Supraclavicular Island Flap for Oropharyngeal Reconstruction
Michael W. Chu
Ernest S. Chiu
DEFINITION
The oropharynx is the middle part of the pharynx from the level of the soft palate to the epiglottis and is bordered superiorly by the nasopharynx and the hypopharynx inferiorly.
The supraclavicular artery island flap (SCAIF) is a fasciocutaneous, axial pattern, local rotational flap based on the supraclavicular artery.
ANATOMY
The oropharynx is a musculomucosal tube that connects the nasal cavity and mouth to the upper aerodigestive tract and serves as a conduit for air and food.
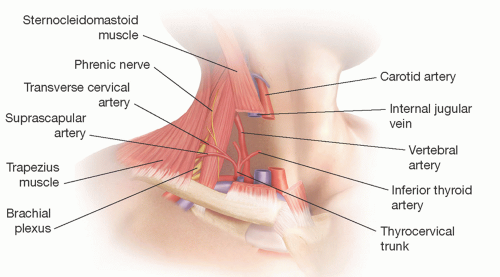
The arterial supply of the SCAIF flap is derived from the supraclavicular artery, a branch of the transverse cervical artery. The transverse cervical artery originates from the thyrocervical trunk which arises from the first portion of the subclavian artery.
Rarely, the supraclavicular artery arises from the suprascapular artery.1
The average length of the supraclavicular artery is 4 cm long (range 1-7 cm),2 and its diameter is 1 to 1.5 mm2 (FIG 1).
The supraclavicular artery can be reliably found in the supraclavicular triangle, between the sternocleidomastoid, clavicle, and trapezius.
The venous supply of the SCAIF flap is derived from vena comitantes accompanying the supraclavicular artery draining to the internal jugular vein. In addition, the SCAIF drains laterally to branches of the external jugular vein. These lateral branches are typically ligated during flap elevation.
Sensory innervation of the SCAIF flap is derived from the supraclavicular nerve arising from cervical roots C3 to C4. These nerves emerge from the deep fascia 1 to 2 cm anterior to the vascular pedicle, underneath the sternocleidomastoid muscle near the midpoint of the muscle belly.
The nerve branches proximal to the pedicle with one branch exiting anterior to the flap and the other coursing axially along the length of the flap. This provides potential for the SCAIF to be a sensate flap (Sands, 2012).
The average dimension of the skin paddle for the SCAIF flap is a length of 24.2 cm and width of 8.7 cm.3
Flap delay or tissue expansion can increase the size of the flap to as large as 12 × 35 cm.5
The arc of rotation for the supraclavicular flap has been reported up to be up to 180 degrees.1 However, caution should be used when rotating flaps greater than 90 degrees to avoid venous obstruction.6
The SCIAF flap has many advantages.
Thin, pliable, hairless flap with good color match for head and neck reconstruction
Harvest and reconstruction are in the same surgical field.
Consistent vascular anatomy with a large arc of rotation
Reliable flap blood supply that is preserved in most cases, even after neck dissection and previous radiation therapy7
Does not require microsurgical expertise and decreased operative duration compared to microsurgical reconstruction8
Primary closure of donor site if width is less than 8 cm
Disadvantages
Risk of vascular pedicle compromise secondary to torsion or kinking particularly with increased arc of rotation6
Shoulder scar is visible with certain clothing choices.
Obese patients with thick supraclavicular tissues may not be good candidates.
PATIENT HISTORY AND PHYSICAL FINDINGS
The most common cause of oropharyngeal defects is head and neck cancer. As a result, history of prior treatments (surgery, radiation) and risk factors for wound healing complications (ie, history of tobacco use, ethanol abuse, malnutrition) common in this patient population should be elicited.
If reconstruction is performed at the time of tumor extirpation, then discussions with the ablative surgeon are important to delineate flap dissection and preservation of the flap pedicle.
Physical exam should evaluate the pliability of the neck and shoulder skin, extent of prior surgery (if any), carotid pulse, lymphadenopathy, and, if possible, size and nature of the primary tumor.
IMAGING
Routine preoperative radiographic imaging is not necessary in patients with no history of prior neck dissection.
In patients who have previously undergone neck dissection (ipsilateral to the proposed flap site), angiography (CTA or MRA) can be done to confirm patency and characterize anatomy, vessel length, patency, and diameter of the supraclavicular artery.
Handheld Doppler can also be used to confirm location and patency of the supraclavicular artery preoperatively and intraoperatively.
Indocyanine green laser angiography is occasionally useful to evaluate perfusion of the SCAIF after the flap has been elevated.
SURGICAL MANAGEMENT
Reconstructive goals of oropharyngeal reconstruction are to promote rapid healing, re-establish the aerodigestive tract, and prevent wound complications and infection.
The main steps of the procedure are as follows:
Measure defect dimensions.
Design skin paddle centered over the axial course of the vascular pedicle.
Raise fasciocutaneous flap from lateral to medial.
Mobilize flap into defect.
Inset the flap by tunneling or interpolating the flap, or transpose the flap by islandizing the flap (propeller flap).
Close the donor site (primarily or with skin grafts).
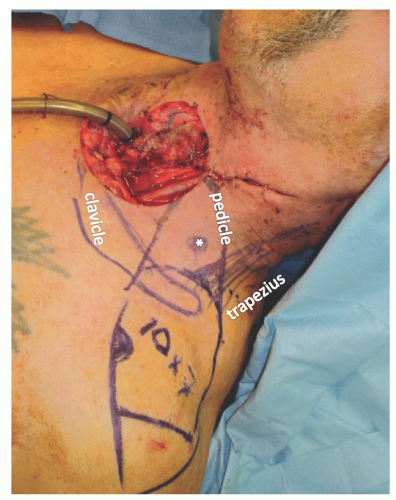 FIG 2 • Design of a supraclavicular arterial island flap measuring 10 × 7 cm. The asterisk represents the supraclavicular artery vascular pedicle found in the triangle delineated by the clavicle, sternocleidomastoid, and trapezius muscle.
Stay updated, free articles. Join our Telegram channel
Full access? Get Clinical Tree
 Get Clinical Tree app for offline access
Get Clinical Tree app for offline access

|