CHAPTER 20 The Cementless Tapered Stem
Ream-and-Broach Technique
COMPONENT DESIGN
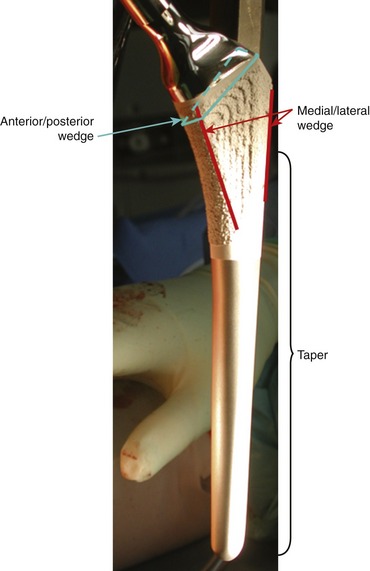
The stem described in this chapter includes a taper over the axisymmetrical portion of the stem and two proximal wedges, one medial/lateral and one anterior/posterior (Fig. 20-1). The end result is a proximally fitting, rotationally secure implant. These are straight stems that require machining of the bone for optimal fit and fill. The preparation is done in two steps. The tapered reaming machines the proximal femur and ensures an interference tapered fit in the intertrochanteric area and proximal diaphyses of the femur. Broaching is not cutting the bone but rather compressing an existing cancellous bone and creating a slightly undersized cavity for the double wedge. The end result is a very tightly fitted stem that transfers load proximally and minimizes proximal stress shielding.
TECHNIQUE
Tapered reaming is the first step; the surgeon should start with a reamer that is at least two sizes smaller than the templated size. The surgeon should feel the cortical contact with the final reamer, and he or she should inspect the final reamer to be certain that the contact is along the tapered part of the reamer proximally and not nearly distally. The presence of cancellous bone remains within the teeth of the reamer is helpful to confirm this (Figs. 20-2 and 20-3
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree