This article is a discussion and presentation for plastic surgeons, in which each section is dedicated to a principle necessary for complex wound reconstruction. Each principle is discussed and includes detailed images of the associated operations.
- •
Planning is critical to the outcome of all plastic surgery procedures.
- •
Keep a “lifeboat,” as one never knows when a problem will recur or an initial solution will fail.
- •
Replace “like with like” to ensure an optimal reconstruction using the best available tissue.
- •
Use all spare parts before taking tissue from a virgin donor site.
- •
Replant when possible, as amputated parts are still typically the best reconstructive option.
- •
Preserve length whenever possible in reconstructing extremities to maximize functionality.
- •
Consider all tissue layers and, where possible, laminate or fold flaps to obtain lining where this is needed.
- •
Innovate when undertaking complex wound reconstruction as more elegant solutions may be available to those who think laterally.
Introduction
Plastic surgery has traditionally been thought of as “surgery of the skin and its contents.” Because of this breadth and scope, plastic surgeons have been guided by the reconstructive ladder, consisting of a hierarchy of techniques:
- •
Healing by secondary intention
- •
Primary closure
- •
Delayed primary closure
- •
Split-thickness skin grafting
- •
Full-thickness skin grafting
- •
Tissue expansion
- •
Random flaps
- •
Axial flaps
- •
Free flaps.
Each of these options can be used individually, in combination, or with multiple variations. Together they form the complete armamentarium of the plastic surgeon, and allow complex wound problems to be repaired while maintaining optimal form and function.
The advent of microsurgery in the 1970s allowed a quantum leap in terms of reconstructive options. Free tissue transfer has allowed coverage of larger and more complicated defects with adequate quantities of tissue, “like-with-like” tissue, and even multiple tissue types in the forms of composite tissue transfers. Tailored flaps are able to be produced using distant tissue that most appropriately replicates lost tissue; this may even take the form of prefabricated or prelaminated flaps where necessary. In addition, free tissue transfer has multiplied the options and provided “lifeboats,” which may be necessary in complex reconstructions.
Free (and pedicled) tissue transfer has been further augmented by a thorough understanding of perforator anatomy, which has brought about the use of freestyle flaps. These flaps further expand the options for donor sites while minimizing donor-site morbidity and maximizing the concept of like-with-like tissue transfer.
A further extension of these concepts has occurred over the last decade, during which time there has been a move from reconstruction to restoration. Restoration using tissue transplantation can provide the most perfect match for complex tissue replacement. In this situation plastic surgeons are no longer “making do” with similar tissues, but are truly restoring anatomy. This approach is especially relevant to facial or hand transplantation, where no other part of the body produces an ideal alternative to the original tissue.
Despite the principles of the reconstructive ladder, free tissue transfer, and tissue restoration, and the ever increasing options available to plastic surgeons through innovative use of multiple modalities, there are numerous principles that hold true. These principles underscore some of the more sophisticated surgical solutions for complex wound problems. Each section in this article is dedicated to a principle necessary for complex wound reconstruction.
Planning is critical
Careful planning of preoperative, operative, and postoperative steps applies to all reconstructive surgery. However, planning is particularly important when undertaking unique or tailor-made reconstructive operations, and critical when reconstruction requires multiple steps. This reasoning is particularly true for complex wound problems whereby many plastic surgical operations are based on principles rather than on repetitive and sequenced operations. In these situations it is very important to ensure maintenance of tissue vascularity and viability while not burning bridges for future options or stages. Expecting the unexpected through careful planning is crucial.
Planning involves several steps. A thorough literature review or discussion with other experts may be important when novel or innovative techniques are being used. This action may necessitate drawing out expected vascular patterns, nerves, and flap dimensions to make sure that a plan is executable. In the operating room, testing the reach of a flap is important to ensure that it is adequate for the intended coverage. In some instances, alginate molds may allow the 3-dimensionality of a reconstruction to be accommodated. During follow-up, photographs of intraoperative and postoperative findings are important in order to learn from a complex reconstruction and its results.
