Temporoparietal (Superficial Temporal Artery) Fascial Flap
H. S. BYRD
EDITORIAL COMMENT
Detailed studies of the temporoparietal area have resulted in some controversy over the number of layers. For clinical purposes, the author’s description and guidelines are accurate and clinically safe.
The superficial temporal artery fascial flap is derived by dissecting the scalp away from its underlying subcutaneous fascia and the contained axial (superficial temporal) vessels, thereby creating a vascularized fascia that can be transferred about a single vascular pedicle.
INDICATIONS
This flap is useful in reconstructing defects of the forehead, eyebrow, eyelid, and ear (1, 2, 3, 4) (see also Chapter 96). It also has been used to provide a vascular cover for bone grafts where an adequate soft-tissue bed does not exist.
ANATOMY
The temporoparietalis is a thin sheet arising from the temporal fascia above and anterior to the ear. It is divided into three parts that spread out like a fan over the temporal fascia. There is a temporal part anteriorly, a parietal part superiorly, and a triangular part between. The temporoparietalis inserts into the lateral border of the galea aponeurotica. The auricularis anterior and superior are recognized as small but inconstant muscle bellies that contribute to this layer.1
The key to the anatomy of the temporoparietal fascial flap is an understanding of the relationship of the superficial temporal vessels to the layers of the scalp (Fig. 6.1). The specific fascia carried by the superficial temporal vessels is the temporoparietalis fascia with its upper galeal aponeurotic extension. The temporoparietalis fascia must be distinguished from the denser and anatomically deeper temporalis fascia, which invests the temporalis muscle. Confusion arises at the level of zygoma, where both the temporalis and temporoparietalis fasciae attach.
At the level of the ear, the vessels are found deep to the subdermal fat and on the surface of the temporoparietalis fascia. At a level approximately 10 cm above the crus helix, the vessels take a more superficial course, penetrating the subdermal fat and eventually entering the subdermal plexus. While there is some variance in the level at which the axial vessels become contiguous with the subdermal plexus, generally this occurs 12 cm above the crus helix. At this level, a subdermal dissection violates the blood supply and thereby describes the limit of the fascial vascular domain.
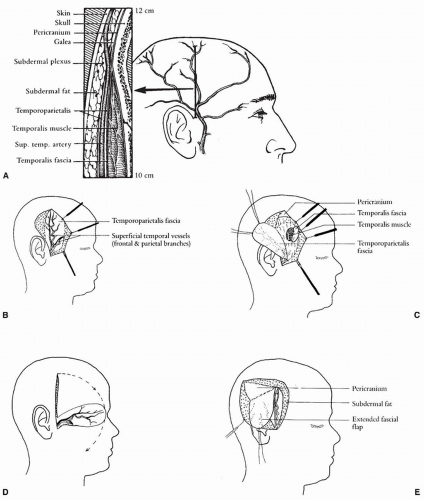 FIGURE 6.1 A: Relationship of temporoparietal fascial flap to the layers of the scalp. Cross section of temporal scalp in the area between 10 and 12 cm above the crus helix. At the 10-cm point, the vessels are still on the surface of the temporoparietal fascia, but by the 12-cm point, the vessels have entered the more superficial subdermal plexus. B: Frontal and parietal branches of the superficial temporal artery and vein lying on the temporoparietal fascia. C: Layers of tissue in the temporal region. D: Arc of anterior rotation of the temporoparietal fascial flap. E: Posterior extension of the flap.
Stay updated, free articles. Join our Telegram channel
Full access? Get Clinical Tree
 Get Clinical Tree app for offline access
Get Clinical Tree app for offline access

|