Sensate Thoracodorsal Artery Perforator Flap
CHENG-TA LIN
LEE-WEI CHEN
EDITORIAL COMMENT
When sensibility recovery is critical (i.e., for the hands and feet), this may be the flap to go to.
INDICATIONS
The sensate thoracodorsal artery perforator flap is used when recovery of sensibility to recipient sites is required. The flap can be used for the reconstruction of hands and feet because recovery of sensibility is important to these locations. The flap is also an option for the reconstruction of breasts and phalluses.
ANATOMY
The blood supply of the flap is from the skin perforators of the thoracodorsal vessels, which run underneath the latissimus dorsi muscle. The thoracodorsal vessels bifurcate into two large branches, the transverse and descending branches. In the flap, the perforators derived from the descending branch are preferred because they are closer to the lateral intercostal
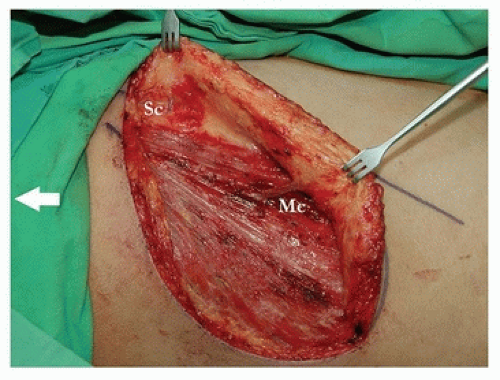
nerves and more constant than those of transverse branch (1, 2). There are two types of skin perforators from the descending branch (3). First is musculocutaneous perforator, which directly pierces the latissimus dorsi muscle. Second is septocutaneous perforator, which does not penetrate muscle. The septocutaneous perforator courses laterally between the latissimus dorsi muscle and serratus anterior muscle (Figs. 145.1 and 145.2).
nerves and more constant than those of transverse branch (1, 2). There are two types of skin perforators from the descending branch (3). First is musculocutaneous perforator, which directly pierces the latissimus dorsi muscle. Second is septocutaneous perforator, which does not penetrate muscle. The septocutaneous perforator courses laterally between the latissimus dorsi muscle and serratus anterior muscle (Figs. 145.1 and 145.2).
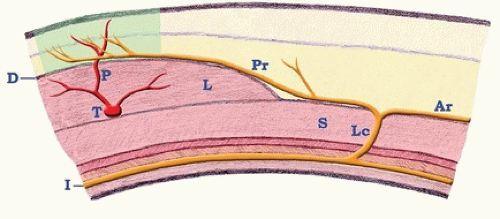
The flaps incorporate the posterior rami of lateral cutaneous branches of intercostal nerves (Figs. 145.3 and 145.4). The lateral cutaneous branch originates from the costal groove segment of the intercostal neurovascular bundle and emerges from the intercostal space. It penetrates the intercostal muscle and serratus anterior muscle and separates into an anterior and a posterior ramus. The posterior ramus courses medially, passes along the lateral border of the latissimus dorsi muscle, and disperses to the subcutaneous tissue. The main trunk of the posterior ramus always contains two or three fascicles (4).
There are two types of relationships between the intercostal nerves and the thoracodorsal artery perforators. The conjoint relationship is when a posterior ramus courses above the latissimus dorsi muscle; its main trunk or branch may travel with a thoracodorsal artery perforator and reach the subcutis together (Fig. 145.4). The separate relationship means the main trunk or branch of a posterior ramus enters the subcutis at different location from the thoracodorsal artery perforators (Fig. 145.5). The incidence of which the conjoint relationship can be found varies from 38.1% to 63.6% (4, 5).
FLAP DESIGN AND DIMENSIONS
Before flap harvest, we prefer using color Doppler sonography to map the locations of thoracodorsal artery perforators and intercostal artery perforators (Fig. 145.1). The location of an intercostal artery perforator helps to identify the approximate course of an intercostal nerve because of their concomitant relationship (Figs. 145.5 and 145.6). There are four reasons that oblique or transverse designs of flap orientation are preferred than vertical designs. First is the horizontal distribution of the dermatomes of intercostal nerves. Second is the prevention of breast distortion caused by the tension line of skin closure. Third is the more acceptable transverse donor site scar (5, 6). Fourth is the oblique-transverse axis of the perforasome of the thoracodorsal artery perforators (7, 8).
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree