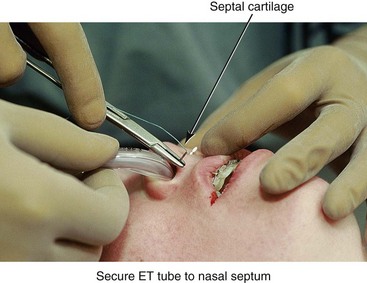
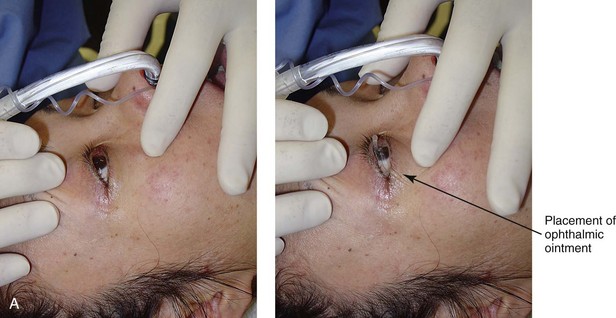
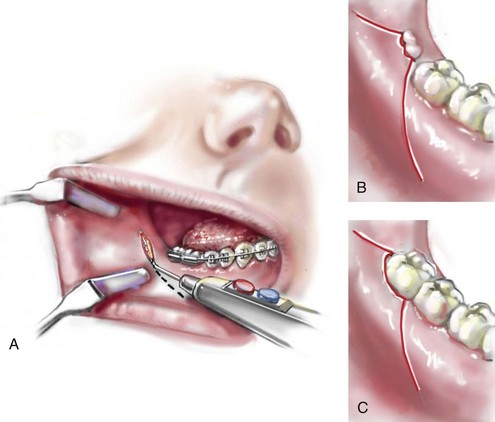
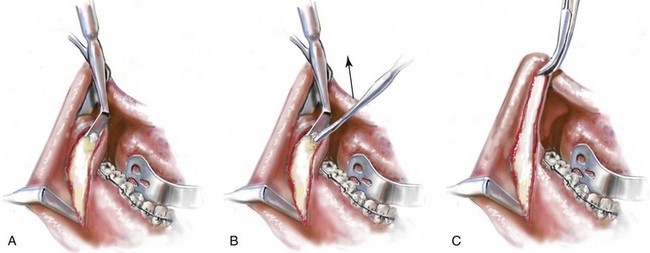
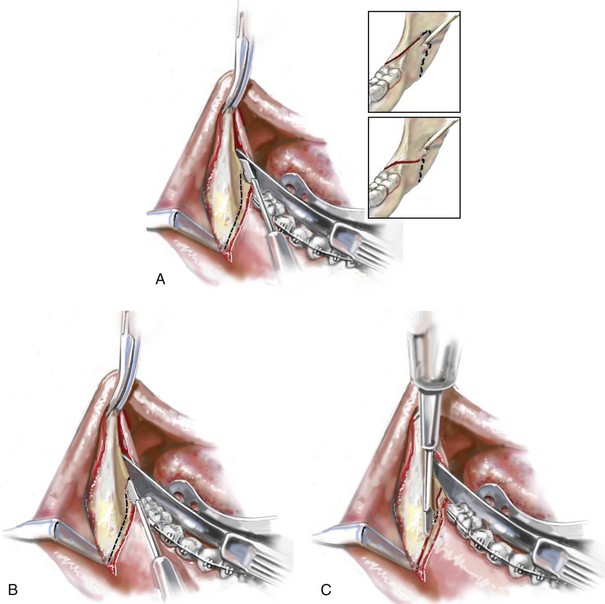
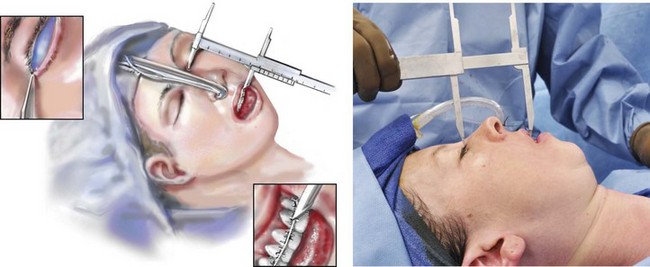
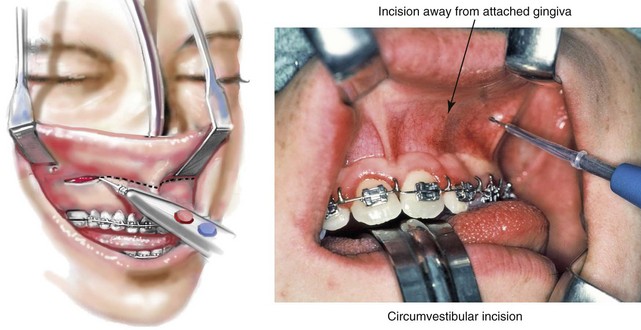
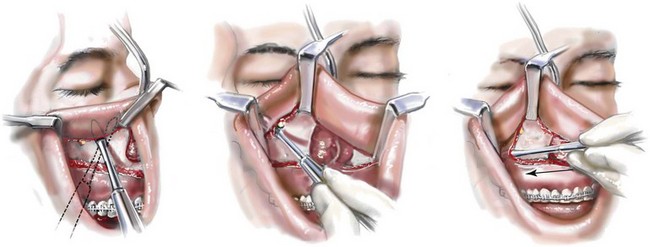
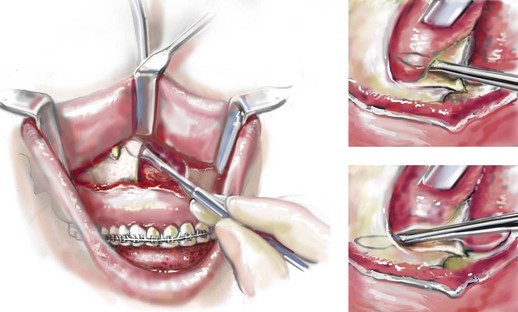
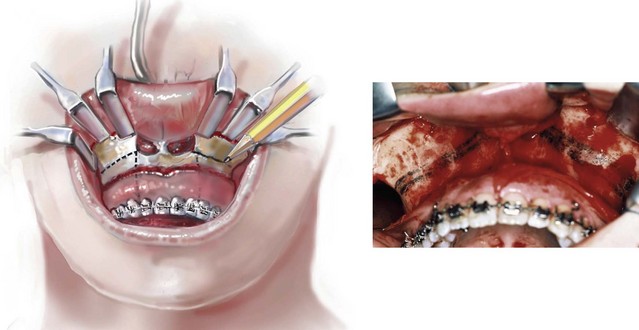
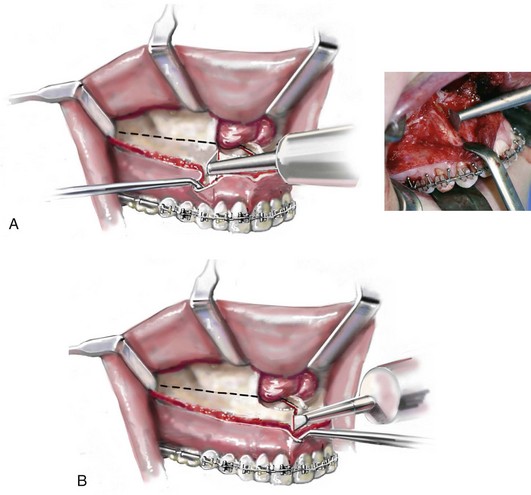
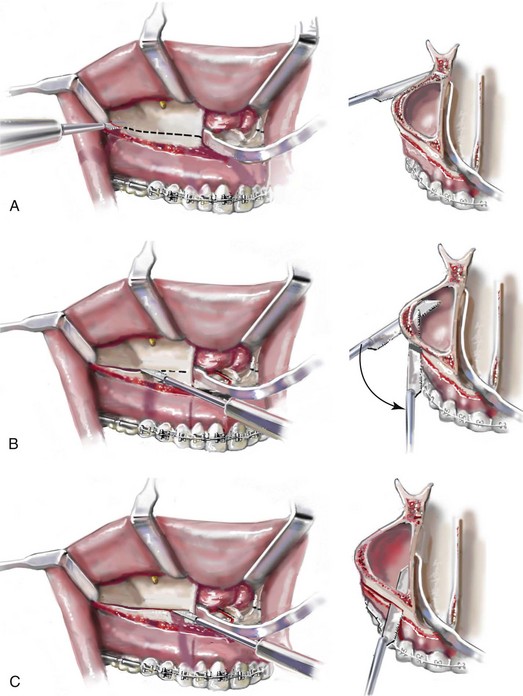
15 Maxillofacial surgeons and orthodontists are the primary clinicians who care for individuals who present with jaw deformities, malocclusions, and the associated facial dysmorphologies. When an orthognathic approach is indicated, there are a limited number of basic surgical techniques that are used to facilitate the three-dimensional repositioning of the skeletal units (i.e., the maxilla, the mandible, and the chin region) to achieve desired improvements in head and neck function and to enhance facial aesthetics. By and large, these options include the Le Fort I (Type) osteotomy, with or without segmentation of the down-fractured maxilla; sagittal split ramus osteotomies of the mandible; and an oblique osteotomy of the chin. Each of these three basic osteotomies and its associated fixation techniques has evolved gradually to its current usage (see Chapter 2).1–6 Step 1. The patient is placed supine on the operating room table with the head in a Mayfield (horseshoe) headrest in the neutral neck position. Step 2. A nasotracheal cuffed (Ring-Adair-Elwyn [RAE]) tube is inserted by the anesthesiologist and then secured by the surgeon to the cartilaginous septum with suture (#0 Ethibond). An additional suture (#0 Ethibond) is placed in the midline anterior hair-bearing scalp and then around the endotracheal tube extension over the top of the head to further secure it and to limit tension on the nose (Fig. 15-1). Step 3. Ophthalmic antibiotic ointment and protective corneal shields are placed beneath the eyelids (or temporary tarsorrhaphies are performed, if preferred) to prevent corneal injury during the operation (Fig. 15-2, A through C). Step 4. The anesthesiologist places monitoring equipment for the safe delivery of deliberate hypotensive anesthesia (i.e., arterial line, Foley catheter, large-bore venous lines, pulse oximeter, carbon dioxide monitor, and temperature probe). The bed is then positioned at approximately 15 degrees reverse Trendelenburg (see Chapter 11). Step 5. Antibiotics (e.g., Cefazolin (Ancef ); 15 to 20 mg/kg and up to 1 g) and steroids (e.g., Dexamethasone 0.5 mg/kg/dose, max: 8 mg) are administered intravenously by the anesthesiologist. Step 6. The head and neck are prepped with povidone–iodine (Betadine) solution. Avoid using soap or alcohol solutions that could irritate the cornea and the mucous membranes. Draping should provide for adequate exposure of the forehead, the eyes, the external ears, the face, and the neck. Staples are used to secure the drapes (Fig. 15-3). Step 7. The mouth and pharynx are suctioned, and a moistened gauze with a radiopaque marker is inserted as a throat pack. The teeth and dorsum of the tongue are cleansed with a sterile toothbrush (1.5% hydrogen peroxide or 0.12% chlorhexidine). The mouth is irrigated with normal saline solution and suctioned. Step 8. Steroid cream (e.g., betamethasone 0.5%) is applied to the lips to limit edema that could otherwise result from contusion during surgery. Step 9. Lidocaine solution (Xylocaine 1% with 1 : 100,000 epinephrine) is infiltrated into the lateral vestibules of the mandible, the facial vestibule of the chin, and the labial vestibules of the maxilla. Step 10. A medium rubber mouth prop is placed between the maxillary and mandibular molars on one side to maintain mouth opening. Attention is turned to the lateral vestibule of the contralateral mandible. A Incision Option One: No erupted wisdom tooth for extraction. If there is no erupted wisdom tooth to extract (i.e., if the wisdom tooth is fully impacted, absent, or erupted and is to remain in place), an incision is made with a Bovie electrocautery device or a knife (no. 15 blade) in the depth of the vestibule adjacent to the second molar (Fig. 15-4, A). The incision extends both anteriorly and posteriorly for a total length of 4 cm. The incision is carried down to bone. A sufficient cuff of mucosa is maintained adjacent to the gingiva of the molar teeth for relaxed wound closure. B and C. Incision Option Two: Erupted or partially erupted wisdom tooth for extraction. If there is a partially erupted (Fig. 15-4, B) or fully erupted (Fig. 15-4, C) wisdom tooth to be removed, the incision starts 1 cm distal and lateral to the wisdom tooth and extends to the distobuccal line angle of the tooth. The incision continues anteriorly along the cervical gingival margin of the tooth within the sulcus and then anterior and lateral into the depth of the vestibule. The incision is carried down to bone. A sufficient cuff of mucosa, including part of the papilla, is maintained adjacent to the gingiva of the second molar for relaxed wound closure. Step 12. The subperiosteal dissection exposes the anterior aspect of the lateral ramus and the posterior body of the mandible down to the inferior border (Fig. 15-5, A). The extent of the dissection anterior to the gonial angle depends on the planned buccal extension of the proximal segment. The dissection exposes the anterior superior aspect of the ramus up toward the coronoid process, with stripping of the temporalis muscle tendon (Fig. 15-5, B C). The dissection exposes the medial aspect of the ramus superior toward the sigmoid notch and inferior toward the mandibular canal (Fig. 15-6, A). (I do not dissect below the inferior alveolar neurovascular bundle or circumferentially around it, because I believe this may cause additional contusion and paresthesia.) Step 13. Retraction of the soft tissues is performed with a curved Kocher clamp on the coronoid process (superior exposure); a channel retractor superior to the neurovascular bundle (medial ramus exposure); an inferior border retractor placed anterior to the gonial angle (anterior exposure); and a tongue retractor (lingual exposure) (Fig. 15-6). Step 14. With a sterile pencil, the osteotomy lines are marked out for the sagittal splitting of the ramus of the mandible. A reciprocating saw (i.e., with a short, straight blade) completes the cortical osteotomies. A The first cut is made horizontally through the medial cortex of the ramus. This is judged to be just superior to the occlusal plane of the mandibular molars and well inferior to the region of the anterior aspect of the ramus, where the medial and lateral cortices join and no longer maintain a medullary cavity. The medial osteotomy need not extend more than 2 cm posterior (Hunsuck modification) (see insert of Fig. 15-6, A). By keeping the medial cut “low” (i.e., close to the mandibular molar occlusal surface) and “short” (i.e., only 2 cm back), the incidence of a “bad” split (i.e., with the condyle as a third segment) is greatly reduced. B The osteotomy then extends anteriorly and just lateral (buccal) to the molars. It is important that the saw blade penetrate the cortex and enter the medullary cavity in all locations. If the wisdom tooth is impacted, the saw blade will bounce off the wisdom tooth just after penetrating the superior paper-thin cortex (Fig. 15-6, B); this will be just lateral to the second molar. The blade will penetrate back into the medullary cavity as the osteotomy progresses anterior past the impacted tooth. C The reciprocating saw is then repositioned to complete the vertical cortical osteotomy. The osteotomy location will depend on the planned buccal extension of the proximal segment (i.e., the Dal Point modification.) The vertical osteotomy begins at the inferior border of the mandible, where the inferior alveolar nerve is close to the cortex and prone to laceration (Fig. 15-6, C). The osteotomy then continues superiorly to join the cortical osteotomy, which was previously completed lateral to the molars. Step 15. If the wisdom tooth is erupted and is to be removed, then the extraction is completed now or just before the cortical osteotomies; doing so before the actual split will limit a fracture of the lingual plate that may otherwise occur during dental extraction. A rotary drill with a tapered fissure bur may be used to judiciously remove bone adjacent to the tooth and to section the tooth to facilitate an atraumatic extraction. Step 16. The wound is irrigated and suctioned. The retractors are removed, and two 1 inch × 3 inch cottonoids are placed for packing (i.e., hemostasis). One is placed along the medial ramus, and the other is placed along the lateral body of the mandible. Step 17. Attention is turned to the contralateral ramus of the mandible, and identical procedures to those described in Steps 10 through 16 are carried out. Step 18. With the use of a Tessier caliper, the vertical distance (height) between the medial canthus and the mid-maxillary incisor crown is measured on the left and right sides and recorded; this generally measures between 55 mm and 70 mm (Fig. 15-7). This is a reproducible relative measure of the anterior vertical maxillary height (see Chapter 12). Step 19. Attention is turned to the vestibule of the maxilla on one side. Two medium “toed-in” retractors are used to retract the lip and cheek and thus expose the vestibule. A circumvestibular incision is initiated from the zygomatic buttress region anteriorly toward the midline (Fig. 15-8). It is useful to remain deep in the vestibule and to leave a full cuff of mucosa adjacent to the attached gingiva of the teeth. The most posterior aspect of the incision remains just anterior to and on the dental (vestibular side) of the visualized parotid duct. The incision is made with a Bovie electrocautery device or a knife (#15 blade). Once the incision is made through the mucosa the knife is directed toward the dentoalveolar region and down to bone. This will avoid injury to the infraorbital nerve and limit the exposure of the buccal fat pad. Step 20. Straight and curved elevators are used for the subperiosteal dissection of the anterior maxilla extending to and on either side of the infraorbital nerve; extending medially to expose the pyriform rim, the floor of the nose, and the anterior nasal spine; and extending posterior to the pterygomaxillary junction. A long “toed-out” retractor is placed subperiosteally in the pterygomaxillary space (Fig. 15-9). Step 21. The two medium toed-in retractors are shifted to the contralateral side of the maxilla, and the identical incision, dissection, and exposure are accomplished as described in Steps 19 and 20. Step 22. Straight and curved elevators are used to further separate the nasal mucosa from each lateral nasal wall; the anterior nasal spine from the cartilaginous septum; and the nasal mucosa from the floor of the nose (Fig. 15-10). Step 23. With four medium toed-in retractors (one on either side of the infraorbital nerve on each side of the maxilla) and two long toed-out retractors (one in each pterygomaxillary junction) in place, the anterior maxilla is fully visualized. A sterile pencil is used to mark the location for the horizontal Le Fort I osteotomy (Fig. 15-11). If significant maxillary intrusion is planned, a second parallel osteotomy line is marked out. The lower marking (i.e., the osteotomy site) is placed to be within the sinus, above the roots of the teeth, into each lateral nasal aperture, and below each zygomatic buttress. If an ostectomy is to be preformed, the upper marking is made superior and parallel to the lower marking and below the infraorbital nerves (Fig. 15-11). Step 24. If segmentation of the maxilla is to be completed, the interdental osteotomies are initiated before down-fracture. This provides a stable “workbench” for the initiation of each interdental osteotomy. The interdental osteotomies are typically made either between the lateral incisor and the canine on each side (Fig. 15-12, A) or between the central incisors (Fig. 15-12, B). The subperiosteal dissection of the gingival cuff provides adequate exposure of each interdental osteotomy location without the need for direct mucosa incisions. Each interdental osteotomy site is marked with a sterile pencil. The osteotomy is then initiated with an oscillating saw (i.e., a short fan blade on a long shaft) and later deepened after down-fracture with the oscillating saw (i.e., a longer fan blade on a long shaft). Step 25. With a reciprocating saw (i.e., a long straight blade), the Le Fort I horizontal osteotomy is completed through the lateral, anterior, and medial maxillary walls on each side (Fig. 15-13, A through C). Before the medial maxillary osteotomy is completed, the lateral nasal mucosa is protected with a small malleable retractor placed between the lateral nasal wall and the nasal mucosa. Before the lateral maxillary osteotomy is completed, the pterygoid fossa soft tissues are protected with a long, toed-out retractor. Step 26. With a specialized guarded chisel and mallet, the septum of the nose (i.e., cartilage and bone) is separated from the maxilla. Care is taken to avoid penetration past the septum into the nasopharynx (Fig. 15-14).
Sequencing of Orthognathic Procedures
Step-by-Step Approach
Description and Sequencing of Orthognathic and Other Frequent Simultaneous Procedures: Step-by-Step Approach
Preparation and Draping
Cortical Cuts for Sagittal Split Ramus Osteotomies (
![]() Video 6:2 and 7:2)
Video 6:2 and 7:2)
Maxillary (Le Fort I) Osteotomy (
![]() Video 6:3 and 7:3)
Video 6:3 and 7:3)
Segmentation of the Maxilla
Maxillary (Le Fort I) Osteotomy: Continued
![]()
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree


Sequencing of Orthognathic Procedures: Step-by-Step Approach