contributing factors to facial shape and should be noted. Visual inspection and manual palpation are required to document the presence of a sub-mental skin crease or scars, platysma bands, and facial nerve function ( Fig. 5 ).