Septal Flaps for Nasal Lining
Jordan D. Frey
John T. Stranix
Pierre Saadeh
DEFINITION
Nasal defects are classified on the anatomical basis of the affected nasal layer: external nasal cover or skin, bony or cartilaginous nasal support, or internal nasal lining.
Replacement of nasal lining is considered the most imperative and challenging aspect in all of nasal reconstruction.1
Poor nasal lining replacement will lead to internal scarring and contracture that will compromise the aesthetic and function of native and/or reconstructed nasal cover and support.
ANATOMY
Intranasal lining transitions from the stratified squamous epithelium of the ala and columella to the mucoperichondrium of the septum and mucosa of the nasal vault.4
Laterally, internal nasal mucosa is supplied by the facial and angular arteries.
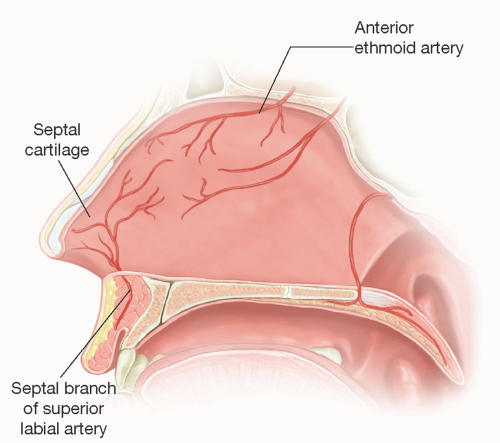
Septal mucoperichondrium is supplied by the paired septal branches of the superior labial arteries and paired anterior ethmoidal arteries5,6 (FIG 1).
The septal branches of the superior labial artery arise anteriorly through the orbicularis oris muscle lateral to the nasal spine at the base of the columella.
The anterior ethmoidal vessels arise posteriorly passing below the nasal bones to supply the dorsal septum.
A variety of septal flaps can be designed based on these vascular pedicles to replace deficient nasal lining.
PATHOGENESIS
Nasal lining defects may arise from a variety of mechanisms including traumatic, oncologic, infectious, autoimmune, iatrogenic, and drug-induced etiologies.3,4,5,7
Although oncologic resections or traumatic injury can result in more localized defects, autoimmune and infectious etiologies more often produce pan-mucosal insult.4
Nasal lining deficiencies may occur in isolation or in the context of nasal support or cover deficiencies, including fullthickness nasal defects.
Septal flaps can be utilized for primary nasal lining defects or to cover secondary defects after other intranasal flaps have been used to provide lining for the primary defect.
NATURAL HISTORY
Significant isolated nasal lining defects eventually result in scar contracture that can circumferentially destroy the midvault and nasal floor.4
This is followed by cartilage and bone necrosis leading to loss of midvault support, tip rotation, and central facial collapse toward the piriform aperture.4
Bony nasal vault collapse is prevented by the strength of the nasal bones.4
Ultimately, if external nasal skin becomes devascularized, full-thickness necrosis can occur.4
Therefore, expeditious reconstruction of nasal lining defects, before the onset of scar contracture, guided by defect etiology, is strongly favored to provide optimal aesthetic and functional results.
PATIENT HISTORY AND PHYSICAL FINDINGS
Upon initial presentation, nasal lining defect etiology must be determined.
If an etiology is not determined or residual disease is apparent, appropriate investigative biopsies, cultures, laboratory tests, or referrals should be arranged.4
It is imperative that the inciting etiology of the defect is rendered quiescent prior to any intervention, lest the ultimate reconstruction be compromised by ongoing pathology.
Possible symptoms of nasal obstruction should be elicited from the patient on history and examination because septal flaps may further compromise obstruction.
A full extra- and intranasal physical examination should largely focus on defining the location, size, and extent of the nasal lining defect as well as any defects in nasal support or cover to guide the determination of the septal flap required.
The subunit principle proposed by Burget and Menick is used to classify nasal cover defects and guide external nasal reconstruction.8
The septal mucoperichondrium and its blood supply should be examined to ensure its integrity; injury along the nasal spine or posterior septum may indicate damage to the superior labial or anterior ethmoidal vessels, respectively.
IMAGING
Traditional radiographic imaging is generally not necessary when planning for nasal lining reconstruction with septal flaps.
Meticulous and standardized preoperative patient photography is mandated for both accurate operative planning and assessment of postoperative results.
DIFFERENTIAL DIAGNOSIS
Trauma (facial fractures, foreign body)
Oncologic (basal cell carcinoma, squamous cell carcinoma, melanoma, lymphoma)
Infectious disease (syphilis, tuberculosis)
Autoimmune disease (Wegener granulomatosis)
Iatrogenic injury (septorhinoplasty, endotracheal tube pressure necrosis)
Intranasal drug abuse (cocaine)
SURGICAL MANAGEMENT
The use of septal flaps for nasal lining in any given defect is based on the size and location of the defect and the availability of septal mucoperichondrium; defect etiology and status of nasal cover and support are separate considerations.
When needed, the septum proper may be harvested as graft for nasal support; care is taken to leave an adequate L strut to prevent dorsal nasal collapse.
Preoperative Planning
Preoperatively, patient examination and photography help determine the full extent of the total nasal defect including the status of the nasal lining to develop a comprehensive operative plan.
Patients are counseled preoperatively that multiple stages are typically required for complex nasal reconstruction and that the need for minor revisions postoperatively is likely, regardless of the type of reconstruction being pursued.
Preparatory surgery includes debridement of necrotic or infected tissues and/or release of tethered scars at the time of or before definitive reconstruction.
These procedures may also take place at the time of flap delay, prelamination, or prefabrication per the reconstructive requirements.
Positioning
Patients are positioned in the supine position with the neck in slight extension to facilitate surgical access to the nose; this can be augmented with a shoulder roll.
Slight reverse Trendelenburg can help decrease venous pressure and thereby bleeding.
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree