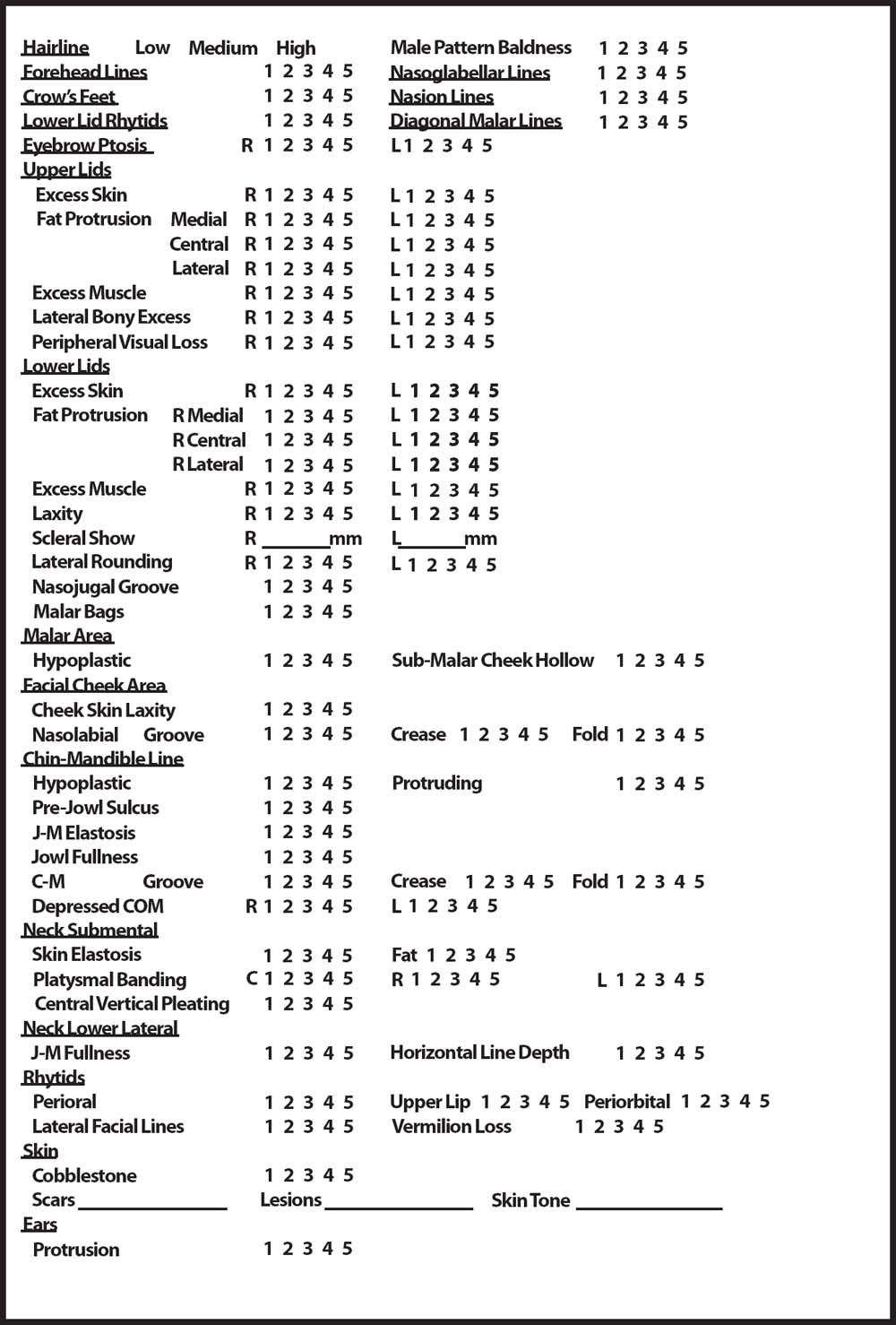
3 The importance of the aging neck and jawline cannot be overstated. Many patients seeking surgical rejuvenation of the head and neck report concerns with jowling and skin laxity as their chief concerns. Patients desire a sharp cervicomental angle (CMA) from their youth onward, and in some cases want a defined jawline that they never had. To achieve an optimal patient result, both in terms of surgical outcome and patient satisfaction, it is essential to understand the aging process of the neck, properly analyze the problems affecting each patient’s neck, understand the patient’s goals and expectations, and select the proper surgical technique with which to correct the patient’s pathology. Some authors have described visual criteria for the youthful neck1 that include a: 1. Distinct inferior mandibular border from the mentum to the angle of the mandible without jowl overhang 2. Subhyoid depression 3. Visible bulge of the thyroid cartilage 4. Visible and distinct anterior border of the sternocleidomastoid (SCM) muscle throughout its entire course from the mastoid to the sternum 5. Cervicomental angle (CMA) of 105 to 120 degrees Another classification system for deformities of the neck is that proposed by Dedo,2 as described in Chapter 2. The classes in this system are: Class I: Minimal deformity, with a well-defined CMA, good platysma-muscle tone, and no accumulation of fat Class II: Early elastosis of the cervical skin, no accumulation of fat, and no weakness of the platysma muscle Class III: Early elastosis of the cervical skin, accumulation of fat, and no weakness of the platysma muscle Class IV: Accentuation of the platysma muscle, with banding present either in repose or on muscle contraction Class V: Congenital or acquired retrognathia/microgenia Class VI: A low position of the hyoid bone Although classification systems serve as useful tools for comparing patients and providing goals for rejuvenation, it must be stressed that the analysis and treatment of deformities of the neck should follow an approach to each patient that is individualized according to the patient’s personal pathology. The aging process depends upon genetic, anatomical, and environmental factors. The most commonly held theory of facial aging is one of progressive gravimetric soft-tissue descent.3 With repeated gravitational forces, skin and soft tissue stretch off the bony skeleton, leading to the development of folds, rhytids, and loss of volume. However, facial aging is much more complex than this, and a proper discussion of it involves dividing the components of facial anatomy into basic categories, including skin, subcutaneous tissue, fascia/muscle, and bone. The skin is subject to both extrinsic and intrinsic aging processes. Within the skin, aging is marked by thinning of the epidermis and by a disorganization of collagen fibers and reduction in their numbers in the papillary and reticular dermis, including a loss of type I collagen and increased presence of type III collagen fibers. There is also effacement of rete ridges within the epidermal–papillary dermal junction. Further contributing to the appearance of aging is the development of dyschromias from collective solar damage to the skin. The resulting solar elastosis and disorganization lead to thinning of the skin and the development of static rhytids. Cumulative exposure to ultraviolet (UV) A and B light leads to direct damage to deoxyribonucleic acid (DNA) in cells of the skin, as well as to the formation of free radicals which, with the decreased levels of antioxidants that accompany advancing age, are less easily buffered. Furthermore, dehydration of the skin and reduction in the sebaceousgland production of sebum leads to further thinning of the skin and the formation of rhytids. Accompanying the changes in the skin that occur with aging are changes in deeper structures. With advancing age there is a concomitant decrease in the basal metabolic rate, leading to increased formation of adipose tissue. Proportionate increases in fat are seen in the face beginning in the fifth decade.3 Fatty tissue accumulates in depot areas of the body beneath the superficial fascia. In the face and neck these areas are located in the periorbital, malar, and submental regions. Progressive fascial and ligamentous laxity decreases the support of adipose tissue, resulting in a relative increase in volume of the lower third of the face. In these patients it is important to address the growth in volume of the lower face and neck, but to also remain cognizant that adipose tissue may camouflage the aging of other tissues, such as platysmal banding or ptosis of the submandibular glands. In many women, the decrease in estrogen levels that occurs with the onset of menopause is accompanied by a further decrease in the volume of deposits of superficial fat, resulting in thin, poorly supported skin that is easily pulled gravimetrically by deeper fat. There can also be a loss of subcutaneous adipose tissue, resulting in volume depletion and hollowing. Additionally, there is increased elasticity of the superficial musculoaponeurotic system (SMAS), which serves as a supporting framework for the skin, leading to vertical descent of the skin–soft-tissue envelope of the face and neck. Besides this, the platysma muscle loses much of its tone with aging, and repeated contraction of the muscle, combined with volume loss in the anterior neck, can lead to prominent vertical banding of the platysma. The aging process also affects the skeletal foundation of the face. Hormonal changes lead to an overall decrease in bone density. This decrease is not exclusive to weight-bearing bone, but may also be seen in the facial skeleton. Osteopenia of the zygoma and maxilla leads to a decrease in malar prominence and a loss of support for the malar fat pads, SMAS, and facial musculature. Osteopenia of the mandible contributes to formation of the anterior mandibular groove and may accentuate existing microgenia or result only in a hypoplastic mentum. Individual patient factors also play an important role in aging. Perhaps the most important of these factors is tobacco use, which is still quite prevalent and is extremely detrimental to skin quality and blood supply. Model4 originally coined the term “smoker’s face” and attributed it to the following visual criteria: 1. Lines or wrinkles on the face, typically radiating at right angles from the upper and lower lips or corners of the eyes; deep lines in the cheeks; or numerous shallow lines in the cheeks and lower jaw. 2. A subtle gauntness of the facial features, with prominence of the underlying bony contours. When fully developed, this change gives the face an “atherosclerotic” look; lesser changes show as a slight sinking of the cheeks. In some cases these changes are associated with a leathery, worn, or rugged appearance of the face. 3. An atrophic, slightly pigmented and gray appearance of the skin. 4. A plethoric, slightly orange, purple, and red complexion that differs from the purplish-blue color of cyanosis or the bloated appearance associated with the pseudo-Cushings’s changes of alcoholism. These qualitative visual criteria reflect physiological changes occurring beneath the epidermis, at the dermal level. The nicotine in tobacco products increases blood levels of vasopressin, causing peripheral vasoconstriction and a state of dermal ischemia.5–7 As blood levels of nicotine decline, leading to a decrease in vasoconstriction, postischemic reperfusion may lead to the generation of reactive oxygen species, which are a major component of UV injury and photoaging.8 Induction of matrix metalloproteinases within the skin9 may be yet another mechanism by which tobacco smoke leads to premature aging of the skin. Other important factors that contribute to the aging of the skin include skin type, a history of exposure to the sun, a history of skin irradiation, hyper- or hypothyroidism, diabetes, peripheral vascular disease, atherosclerosis, and liver failure. Not only do these factors contribute to aging of the skin, but they may also influence the degree of surgical correction of the aging face and neck by affecting the viability of skin flaps. Ameliorating factors, such as the use of retinoic acid, routine skin care, and protection from the sun, may retard the aging process. Historically, there has been an evolution of techniques for correcting the aging neck. Early techniques for facial rejuvenation appear to have originated in Europe and involved simple skin excisions through incisions made in natural pre- and postauricular creases.10 The first formal teaching on rhytidectomy, involving extensive undermining of sub-cutaneous tissue and lipectomy, came in 1919 from Bourguet11 and Bettman.12 After the First World War, the development of cervicofacial rejuvenation occurred largely in North America. However, all of the flaps used in this were subcutaneous, and rejuvenation was accomplished through the resection of skin. This began to change with the next major innovation in cervicofacial rejuvenation, with the development in 1968, by Tord Skoog, of a subplatysmal flap without detachment of the overlying skin.13 This flap also incorporated the superficial fascia of the lower third of the face, which Skoog termed “buccal fascia.” The platysma and fascia were undermined anteriorly to the nasolabial and commissural–mandibular grooves, and the flap was repositioned posteriorly and affixed to the parotidomasseteric and mastoid fasciae. In 1976, Mitz and Peyronie discovered a fascial layer that invested the mimetic facial musculature and was distinct from the underlying parotidomasseteric fascia. It was this fascia that was named the superficial musculoaponeurotic system (SMAS) and which is the basis for rhytidectomy involving the SMAS. At the end of the twentieth and beginning of the twenty-first centuries, various techniques were developed for limited rhytidoplasty. Their development has been partly based on the desire of the patient population for a more rapid recovery from surgery for cervicofacial rejuvenation. Many different names have been given to the flaps used in these procedures, but all of them involve a preauricular incision with some degree of postauricular incision. There is sub-cutaneous undermining of the skin flap and plication or imbrication of the SMAS and platysma muscle. Critics of these lifts question the longevity and degree of improvement achieved with limited undermining and resuspension of the SMAS and platysma. However, more aggressive techniques of rhytidoplasty have also been developed. Increasing degrees of undermining of subcutaneous tissue, coupled with sub-SMAS dissection anterior to the parotid gland, were purported to effect greater improvement and greater longevity in the correction of ptotic tissue. Nevertheless, these techniques were criticized for producing only limited improvement in the nasolabial fold and the ptotic midface. Hamra, in 1990, described his deep-plane rhytidectomy to better address redundant nasolabial folds.14 This procedure involves a limited subcutaneous dissection in front of the tragus and to the jawline, followed by a sub-SMAS dissection in the lower face, referred to as the Skoog technique, to the malar eminence and mandibular border. Submuscular dissection proceeds to expose the orbicularis and zygomaticus muscles in the region of the nasolabial fold, where this dissection joins the sub-SMAS Skoog dissection. A thick musculocutaneous flap is created, containing skin, platysma, and fat pads of the cheek. The Skoog flap is then advanced and suspended from the preauricular parotidomasseteric fascia, and the upper facelift flap is rotated and advanced with the dermis of the flap, which is secured to the superficial temporal fascia at the level of the helix of the ear. The platysma is addressed through the approach used for a submentoplasty, with imbrication of the platysma and horizontal sectioning of the platysma with electrocautery. The posterior border of the platysma is left attached in its original position. Hamra then presented the composite rhytidectomy,15 in which the deep-plane approach was extended further to include repositioning of the ptotic orbicularis oculi muscle. In this procedure the platysma is addressed in a manner similar to that in the deep-plane rhytidectomy, in that vertical resection with imbrication is performed. However, there is no horizontal resection and no specific posterior resuspension of the platysma. Much debate has surrounded the merit of such extended procedures with regard to intraoperative risk, postoperative recovery, and long-term benefit in terms of improved rejuvenation and longevity of repair. A long history also marks the development of techniques for addressing the submental region. Bourguet11 discussed submental lipectomy and the transection of platysmal bands. Subsequently, many techniques have been used to address the aging platysma, such as varieties of midline plication/imbrication, horizontal wedge resection, corset platysmaplasty,16 interlocking suspension with cervico-mental sutures,17 and the use of expanded cervical slings with polytetrafluoroethylene (ePTFE) sutures.18 Techniques used to address submental adipose tissue initially involved lipectomy, with cervicofacial liposuction a subsequent innovation. The treatment of skin redundancy has involved various approaches, such as allowing postoperative readhesion and redraping, vertical elliptical excision of skin with simple versus Z-plasty, W-plasty, and double-advancement flap closure. As is evident from the preceding discussion, there is a rich heritage of surgical approaches to rejuvenation of the aging neck, with many different techniques currently being used for this. As is often the case in medicine when multiple techniques are used to address a particular issue, there is frequently no single optimal approach, with each approach having advantages and disadvantages. What must be emphasized is that selection of the optimal surgical technique for a particular patient depends on the patient’s individual pathology and should be tempered by the surgeon’s level of experience and comfort. The consultation process begins as soon as the patient’s initial telephone call is made to the surgeon’s office. A receptionist who is both pleasant and well-versed in the basics of the procedures of the practice is fundamental for success. Often the decision to book a consultation depends on the patient’s telephone demeanor and information that the patient provides over the telephone. However, there is a fine balance between offering useful information and providing a free consultation. After answering fundamental questions, the surgeon should make every effort to schedule an appointment for a consultation. The next phase of the consultation occurs when the patient enters the surgeon’s practice office. The waiting room should be welcoming, tastefully decorated, and spacious enough to offer a feeling of privacy. A courteous patient-care coordinator or receptionist should greet the patient and give a brief orientation to the practice. Necessary information, including e-mail contact information for future practice updates, a pertinent medical history, and the reasons for requesting a consultation should then be provided in writing by the patient. Any forms to be filled out by the patient should be succinct, to avoid giving the patient a feeling of impersonality. As soon as the forms are completed, the patient should be escorted to a comfortable consultation room where books of pre- and postoperative photographs of patients who have had reconstructive cervicofacial surgery are available for leisurely perusal while the patient waits. Although it depends on the style of the practice, a trained consultant is usually the next person after the receptionist to see the patient. This consultant should be professional in appearance and manner, friendly, and able to ease any reservations the patient may have about the surgeon or the practice. The consultant should review the patient’s medical history, including any previous cosmetic or rejuvenation procedures, discuss the reason for the consultation, and provide a brief background description of the surgeon and of the basic treatment involved in cosmetic surgery before the surgeon meets the patient. Preoperative photographs of the patient may be taken at this time and should include anteroposterior, right and left oblique, and right and left lateral views. This preconsultation should last approximately 10 to 15 minutes and should make the patient feel completely at ease with the surgeon’s practice. It should set the tone and lay the groundwork for the consultation with the surgeon. Discussion with the consultant before the surgeon meets the patient is extremely important to ensuring an optimal first surgeon–patient interaction. Some patients are open at this time to a global assessment of their pathology and treatment options, whereas others want only to discuss limited areas of concern. Upon entering the consultation room, the surgeon should quickly establish a friendly rapport with the patient. Any concerns about the patient’s medical history, including any tobacco use or potentially harmful medications or herbal supplements, should be succinctly addressed. Past cosmetic or rejuvenation treatments need to be discussed, and any resultant imperfections pointed out and documented. It is useful to then address the patient’s concerns, thereby validating them, and to offer a brief discussion of the patho-physiology of the patient’s problem in easily understood terms. If the patient is amenable to a global assessment, it is extremely valuable to do this in a systematic, consistent manner. The authors use a standardized evaluation form for every patient consultation (Fig. 3.1). A numerical scale allows quantification of the findings in the patient’s case, as well as allowing comparisons among patients, and is essential in the planning and selection of a reconstructive technique for each patient. After completing the evaluation form, the surgeon should explain the assessment to the patient and the patient should be given an opportunity to ask questions. Treatment options for the patient should then be discussed. It is practical to broadly categorize these into noninvasive and invasive options. Noninvasive treatments include the use of botulinum toxin, injections of filler materials, and resurfacing to address dyschromias and static rhytids. Invasive treatments include a variety of surgical options that will be discussed in depth later in this chapter. The surgeon should then give the patient an additional opportunity to ask questions directly or through a patient-care coordinator. All fee schedules should be clearly explained so as to avoid any future confusion. A copy of any fee sheets should be given to the patient, with encouragement to call or return for reconsultation if questions arise. It is the practice of the senior author (H.M.) to charge a nominal consultation fee, which may be used as a deposit for any future surgery. This may serve to legitimize the consultation process, help defray staff and material costs, and help discourage “doctor shopping.” Although patients who will undergo rejuvenation of the neck routinely have a complete facial analysis, this discussion will focus only on findings pertinent to the aging neck. It is important to view the neck as part of the patient’s global appearance. Addressing the neck at the expense of facial pathology can lead to postoperative imbalance, an unnatural look, and patient dissatisfaction. Visual inspection begins with an assessment of skin quality of the neck, which includes dyschromias, static horizontal furrows, and skin lesions such as nevi, skin tags, or acrochordons. Palpation also plays a fundamental role in assessing pathology of the neck. Elastosis of skin may be estimated visually, but palpation helps confirm the extent of tissue laxity and position of the submandibular glands. Following a superior-to-inferior direction, evaluation of pathology of the neck begins with assessment of the chin–mandibular line. On lateral view, the pogonion is the most anterior projection of the chin. The ideal location of the pogonion is tangential to a line perpendicular to the Frankfort horizontal from the vermilion border of the lower lip.19 If a patient is in normal class I occlusion (mesiobuccal cusp of the maxillary first molar interdigitating with the buccal groove of the mandibular first molar), and the pogonion is posterior to this line, the mandible is hypoplastic. Although the ideal position of the pogonion in men is tangential to the line just described, its ideal position in women may lie 1 to 2 mm posterior to this. In addition, the mentolabial sulcus should lie ~4 mm posterior to a vertical line from the vermilion border of the lower lip to the pogonion.20 A hypoplastic mentum may be the result of microgenia, in which the chin is of small size as a consequence of underdevelopment of the mandibular symphysis, or from micrognathia, which is the result of hypoplasia of various parts of the jaw.21 Alloplastic implantation is indicated for a hypoplastic mentum in patients with normal or near-normal occlusion. Fig. 3.1 The standardized form used by the senior author for patient facial analysis. Although the development of a hypoplastic mentum is largely determined by genetic factors, the development of a groove between the chin and the remainder of the body of the mandible, known as a prejowl sulcus, is more the result of aging. Although this sulcus, or antegonial notch, may be congenital and be present from childhood,22 a combination of progressive soft-tissue atrophy and gradual bony resorption of the inferior mandibular edge immediately anterior to the jowls (anterior mandibular groove)23,24 also results in the development of a prejowl sulcus.25 With continued aging, the prejowl sulcus may merge with the commissural–mandibular groove, or “marionette line,” further accentuating a classic sign of the aging jawline. A prejowl sulcus may be repaired through alloplastic implantation with the Mittelman PreJowl Implant, or by the submuscular placement of filler substances, such as hyaluronic acid or hydroxylapatite. Immediately inferior to the mandibular border, and lying just anterior to the angle of the mandible, are the submandibular or submaxillary glands. With advancing age, ptosis of these glands is common, and failure to recognize this pathology may compromise the aesthetic cervicomandibular contour. It is important to point out prominent and ptotic submandibular glands to the patient during the preoperative consultation. Although the authors of this chapter does not routinely address ptotic glands, a variety of treatment options exist for this problem. De Pina and Quinta advocate gland resection at the time of rhytidectomy, through either the rhytidectomy incison or a cervical incision.26 Singer and Sullivan advocate gland excision through a submental incision,27 and others recommend submental–mastoid suture suspension or imbrication/plication of the periglandular platysma for the correction of ptotic submandibular glands.28 The degree of a patient’s jowl–mandibular elastosis is estimated by palpating tissue laxity along the mandibular margin, simulating the direction of pull in a rhytidoplasty. Jowl fullness is assessed primarily through visualization of the jowl immediately posterior to the anterior mandibular ligament, and is the result not only of soft-tissue descent but also of accumulation of adipose tissue. Palpation may be used to confirm the presence of adipose tissue. The commissural–mandibular area is next assessed. This area is commonly referred to as containing the “marionette lines,” but use of the proper nomenclature for these is warranted. The commissural–mandibular fold (CMF) refers to the extent of tissue lateral to each marionette line. The CMF is a measure of soft-tissue excess and descent. The commissural–mandibular crease refers to the true depth of etched rhytid formation within the marionette “groove.” In general, this crease tends to increase in severity with advancing age. The commissural–mandibular groove (CMG) refers to the concavity between the CMF and the lower lip. The distinction in terms is important when discussing the use of fillers and the location of injection of filler material. One would never inject material directly into the fold because this would accentuate the depth of the groove. However, it is quite appropriate to inject material into the commissural–mandibular crease to reduce its depth or into the CMG to create a smooth contour and decrease or eliminate the CMG. The corner of the mouth, or oral commissure, is next evaluated. With advancing age and loss of soft-tissue support, the commissure commonly becomes downturned, creating an “unhappy” appearance of the face. Not only should the degree of this depression be noted, but the creases on each side of the face should be compared with one another to document pretreatment asymmetry and to help guide treatment. Evaluation of the submental area has several components. Elastosis of the skin is evaluated in a manner similar to that for the jowl–mandibular region, using both visual inspection and manual palpation. Medial–lateral as well as superior–inferior movement should be assessed. The amount of adipose tissue, both subcutaneous and subplatysmal, should be estimated by visualization as well as palpation. Accumulation of fat is not universal with age, and skeletonization of subcutaneous muscles should be avoided to preserve a natural appearance. Platysmal banding should be assessed with the patient in repose as well as with animation. A distinction must be made between lateral banding and central banding (Fig. 3.2), because this may dictate treatment. By asking the patient to curl the lower lip or grimace, the anterior edge of the platysma may be brought into relief. Central vertical pleating of skin is often found between lateral platysmal bands, and represents a medial–lateral excess of skin. Fig. 3.2 (A) A right oblique view of a neck with lateral platysmal banding. (B) A right oblique view of a neck with central platysmal banding. All of the findings described above should be clearly documented on the assessment form. Special description of any unusual pathology should be made. All findings should be demonstrated and explained to the patient so that surgical recommendations may be better understood and realistic postoperative expectations better achieved.
The Aging Neck: Patient Consultation, Physical Findings, and Selection of Rejuvenation Technique
Pathophysiology of the Aging Neck
Aging of the Skin
Aging of Soft Tissue
Aging of the Facial Skeleton
Other Factors in Aging of the Neck
Historical Background
Patient Consultation
Physical Findings
Jowl/Mandibular Evaluation
Evaluation of the Submental Area and Neck

Selection of Technique
Nonsurgical Interventions
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree








