Staged Pedicle Flaps
INTRODUCTION AND FLAP DYNAMICS
Most operative wounds are suitably repaired with local adjacent tissue transfers. When a local flap is not able to achieve an aesthetic closure a staged interpolation flap may be utilized. Interpolation flaps are delayed pedicle flap reconstructions in which a flap of tissue is elevated at one location and transposed over intervening skin to an operative wound. The flap is left in place for a defined period of time in order to vascularize from the recipient bed, and then the pedicle is severed. Interpolated pedicle flaps allow for the reconstruction of challenging operative wounds, in particular wounds of the nose, ear, and lip.
The history of pedicle flaps dates to ancient India and has been artfully reviewed. The most well-known pedicle flap is the paramedian forehead flap, which is based on the rich vasculature of the supratrochlear region.1–4 The great benefit of a forehead flap or cheek interpolation flap is the ability to tap into a reservoir of suitable tissue at a substantial distance away from its intended target defect. Other than the mastoid pedicle flap, all of the flaps discussed herein have a robust, predictable vascular supply, allowing them to have a narrow and highly mobile base. The paramedian forehead flap carries within it the supratrochlear artery and vein or branches thereof. The cheek-to-nose pedicle flap is supplied by large perforating vessels from the angular artery. The Abbe-Estlander flap contains the labial artery. The inclusion of a single larger caliber vessel in such pedicles increases the blood supply to the flap by a factor of 625, and it is usual for a very long, narrow pedicle flap to have arterial bleeding from its distal tip after complete elevation.
Pedicle flaps require a substantial knowledge and understanding of anatomy, surgical planning, and surgical skill. Properly designed interpolation flaps can recreate a distal nose so well that it appears to be a native nose at a conversational distance. This, however, requires a precise plan, meticulous operative technique, and an attention to detail both at the initial flap creation and at the flap takedown. While failure of a local flap is problematic, complete failure of a pedicle flap can be devastating. The recipient site for a pedicle flap must be deep enough to receive a full-thickness operative repair, and must have the appropriate support structure to shape the flap and recreate a native aesthetic contour. In some instances, particularly on the distal nose, this may entail the need for mucosal repair and/or cartilage graft placement.
Pedicle flaps with appropriate planning have an excellent arterial blood supply, even when the pedicle is narrow. A wider or deeper pedicle may be needed in order to assure adequate venous drainage. While the portion of the flap placed in the operative wound may have very little subcutaneous tissue, the same cannot be true of the nourishing stalk or pedicle. Also, pedicle flaps are designed to be sewn into place under little to no tension. Tension and torsion of a pedicle can lead to flap failure and should be avoided.
Because interpolated pedicle flaps require patients to live for at least several weeks with a deformed appearance, appropriate preoperative consultation is essential. All pedicle flaps require at the very least one revision (the flap takedown), and patients should be counseled that further revisions and modifications may be needed. While pedicle flaps can be accomplished in smokers, flap failure is more likely in this subgroup of patients and appropriate counseling is needed.
As reconstruction has evolved, the use of staged pedicle flaps has expanded greatly. While local flaps are often preferred, pedicle flaps are able to repair devastating operative wounds and allow a level of subunit reconstruction and cosmesis that are beyond compare. For that reason this chapter is expanded to include multiple examples of nasal reconstruction with a variety of techniques. The basic mastoid-to-ear and Abbe-Estlander flaps are covered as well.
REGIONAL APPLICATION
Nose
Paramedian forehead flap
Since the antiquities, the forehead has been used to recreate the nose. The history of the forehead pedicle flap has been artfully reviewed,5 and the rationale for the use of forehead skin for a nasal substrate has been eloquently elaborated by the famous Sir Harold Gillies:
The tint of forehead skin so exactly matches that of the face and nose that it must be first choice. Is not the forehead the crowning feature of the face and important in expression? Why then should be jeopardize its beauty to make a nose? First, because in many instances, the forehead makes far and away the best nose. Second, with some plastic juggling, the forehead defect can be camouflaged effectively.6
The paramedian forehead flap and the art and science of nasal reconstruction have been delineated with excellence in two outstanding full-length books. The first is Aesthetic Reconstruction of the Nose authored by Gary C. Burget and Frederick J. Menick, published by Mosby in 1994. The second is Nasal Reconstruction by Dr. Menick, published by Saunders in 2008.
Anatomy
The upper forehead skin has a sebaceous quality that matches the sebaceous nose and is of a suitable thickness to fill a deeper nasal operative wound. The vascular
supply for the forehead flap is highly predictable. The supratrochlear artery is usually located just medial to the brow within the glabellar crease at a distance of about 1.5 to 2 cm from the mid glabella. The artery can be reliably identified by Doppler at this site. The artery emerges from the supratrochlear foramen, ascends over the belly of the corrugator supercilii, pierces the frontalis muscle, and then ascends vertically as multiple branches on the forehead, reaching the superficial subcutis midway up the forehead. Therefore, the pedicle of the paramedian forehead flap contains skin, subcutis, musculature, and an axial vessel. While there is some debate about the importance of retaining an axial vessel in a forehead flap, the supratrochlear artery is easily seen entering the base of the flap as the repair is elevated.
Forehead flap design and preparation
The operative wound for a forehead flap should be enlarged, as appropriate, to encompass a subunit or several subunits. Because pedicle flaps have the tendency to retract and pincushion somewhat during healing, if a round wound is reconstructed with a forehead flap, the result may be a pincushioned blob of tissue. In practice this most commonly involves either the alar subunit or the distal nasal subunit. Not all forehead flap repairs need to be subunit reconstructions, but consideration should be given to this approach for the optimal cosmetic outcome. All wounds should be nearly skeletonized, excising all tissues down to the perichondrium and periosteum (Fig. 6.1). Wounds that are not innately stable or are lacking in mucosal integrity require advance preparation with mucosal flaps, inverted skin grafts and/ or cartilage grafts. These procedures are discussed in Chapter 7, while the focus of this chapter is on the pedicle flap itself.
Figure 6.1 A skeletonized operative wound of the nose is an appropriate defect to repair with a paramedian forehead flap
For most forehead flaps, the contralateral supratrochlear location is identified and utilized as the flap base. For a defect on one side of the nose, the pedicle is rotated through a less acute angle and therefore is subjected to less torsion if the flap comes from the contralateral side. In midline cases the flap may be elevated from either side, and the choice is often determined based on the quality of the forehead skin and the presence or absence of any forehead lesions. For that matter, the forehead should be carefully examined prior to flap elevation, as the presence of extensive sun damage, precancerous lesions, or even a separate skin cancer may either negate the use of the forehead altogether or suggest using an ipsilateral pedicle. In addition, some foreheads are high and arching, thus, making forehead flap design easy, whereas other foreheads are very short with a low hairline, in which case extensive design changes may be needed and a cheek-to-nose pedicle may be more appropriate.
A template of the operative wound is obtained (Fig. 6.2). This can be done with the sterile foil of a suture packet or with sterile gauze. For a contralateral pedicle, the template is inverted, rotated, and moved to the forehead. In obtaining a template over a convex surface, it is important to use a form that will take into account the curvature of the underlying structure. A common error is to undersize the flap by basing the template size on only the horizontal dimension of the wound. On the other hand, if a subunit repair is to be undertaken, the template should be created prior to excision of the remaining subunit in order not to overestimate the operative wound secondary to peripheral wound contraction.
Figure 6.2 A template of the operative wound is created and takes into account the curvature of the distal nose
When the template has been transferred to the forehead, the length and dimensions of the flap should be delineated and marked. The length of the flap should be designed so that the distant tip of the template will reach its target under little to no tension (Fig. 6.3). The narrowest safe pedicle width should be chosen. A 7 to 8 mm margin on either side of the glabellar crease will reliably produce a flap with abundant vascular supply and drainage, and in most cases an overall pedicle width of 1.5 cm is a safe plan. Many surgeons prefer to Doppler the supratrochlear artery, but this step is not routinely necessary.
Figure 6.3 A pedicle is created on the forehead based on the supratrochlear vessels and frontalis. The flap must be long enough to reach the distal nose easily
The two-staged paramedian forehead flap
Execution step by step
Flap elevation: The forehead is appropriately prepped and anesthetized. A supraorbital and supratrochlear block will provide dense and long-lasting anesthesia. Local anesthesia higher on the forehead including epinephrine will make execution of the flap easier. The flap is first incised along its entire margin through to subcutis, and hemostasis is obtained. The portion of the flap that will become nasal tissue is elevated above frontalis. Once this portion of the flap has been elevated, the frontalis and galea are incised and the remainder of the flap and pedicle are elevated in the loose tissues above the periosteum. The corrugator is approached under direct visualization and the emerging supratrochlear vessels are preserved. The properly designed flap will at this point drape over the operative wound with no tension (Fig. 6.4). If further release is needed to achieve this, an incision may be carried out through the brow and the deep dissection may proceed beneath the corrugator or, with great care, the vessels may be preserved by dissection gently over the corrugator.
Figure 6.4 The pedicle is elevated and drapes easily over the operative wound
Initial flap inset: The defect should be squared off with an appropriate bevel to receive the forehead flap. Some surgeons will employ a bevel-antibevel closure, especially at the distal extent of the repair. The flap should be meticulously thinned to a thickness appropriate for the location and type of nasal skin to be replaced. In most cases the repair is most aesthetic with substantial thinning. This is done under direct visualization. Most of the subcutaneous adipose tissue may be removed while leaving in place the vertical and branching vessels of thesubdermal plexus (Fig. 6.5). Pulsatile arterial flow will usually be observed in several locations just beneath the dermis at the flap tip. If any hair has been elevated within the flap tip and will be transferred to the nose it may be electroepilated at this point. The flap is sutured into place mainly with surface sutures but in a few key locations buried dermal sutures may be employed (Fig. 6.6). For large operative wounds in which a concavity is resurfaced, through-and-through sutures may be employed to tack the flap down to the depth of the defect in order to close dead space and anneal the depth of the flap to the recipient bed.
Figure 6.5 In a standard two-staged paramedian forehead flap, the portion of the flap used to recreate the nose is thinned of most subcutaneous tissues. The distal extent of the branching subcutaneous arteries can easily be seen and such vessels are preserved
Figure 6.6 Flap at immediate closure. A bevel or antibevel approach along the distal aspect may be of benefit
The pedicle
The pedicle has a raw deep surface from its origin to the sutured portion of the repair. Meticulous hemostasis should be achieved by pinpoint electrocoagulation of any vessels bleeding on the exposed stalk. In some cases a small pulsatile vessel may require ligature. The pedicle tends to ooze postoperatively as epinephrine from the local anesthetic wears off. For that reason it is worthwhile to apply a layer of Surgicel° to the exposed pedicle, which substantially reduces bleeding the evening following the procedure. Many surgeons have performed a skin graft on the posterior surface for neatness, but this adds a secondary procedure and is not necessary. A “no care” dressing may be achieved by carefully wrapping the pedicle with Vaseline-impregnated gauze (Fig. 6.7).
Figure 6.7 Wrapping the pedicle with Surgicel° followed by a petrolatum-impregnated gauze may diminish minor postoperative bleeding and obviates a portion of wound care
The forehead
While little attention is paid to the forehead in many texts, and the forehead is, in a way, sacrificed for the sake of the nose, a poorly closed forehead wound does create disfigurement. The forehead should be suitably undermined and closed with attention to fascial closure where feasible to prevent an inverted or depressed scar. Where the wound cannot be closed entirely, a series of horizontal mattress sutures can be used to diminish the size of the remaining operative wound. Given that the forehead will usually heal well by second intention, it is rarely necessary to create substantial flaps or to force complete forehead wound closure. A very tight closure on the forehead can be exceedingly painful in the postoperative period and should be avoided.
Division
While a pedicle flap may survive severing after several days, the most reliable time frame for division is approximately 3 weeks. During that period the flap is heavily vas-cularized with anastomoses from the operative wound bed. If there is concern about viability, the division can be slightly delayed, but most flaps are ready for division at this time frame and are hypervascular. The division is done deliberately. First, the pedicle source is severed. The pedicle will have partially reepithelialized, and substantial granulation tissue will have accumulated at the supratrochlear origin. Either the entire stump may be excised and repaired linearly, or the stump may be inset as an inverted V-Y repair. In either case all edges should be sharply freshened, and all accumulated granulation tissues should be sharply excised. If the inverted V-Y closure is chosen, the V should be slightly inset to prevent a common aesthetic detraction, namely a pincushioned glabellar deformity (Fig. 6.8).
Figure 6.8 The flap stump should either be entirely excised and repaired linearly or inset carefully as a V-Y closure. Here the V-Y is being prepared
The flap inset is accomplished by redefining the original operative wound or subunit, meticulously thinning the flap, and then sewing the flap into place. The lateral margins of the flap are first sharply debrided to a squared off edge. The original wound edges or subunits are sharply incised to the nasal skeleton, and all remaining deep tissues are excised at a periosteal or perichondrial level. The accumulated granulation tissues are then excised en bloc and the flap is thinned of all tissue other than a thin layer of subcutis. Depending on flap thickness and how well the flap has annealed to the underlying nasal structure, it may be necessary to remove granulation tissue and thin a substantial portion of the flap. The flap takedown offers the best opportunity to thin and contour the tissues for an aesthetic long-term result. After appropriate thinning the flap should be sewn in under slight tension, trimming the flap or adjacent tissues as needed (Fig. 6.9).
Figure 6.9 The flap is meticulously thinned and trimmed, then closed
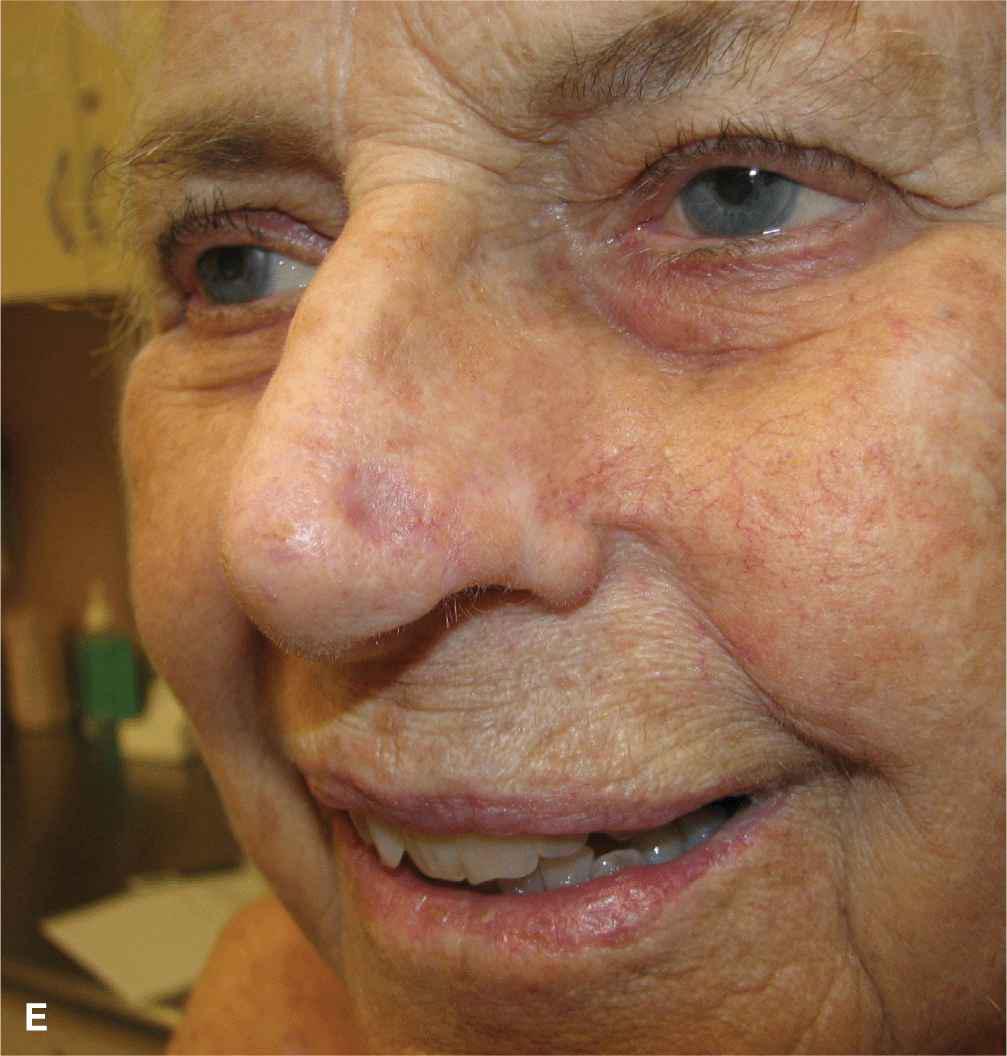
Healing and expectations
Properly designed and executed forehead flaps can produce results that are almost imperceptible at a conversational distance, particularly when used to recreate an ala or a distal nasal subunit. Forehead flaps used to repair upper nasal wounds have more of a tendency to pincushion, especially if the entire upper nose is not resurfaced. All patients undergoing pedicle flap reconstructions should be counseled up front that some revision may be necessary. Usually, healing proceeds without incident, and over a time frame of 1 year the flap becomes sensate and original cosmesis is restored satisfactorily.
Three-staged forehead pedicle flaps
Some surgeons have moved to a three-stage reconstruction technique for the paramedian forehead pedicle flap.7 The three-staged forehead flap enables aggressive and meticulous thinning of the entire flap, and it allows for the secondary insertion of cartilage grafts as indicated for nasal support and contour. In a three-staged repair, the forehead flap is elevated and inset much as in the two-staged repair, albeit the frontalis is left attached to the entire flap at its depth. It is argued that this leads to less fibrosis, less wound contraction, and improved cosmesis, although side-by-side studies have not been completed. The second stage of the repair that is accomplished several weeks later is to elevate the entire flap back off of the nose and excise all of the underlying frontalis and much of the adipose tissue. At this point delayed cartilage grafts may be inserted. A second delay period is then employed, following which the flap is divided and inset.
The three-staged forehead flap has the likely advantage of being more reliable in smokers and those with severe comorbid factors, as the flap contains muscle and has a very robust blood supply. It may also be of benefit in cases where a profound underlying lining and cartilaginous reconstruction has been performed, as the frontalis provides an extremely rich anastomotic vascular network. The obvious disadvantage is the need for an extra procedure and the time delay involved. Because most of the large operative wounds facing the dermatologic surgeon are in somewhat older individuals with manageable wounds, the two-staged procedure remains less of an encumbrance, is better tolerated, and creates a repair that is of suitable cosmesis for patient satisfaction.
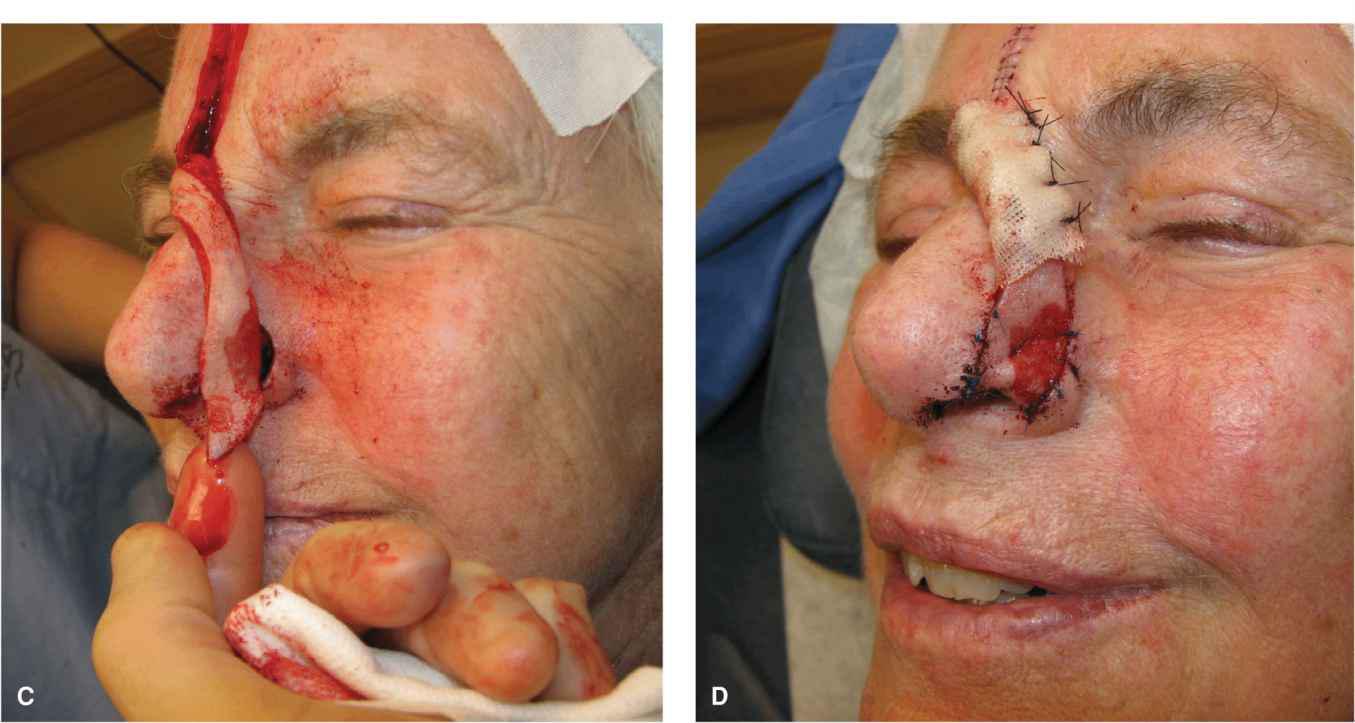
Foldover flaps
The lining of the distal nasal aperture and the alar margin can both be repaired with a forehead flap of adequate length and vascularity (Fig. 6.10)5. The lining of the distal nare is cutaneous, and even a portion of the mucosal lining can be repaired using forehead flap tissue. For this to be suitable, the forehead must be high enough and the reach of the forehead flap must be adequate to both line the distal nose and then fold over to create the external surface. This does place actinically exposed skin into the nose that warrants subsequent observation. A foldover flap must satisfy two seemingly mutually exclusive features. It must have adequate perfusion to tolerate partial kinking, and it must be thin enough to avoid the creation of a bulky ala. Fortunately, the distal flap may be thinned almost to dermis, preserving the very shallow arterial and venous supply of the upper forehead. As the flap folds on itself, it creates a sandwich that actually stabilizes the absent ala. While in some cases it is helpful to fold the flap around a cartilage brace, in other cases this is not necessary. If the flap is adequately vascular, several through-and-through sutures can be placed to anneal the anterior surface to the recreated inner lining. Foldover flaps are particularly suited to distal wounds in older patients or in patients who have had prior septal surgery or rhinoplasty.
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree


