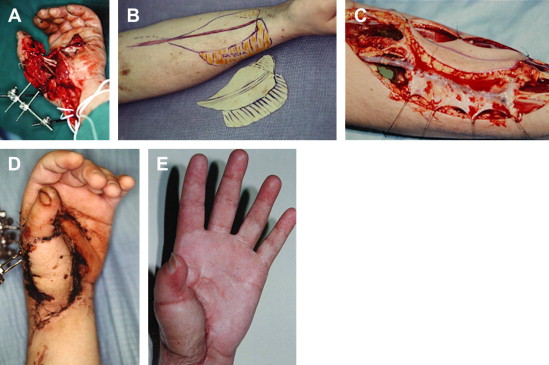
Unique repairs require planning more than any other situation. Fig. 1 demonstrates a traumatic volar thumb injury. Despite significant soft-tissue defects, maintenance of the thumb is crucial to maintaining hand function. The first stage in this repair involves debridement of all nonviable tissue. An external fixator is placed to maintain a bony stability while the remaining soft tissues are repaired and heal. The flexor pollicis longus tendon is repaired using a tendon graft. A tailored radial forearm flap is then used, and the underlying vascularized fascia maintained with it to allow a gliding surface for the tendons. Through careful planning, a very functional and cosmetically acceptable result is obtained.
Keep a “lifeboat”
Keeping a lifeboat is another very important principle that underscores complex wound repair. Sophisticated solutions do not always work as planned, and alternatives must always be kept in mind. Experienced plastic surgeons are aware that the part of the flap that fails is typically the most distal aspect, and this is usually the most important part needed to cover critical structures. As a result, anticipating potential complications or flap losses and maintaining an alternative wherever possible is important. Lifeboat alternatives may be required intraoperatively or for a second procedure, and it is important not to burn bridges in terms of vascularity, scarring, or compromising donor sites unnecessarily.
Where lifeboats are limited, prefabrication of a flap may be used. This technique involves bringing a blood supply to tissues where no axial blood supply previously existed. Prefabricating a flap allows donor sites, which could not otherwise be used, to be transferred on their implanted vascular pedicle, after a period (usually 8 weeks) of revascularization.
Replace like with like
The principle of replacing like tissue with like tissue is central to complex wound reconstruction and continues to be a fundamental principle of plastic surgery. Like tissues may require significant innovation. Fig. 2 shows an example of Achilles tendon reconstruction after a sarcoma resection. Although native Achilles tendon is unavailable, the use of folded vascularized fascia lata allows a close approximation and allows not only vascularized coverage of the skin defect but also functional reconstruction of the Achilles tendon.
Use all spare parts
Another key principle is to consider the option of using spare parts. Using parts that would otherwise be discarded including amputated parts, “dog ears” at wound edges, or segmentally resected tissue is an ideal way to minimize donor-site morbidity while potentially preserving irreplaceable tissue. The opportunity to replant a part is the ultimate example of replacing like tissue with like tissue.
In any surgery involving complex reconstruction, the surgeon should avoid throwing away any tissue, including fat, skin, and vessels for grafting, until a reconstruction is completely finished, to avoid the need to harvest further tissues later.
The principle of using all spare parts is particularly applicable in the hand. Using tailored grafts and flaps from adjacent fingers or the feet and using tissue rearrangement, heterotopic replantation, or ectopic replantation allows the surgeon to maximize function and minimize donor-site morbidity.
One such example of this is the use of a fascial extension and palmaris tendon when using a radial forearm flap to provide a gliding and vascularized graft ( Fig. 3 ).
Another example of this principle is shown in Fig. 4 . The thumb is so valuable that rarely will a reconstruction from scratch be as good as a native thumb. Maintenance of whatever is left after severe trauma is attempted at the primary stage. Additional tissue can then be transferred as a free flap from such sites of the toe, giving an excellent esthetic and functional reconstruction.
Segmental injuries either from trauma or surgical resections can cause the loss of proximal tissue while distal tissue remains viable. When this occurs in the lower extremity, a Van Nes rotationplasty can convert an above-knee amputation into a functional below-knee amputation by using the ankle joint as a pseudo-knee. Functionally, this dramatically reduces energy expenditure and allows placement of a below-knee prosthesis with active knee flexion ( Fig. 5 ).