16 Sling Procedures for Stress Urinary Incontinence
HISTORICAL PERSPECTIVES
The vaginal approach for the surgical management of urodynamic stress urinary incontinence (SUI) associated with urethral hypermobility and intrinsic sphincter deficiency (ISD) has been comprised of a wide variety of procedures based on different surgical principles. Historically, suburethral sling procedures have been reserved for patients with severe stress incontinence, previous surgical failures, and patients who have significant ISD. Until recently, anterior colporrhaphy with Kelly’s plication and transvaginal needle suspension procedures were used for the transvaginal repair of primary stress incontinence and associated urethral hypermobility. Numerous studies, however, have shown that the objective success rate after anterior colporrhaphy and suburethral plication is significantly less than what could be achieved with retropubic colposuspension or a suburethral sling procedure. For this reason, suburethral plication should no longer be considered as a procedure for the correction of stress incontinence and should only be performed as part of an anterior colporrhaphy or cystocele repair without incontinence or in the occasional elderly patient with mild incontinence in whom surgical morbidity should be kept low (see Chapter 19).
The tension-free vaginal tape (TVT) procedure was developed in the 1990s by Petros and Ulmsten (1990), 1995). The concept behind this procedure is that stress incontinence results from the failure of the pubourethral ligaments in the midurethra. The “integral theory” for the management of stress incontinence was based on the model that continence is maintained at the midurethra and not at the bladder neck. The aim of the tape (sling) is to reinforce the functional pubourethral ligaments and hence secure proper fixation of the midurethra to the pubic bone, allowing simultaneous reinforcement of the suburethral vaginal hammock and its connection to the pubococcygeus muscles. This operation introduced two new concepts to the mechanism of cure for slings: placement at the midurethra, and placement without tension. Numerous cohort studies and a large clinical volume worldwide seem to show that the TVT procedure (and other variations of midurethral slings) is equivalent to other operations for cure of continence, with a quicker return to normal voiding and fewer postoperative complications. The other important innovation of the TVT was that it could be done under local anesthesia as an outpatient, and often patients could void the day of surgery and be discharged home without a catheter.
TYPES OF SLINGS
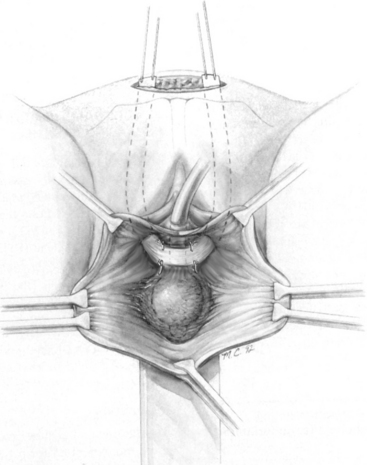
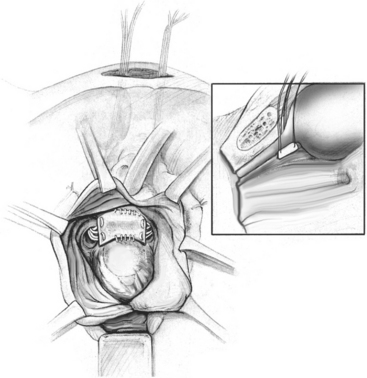
Currently, suburethral sling procedures can be broadly classified into bladder neck and midurethral slings (Box 16-1; Fig. 16-1). Slings can be made of a biologic material and are placed at the level of the proximal urethra and bladder neck or a synthetic material placed either under the proximal or midurethra. The currently used biologic materials are divided into autologous tissue, which is harvested from the patient who is undergoing the sling; allograft material, which is most commonly cadaveric fascia lata; or xenografts, which are harvested from various animal sources. Proximal urethral slings are called pubovaginal slings when the arms of the material used are connected to the anterior rectus fascia on each side.
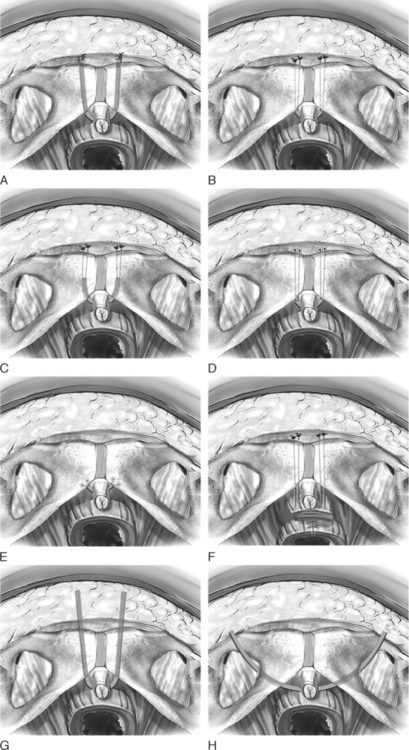
The TVT procedure was the first synthetic midurethral sling and was described by Petros and Ulmsten (1990), 1995). This ambulatory procedure was aimed at restoring the pubourethral ligament and suburethral vaginal hammock by using specially designed needles attached to a synthetic sling material. The synthetic sling material is made of polypropylene and is approximately 1 cm wide and 40 cm long. The sling material is attached to two stainless steel needles that are passed blindly from a vaginal incision made at the level of the midurethra through the retropubic space to exit at previously created stab wounds in the suprapubic area.
After this midurethral sling became well-established, techniques to surgically correct stress incontinences via a suprapubic approach were described (SPARC procedure [American Medical Systems, Minnetonka, MN]; percutaneous vaginal tape [PVT]). This involved passage of a needle from the suprapubic area to exit in a previously created incision in the vagina of the level of the midurethra. These procedures quickly became popular and were shown to be efficacious. Because they did require blind passage of the needle through the retropubic space, rare but serious complications were reported in the form of vascular and bowel injuries. These complications resulted in significant morbidity and rare cases of mortality.
Delorme (2001) reported on the first transobturator synthetic midurethral sling and described that the passage of the needle completely avoided the retropubic space and avoided any potential for serious complications in the form of vascular or bowel injuries as well as the potential for injury to the lower urinary tract. The initial description of this procedure involved the passage of specially designed needles from the obturator region, through the obturator membrane, around the ischiopubic ramus to exit in the open portion of the vagina. Shortly after the initial description, a procedure that involved passage of the needle from the vaginal incision to exit the obturator space was described.
TECHNIQUES OF SUBURETHRAL SLING PROCEDURES
Proximal Suburethral Sling and Modifications
Synthetic Retropubic Midurethral Slings
TVT
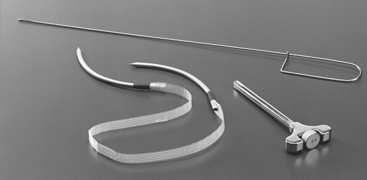
The instrumentation required for the procedure includes 30 mL of local anesthetic, such as lidocaine or Marcaine; a 22-gauge needle for infiltration; TVT kit (Fig. 16-5 [Ethicon Inc., Somerville, NJ]), which includes two 5-mm stainless steel needles connected by a 1.2-cm wide piece of polypropylene mesh; a nondisposable handle or introducer; an 18-French Foley catheter; catheter guide; and absorbable sutures to close the incisions.
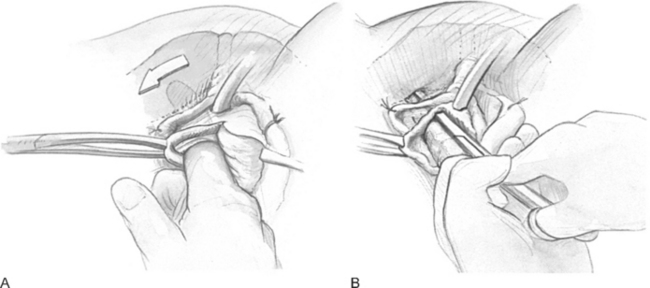
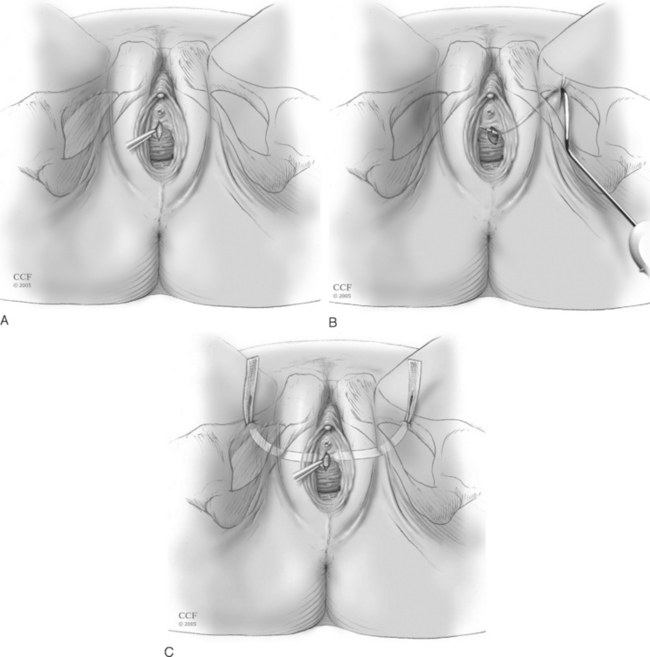
An 18-French Foley catheter should be placed and the bladder drained. A Sims or weighted speculum is placed in the vagina. Local anesthesia (8 to 10 mL) is infiltrated in the anterior vaginal wall to achieve hydrodissection and vasoconstriction. A 1.5-cm midline incision is then made at the midurethra, as shown in Figure 16-10, A. Palpating the Foley bulb at the bladder neck may be helpful to ensure that the incision is appropriately placed. With Allis clamps stabilizing the vaginal mucosa, the Metzenbaum scissors are used to dissect under the vaginal epithelium laterally to create a tunnel to the inferior pubic ramus. Unlike the bladder neck, at the midurethra the anterior vaginal wall and posterior urethra are fused and no natural plane of dissection is present. Hence, one must minimize creation of these tunnels to ensure that the tape stays in the proper position.
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree