What is the difference between “headache” and a “migraine headache”?
• A migraine is a specific type of headache which meets diagnostic criteria that is sub-categorized by the presence or absence of an aura (reversible neurological symptoms preceding the onset of migraine).
• Migraine without aura is defined as ≥5 attacks that (1) last 4 to 72 hours; (2) include ≥2 specific qualities (pulsating, unilateral location, moderate–severe intensity, aggravation by routine activities); and (3) associated with nausea/vomiting or photophobia.
• Migraine with aura is characterized by ≥2 episodes of headaches fulfilling “migraine without aura” criteria accompanied by aura ≤60 minutes in duration.
 How common are migraine headaches?
How common are migraine headaches?
• Affects 12% of the population
• Three times more common in women
 What is the pathophysiologic mechanism of migraine headaches?
What is the pathophysiologic mechanism of migraine headaches?
The exact etiology is unknown. The mechanism may involve activation of nociceptive sensory fibers of the trigeminal nerve which innervate meningeal vessels (trigeminovascular system). Altered cortical excitability and cortical spreading depression may affect the pathway. Peripheral nerve irritation/sensitization and myelin abnormalities recently have been implicated.
 What pharmacological therapies are available for migraines?
What pharmacological therapies are available for migraines?
• Acute analgesic—acetaminophen, nonsteroidal anti-inflammatory drugs, narcotics
• Acute abortive—triptans, ergotamine
• Prophylactic—beta-blockers, anticonvulsants, tricyclic antidepressants
 What nonpharmacological treatments are available for migraines?
What nonpharmacological treatments are available for migraines?
• Behavioral (e.g., avoidance of environmental triggers)
• Botulinum toxin (Botox)
• Surgical treatment
 How was a surgical option for migraine management discovered?
How was a surgical option for migraine management discovered?
Guyuron et al. observed improvement of headaches in patients that underwent aesthetic rejuvenation of the brow.
 Which patients may be considered candidates for surgical treatment of migraine?
Which patients may be considered candidates for surgical treatment of migraine?
Patients with chronic, debilitating refractory migraine headaches that persist despite treatment by a neurologist with maximal medical therapy. Imaging is obtained to rule out intracranial or rhinogenic etiologies. History and physical examination should be consistent with a nerve trigger point. Response to Botox and/or nerve block can be correlative.
 What is the surgical goal of migraine treatment?
What is the surgical goal of migraine treatment?
Decompression/deactivation of peripheral nerve triggers that have been identified preoperatively as a likely migraine potentiator (synonymous to compressive neuropathies like carpal tunnel syndrome).
 What basic anatomical structures may compress/irritate involved peripheral nerves and trigger migraine?
What basic anatomical structures may compress/irritate involved peripheral nerves and trigger migraine?
• Bone—compression through foramen/notch that nerve may exit (e.g., supraorbital foramen)
• Fascia—entrapment from fascial element (e.g., trapezius fascia)
• Muscle—compression from entry or exit into a muscle (e.g., corrugator muscle)
• Vascular—vessel crossing nerve (e.g., occipital artery)
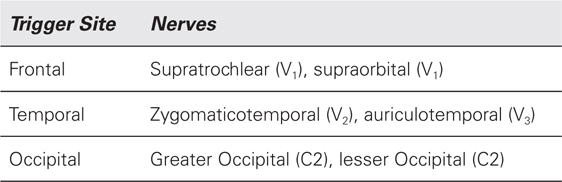
 What are the migraine trigger points and which nerves are involved?
What are the migraine trigger points and which nerves are involved?
 What are nasoseptal triggers of migraine?
What are nasoseptal triggers of migraine?
•
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree


