Temporalis muscle tendon unit (MTU) transfer may be used as a single-stage procedure for dynamic reanimation of the paralyzed face. Principles and biomechanics of muscle function and tendon transposition are essential in optimizing outcome. Critical steps and pearls for success include minimizing scarring, maintaining glide plains, mobilizing adequate tendon length, insertion of MTU at ideal tension based on intraoperative dynamic tension-excursion relationship, and insertion of tendon as close to the lip margin as possible. Because muscles adapt to tension, load, and task changes by altering their sarcomere arrangement and muscle fiber composition, physiotherapy should be initiated to use the repurposed temporalis MTU for smile restoration.
Key points
- •
The temporalis MTU procedure is an effective single-stage procedure for reanimating the paralyzed face and restoring smile.
- •
As with all functional muscle transfer procedures, surgeons performing the temporalis MTU procedure should be guided by the biomechanics of muscle function and the principles of tendon unit transfer muscle.
- •
Intraoperative electrical stimulation guides the establishment of the tension excursion relationship of the transposed tendon to guide optimal insertion to avoid overcorrection.
Introduction
Facial paralysis can be a devastating injury that results in functional impairment of the eyelids, nose, and lips. Impaired facial expression during communication and the associated blunted emotional exchange significantly affects the patient and their interactive circle and can lead to depression and strained relationships. Restoring facial tone, movement, and expression are primary goals of facial reanimation surgery and are achieved in almost all cases when the appropriate intervention is selected in a timely fashion. The functional end organ that produces dynamic movement consists of two discrete parts, the muscle belly and its tendinous attachment. An intact muscle tendon unit (MTU) with a given function may be repurposed to perform a new function by releasing and reattaching the tendon from its native insertion site to a new target. Functional MTU transfer is a common procedure performed in the upper extremity to restore hand function. The temporalis tendon transfer procedure and digastric tendon transfer are examples of functional MTU transfer procedures used in the correction of facial paralysis. In 1952, McLaughlin first introduced the concept and technique of mobilization and transposing the temporalis tendon for facial suspension. In the past two decades, the temporalis MTU transfer procedure has regained popularity as a single-stage option for reanimating the paralyzed face. Although newer and refined techniques of free functional microvascular transfer of muscles, such as the gracilis, latissimus, pectoralis minor, and sternohyoid muscles flap, have added new dimensions to facial reanimation, tendon transfer remains a viable option in the management of facial paralysis. The temporalis MTU originates from the temporal fossa as a broad fan-shaped muscle that converges into a tight tendon inserting on the coronoid process of the mandible. Detaching the temporalis muscle tendon from the coronoid process and inserting it into the upper lip can repurpose the temporalis muscle function for commissure contraction and smile restoration after facial paralysis. Understanding the functional anatomy of the temporalis muscle as an MTU and appropriately selecting patients for this procedure is a prerequisite for its successful application in facial reanimation. In addition, the principles and biomechanics of MTU function should guide the surgeon when applying the temporalis MTU for smile restoration.
Introduction
Facial paralysis can be a devastating injury that results in functional impairment of the eyelids, nose, and lips. Impaired facial expression during communication and the associated blunted emotional exchange significantly affects the patient and their interactive circle and can lead to depression and strained relationships. Restoring facial tone, movement, and expression are primary goals of facial reanimation surgery and are achieved in almost all cases when the appropriate intervention is selected in a timely fashion. The functional end organ that produces dynamic movement consists of two discrete parts, the muscle belly and its tendinous attachment. An intact muscle tendon unit (MTU) with a given function may be repurposed to perform a new function by releasing and reattaching the tendon from its native insertion site to a new target. Functional MTU transfer is a common procedure performed in the upper extremity to restore hand function. The temporalis tendon transfer procedure and digastric tendon transfer are examples of functional MTU transfer procedures used in the correction of facial paralysis. In 1952, McLaughlin first introduced the concept and technique of mobilization and transposing the temporalis tendon for facial suspension. In the past two decades, the temporalis MTU transfer procedure has regained popularity as a single-stage option for reanimating the paralyzed face. Although newer and refined techniques of free functional microvascular transfer of muscles, such as the gracilis, latissimus, pectoralis minor, and sternohyoid muscles flap, have added new dimensions to facial reanimation, tendon transfer remains a viable option in the management of facial paralysis. The temporalis MTU originates from the temporal fossa as a broad fan-shaped muscle that converges into a tight tendon inserting on the coronoid process of the mandible. Detaching the temporalis muscle tendon from the coronoid process and inserting it into the upper lip can repurpose the temporalis muscle function for commissure contraction and smile restoration after facial paralysis. Understanding the functional anatomy of the temporalis muscle as an MTU and appropriately selecting patients for this procedure is a prerequisite for its successful application in facial reanimation. In addition, the principles and biomechanics of MTU function should guide the surgeon when applying the temporalis MTU for smile restoration.
Indications for temporalis tendon transfer
In 1974, Burkhalter reported the indications for MTU in extremity injury, which are applicable to the temporalis tendon transfer: (1) the transfer can act as a substitute during regrowth of a nerve, which thereby reduces the time of function loss; (2) the transfer can act as a helper and add power to normal reinnervated muscle function; and (3) the transfer can act as a substitute when, statistically, the recovery after neurorrhaphy or nerve repair is poor. When presented with facial paralysis, the clinician should make the determination if the paralysis is reversible. Reversible paralysis is that which may recover spontaneously or after nerve repair or grafting. Timely nerve grafting or nerve substitution to reinnervate a reversibly paralyzed facial muscle yields superior results to muscle tendon procedures. Electromyogram studies in combination with clinical history can help establish the reversibility of the paralyzed facial muscle. In cases were the repaired nerve is expected to recover partially or slowly, the temporalis MTU procedure can be performed as an adjunct while waiting for regrowth of the nerve thereby reducing the time of facial dysfunction. A typical example is a patient who after a radical parotidectomy is scheduled to undergo postoperative radiotherapy. Although the facial nerve is grafted, a temporalis MTU can be performed at the same time to provide facial support. The temporalis MTU transfer procedure can also be considered as an option to upgrade partial recovery after facial paralysis. The indications for the temporalis MTU procedure overlap with those for free functional muscle transfer, such as the gracilis flap. Choosing between the temporalis MTU and the gracilis flap depends on individual patient features, patient desires, and the surgeon’s expertise and success with either technique.
Surgical anatomy
Muscle Tendon Unit
The temporalis muscle is a fan-shaped muscle that originates from the temporal fossa, passes under the zygomatic arch, to insert on the coronoid process of the mandible. The muscle fibers are arranged more vertically anteriorly for elevation of the mandible and posterosuperiorly posteriorly for retraction of the mandible. Detailed examination of the muscle shows three clear parts: (1) the superficial part, (2) a zygomatic part, and (3) a deep part. The zygomatic part of the temporalis muscle originates from the zygomatic arch to insert into the superficial part of the temporalis as it inserts into the lateral surface of the coronoid process. The deep temporalis contains muscle bundles that originated from the temporal fossa along and inserts into the medial aspect of the coronoid process and retromolar triangle down to the buccinators line.
Innervation
The muscle is innervated by the deep temporal nerves that arise from the mandibular division of trigeminal nerve and courses close to the mandibular condyle into the muscle. Typically, three deep temporal nerves corresponding to the anterior, middle, and posterior portions of the muscle are present. Intramuscularly, there is abundant intramuscular nerve fiber anastomosis from the anterior to posterior extent of the muscle. Following the temporalis MTU procedure, voluntary movement for smile production requires that the patient clenches down on the affected side. Frequent practice with biofeedback and implementation of the acquired smile to social settings is necessary to improve the natural appearance of the temporalis smile.
Vascular Supply
The temporalis muscle is supplied by the anterior deep temporal artery, the posterior deep temporal artery, and the middle temporal artery. The arteries are situated on the medial (deep) aspect of the muscle and are medial to the coronoid process. Protecting the soft tissue surrounding the coronoid process during the coronoidectomy is important in preventing injury to these vessels.
Principles and biomechanics of temporalis muscle tendon unit
The principles for MTU transfer have mostly resulted from experience in extremity surgery but are applicable in all situation of functional muscle transfer including the temporalis tendon transfer. Box 1 outlines the fundamental principles of MTU transfer procedures.
The muscle selected as an MTU donor must be expendable and functioning
Adequate soft tissue bed for the transfer tendon
Full passive range of motion of the involved joints (no fixed deformity)
Adequate excursion and length of donor tendon
Direct line of pull
Suitable insertion technique and firm fixation
Synergy of transfer
Single function for each transferred tendon
The Selected Donor Muscle Must Be Expendable and Functioning
The success of muscle tendon transfer surgery depends on the proper selection of a donor muscle. First, the MTU selected as a potential donor must be expendable in that sacrificing its function should not cause significant morbidity. The temporalis muscle works in conjunction with the masseter muscle to raise the mandible during jaw closure. In the classic transfer of the temporalis muscle where a segment of the muscle is transposed over the zygomatic arch for facial suspension, residual temporalis muscle effect on the mandible is retained. In contrast, with orthodromic transfer of the temporalis MTU the effect of the temporalis muscle on the mandible is completely lost on the side of the transfer. Clinically, one or both temporalis tendons can be transferred without significant functional deficits as long as the medial pterygoids are intact.
The donor muscle selected for MTU transfer should also be functional. Muscles that have compromised function either from direct trauma, fibrosis, or partial denervation are not ideal donors for MTU transfer. The function of the temporalis muscle should be tested clinically by observing and palpating for contraction of the muscle in the temple area when the patient is asked to bite down. Intraoperatively, the temporalis muscle can also be stimulated with surface electrodes to detect contraction. Preoperative testing of the temporalis muscle function is particularly important in patients with multiple cranial nerve injuries, Möbius syndrome, or a history of previous cranial surgery where the temporalis muscle was divided. Patients who have previously undergone the traditional temporalis muscle transfer procedure may still be good candidates for the temporalis MTU procedure if strong contraction of the remnant muscle is elicited.
Muscles Selected for Transfer Should Have Adequate Strength and Excursion
The temporalis MTU is used to replace the function of upper lip elevators, mainly the zygomaticus major and minor muscle along a single vector of contraction. When replacing the function of a deficient muscle with that of a donor MTU, the donor muscle should have adequate strength and excursion that is comparable with that of the paralyzed muscle it is replacing. Choosing a donor MTU with contraction velocity similar to the muscle it is replacing is also desirable. The strength of a muscle depends on the maximal force it can generate. The maximal force of a muscle is proportional to its physiologic cross-sectional area and its excursion range to the length of the muscle fibers. The length of the sarcomeres is a major determinant for force and excursion range. The speed of muscle fiber contraction is largely determined by the heavy chain of the myosin molecule that in turn determines the muscle type. Muscle fibers are traditionally classified into three groups depending on their physiologic behavior. Type I fibers are slow contracting, fatigue resistant, and generate small forces; type IIA fibers are fast contracting, fatigue resistant, and generate larger forces; and type IIB fibers are fast contracting, fatigue resistant, and generate the largest forces. Freilinger and colleagues distinguished the function of the facial muscles based on the proportion of muscle fiber type. The muscles that attach to the oral commissure for lip elevation (zygomaticus major, levator labii superioris) are intermediate phasic muscles with a mixture of type I and type II fibers suited for sustained tone and fast phasic movement seen in facial expression. The temporalis muscle is made predominantly of type I fibers with about 13% of type II fibers. This muscle fiber profile is adequate to maintain tone in the midface and generate the phasic contraction necessary from smile generation.
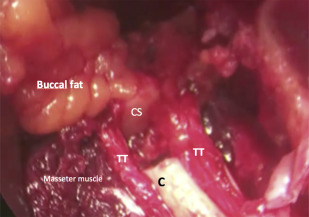
Suitable Soft Tissue Bed for Transfer
Muscles and their tendons are uniquely designed for smooth contraction and gliding by their myomysium, paratenon, and surrounding fat. For optimal contraction, MTUs should be transposed while maintaining these glide planes within a healthy soft tissue bed that is free from inflammation, edema, and scar. This is necessary to allow the tendon to glide freely untethered by adhesions and scar. The importance of an optimal soft tissue bed in MTU transfer has long been recognize as noted by Steindler in 1919 who advocated for achieving soft tissue equilibrium, in which edema is resolved, joints are supple, and scars are soft, before proceeding with tendon transfer surgery. The temporalis tendon is commonly transposed through the buccal space to reach the oral commissure. Buccal fat pads should be preserved as soft tissue cushion that separated the transposed temporalis tendon from the surrounding muscles and bone. The buccal fat pad fills the masticator space and consists of a main body and four extensions: (1) buccal, (2) pterygoid, (3) superficial, and (4) deep temporal. The deep temporal extension of the buccal fat pad lies directly over the temporalis muscle and its tendon separating it from the zygomatic arch. Disruption of the deep temporal fat pad risks scaring of the muscle fibers and tendon to zygomatic arch and disruption of its smooth contraction. The extension of the buccal fat pad into the buccal space passes anterior to the masseter and overlies the buccinator muscle as it courses to the lip musculature. The transposed temporalis tendon passes through the buccal extension to reach the melolabial crease and modiolus. To maintain a gliding path for optimal tendon movement, an adequate cushion of vascularized fat should be preserved on all sides of the tendon ( Fig. 1 ).