Subciliary Skin Versus Subconjunctival Approach
Jane Jenison Olson
EDITOR COMMENTARY
In this chapter, Dr. Jenison Olson introduces the reader to the approaches to cosmetic lower eyelid surgery. It necessarily considers not only the surgical approach but also the treatment of orbital fat and lower eyelid support.
Aesthetic surgical management of the lower eyelid has evolved over several decades. Given the unforgiving nature of the lower eyelid, a number of approaches have been tried but then abandoned because they resulted in complications or inadequate results. Today, there is no single ideal procedure; rather, individual surgeons select from a spectrum of techniques based on their experience and patient goals.
The surgeon gains access to the lower eyelid and cheek structures from the subciliary skin or transconjunctival approach. In addition to incisional technique, consideration is given to how the orbital fat will be handled, options to smooth the lid contour and camouflage the exposed orbital rim, treatment of skin discoloration and textural rhytides, and control of the lower lid, lateral canthal, and palpebral fissure shape. The contour of the eyelid-to-cheek transition and the structure of the midface, with descent of the malar fat pad and accentuation of malar mounds, all affect the lower eyelid appearance. Midface lifting surgery can be done in conjunction with or subsequent to blepharoplasty, but it is in its own stage of controversy and evolution and will be discussed by other authors. Although the patient and the surgeon must evaluate and discuss facial concerns, many patients are not prepared to undergo entire face lifting to achieve periorbital rejuvenation, and not all patients will require manipulation of all these structures.
Lower eyelid blepharoplasty was described in the 1980s as excision of excessive skin, herniated orbital fat, and hypertrophic orbicularis (1,2). Surgery primarily involved fat removal, replacing the lower eyelid convexity with a concavity (3). The transconjunctival approach, although described in 1924 (4), was popularized over the past 20 years (5, 6 and 7). It is used to avoid cutaneous scarring and interruption of orbicularis muscle, and to decrease the incidence of eyelid retraction. Combined skin and skin-muscle flap technique also was described to preserve pretarsal orbicularis muscle yet allow for skin trimming (8).
The suboptimal results sometimes caused by using any single approach led authors to develop more extensive surgery to prevent lower lid retraction, augment lid support, and address malar festoons, including canthopexy (9,10), tarsal strip (11), and extended lower lid blepharoplasty with orbicularis plication to the periosteum (12). Development of reconstructive techniques was necessary to correct iatrogenic lid malpositions from aesthetic blepharoplasty, such as the “Madame Butterfly” procedure (13,14), hard palate grafting (15,16), and midface lifting (17,18).
In the last decade, techniques have been introduced that tout orbital fat preservation (19, 20 and 21), release of ligamentous attachments of the lower eyelid (22, 23 and 24) to mobilize the orbicularis for tightening and redraping, and lateral canthal support (25,26). Complications such as extraocular muscle restriction (27), persistent fat protrusion and lid edema (28), and lid retraction (22) from fat redraping are reported from these aesthetic reconstructive procedures. The higher incidence of morbidity and disappointing results associated with aesthetic surgery of the lower eyelid relative to other facial procedures has stimulated innovative surgical contributions from oculofacial plastic surgeons, general plastic surgeons, facial plastic surgeons, and anatomists.
Contemporary Techniques in Periorbital Rejuvenation
Current surgical procedures in primary aesthetic periorbital rejuvenation now focus on preservation of soft tissue and prevention of soft tissue descent. Yet, surgery does not restore youth. Rather, my goal is to approximate the illusion of youthful contours, soften skin rhytides, take the eye away from the caricature signs of aging, and avoid telltale surgical signs. Foremost, lower eyelid function must be preserved, including orbicularis function, vertical lid position and excursion, and correct lid margin and punctal position. Still photographs may document an ideal lid contour and position, but they may not reveal poor lower eyelid excursion.
In discussing my approach to the lower eyelid, I will articulate some of the controversy that surrounds each technique. I design a customized plan for each patient that is as simple as possible yet achieves mutually discussed goals. It includes the following components. Risk of the procedure for each individual is taken into consideration, along with the patient’s motivation. Patient goals and lifestyle are assessed, options and alternatives are presented, and a joint decision is made for a treatment plan. Sometimes this may include a simpler procedure to start, with options for additional procedures later. A combination of surgery and treatment of textural and dynamic rhytides may provide the most comprehensive effect on the lower eyelid area. The following case presentations illustrate a spectrum of techniques and points of controversy that arise.
EDITOR COMMENTARY
As Dr. Jenison Olson indicates, cosmetic eyelid surgery and adjunctive procedures do not restore youth. As surgeons, it is our responsibility to educate patients.
Case 1
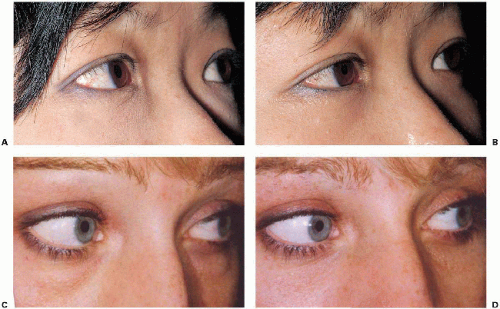
A 32-year-old Asian woman has familial prominent orbital fat, good skin texture, and high position of the malar fat pad with adequate maxillary projection (Fig. 4.1.1A).
A transconjunctival blepharoplasty is performed with removal of the bulging areas of anterior orbital fat. I use incisional ultra pulsed CO2 laser to make an incision midway between the inferior tarsal border and inferior fornix from the caruncle to the lateral canthal angle. This is deepened to expose the nasal, central, and lateral fat pads, identifying the inferior oblique muscle. The arcuate expanse of the inferior oblique is severed to allow the central and lateral fat pads to become one. The fat is allowed to prolapse from its capsule gently and is not clamped. The fat is appropriately contoured by incising and defocusing to cauterize as necessary with the CO2 laser. The lid is placed on upstretch to check the contour while the patient is supine, and again in the sitting position at the end of the case. The conjunctiva may or may not be closed, as desired.
EDITOR COMMENTARY
The indications for transconjunctival blepharoplasty are rare, except in the very young. In most cases, treatment of the anterior lamella and lateral canthus is necessary. Younger patients with excellent skin elasticity may not require any anterior lamellar tightening. Analysis of the preoperative photograph provided by Dr. Jenison Olson suggested that this patient may require anterior lamellar tightening as provided by the three-step technique outlined in Chapter 2.The lower eyelid skin medially appears somewhat thin. Resurfacing this patient with pigmented skin may provoke long-term hypopigmentation.
Nonetheless, the postoperative photograph (Fig. 4.1.1B) demonstrates an excellent result with transconjunctival blepharoplasty alone. Photographs of one of the few patients in my practice who underwent a simple transconjunctival blepharoplasty are provided (Figs. 4.1.1C and 4.1.1D).
Nonetheless, the postoperative photograph (Fig. 4.1.1B) demonstrates an excellent result with transconjunctival blepharoplasty alone. Photographs of one of the few patients in my practice who underwent a simple transconjunctival blepharoplasty are provided (Figs. 4.1.1C and 4.1.1D).
Case 2
In some young patients there is a “tear trough” configuration or nasojugal groove inferomedially with a depressed area along the inferonasal orbital rim (Fig. 4.1.2A).
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree