Segmental Maxillary Osteotomy
Philip Kuo-Ting Chen, Eric J.W. Liou, Yu-Ray Chen
KEY POINTS
○ Segmental maxillary osteotomy is used to correct relative malposition within the maxilla.
○ Understanding development of late mixed dentition to skeletal maturity is important in planning segmental maxillary osteotomy.
○ Preoperative preparation depends on the type of approach selected (orthodontic first versus surgery first).
○ The different segments are repositioned through direct repositioning or distraction osteogenesis.
○ Rapid orthodontic tooth movement can be used to align the teeth, relieve dental crowding, and prevent relapse.
Even with the well-established multidisciplinary treatment approach, most patients with clefts continue to develop skeletal problems, such as discrepancy between the dental arches, maxillary hypoplasia, mandibular prognathism, inappropriate facial proportions, and wide alveolar gaps with complex alveolar oronasal fistulas. These concerns may result in functional and aesthetic problems such as malocclusion, poor dental hygiene, foul smell from food impaction, nasal inflammation from nasal regurgitation, and nasal deformity from an unbalanced skeleton.1–9 Such problems can be addressed through orthognathic surgery (OGS) after the patient has reached skeletal maturity.10,11 The current approach for treating the cleft skeletal deformity is typically a one-piece maxillary advancement that may be combined with a mandibular setback or leveling, depending on the mandibular position and canting of the occlusal plane. Orthognathic surgery, combined with orthodontic treatment, results in improvement in the position of the maxillary and mandibular bones, change of the facial proportions, and alignment of the dental arches.
Despite the known benefits of OGS, the procedure is not considered until a patient reaches skeletal maturity. Because a hypoplastic maxilla can be identified at an early age in patients with a cleft, the technique of maxillary distraction osteogenesis provides an opportunity for early intervention, serving as a solution to the primary and secondary problems related to the cleft skeletal deformity.12–16 Most of the maxillary distraction osteogenesis techniques described involve a LeFort I–type maxillary osteotomy and pterygomaxillary disjunction. In the standard approach, the maxilla is advanced in one piece, and new bone forms at the osteotomy sites along the maxillary sinus walls and pterygomaxillary junction. Three drawbacks of this technique are (1) the maxillary bone itself remains unchanged from its previous shape and size, with no sagittal lengthening of the alveolar process; (2) dental crowding is difficult to relieve, because it is difficult for an orthodontist to move the molar teeth posteriorly into the regenerated bone in the pterygomaxillary region; and (3) deterioration of velopharyngeal port closure is possible when the maxilla is advanced significantly.
SEGMENTAL MAXILLARY OSTEOTOMY AND INTERDENTAL DISTRACTION OSTEOGENESIS
The purpose of a segmental maxillary osteotomy in a cleft orthognathic procedure is to correct relative malposition within the maxilla. A common deformity that cannot be solved by standard cleft OGS is a severely hypoplastic maxilla with dental crowding. The one-piece LeFort I maxillary osteotomy can only change the position of the entire maxilla in six directions: sagittal, vertical, and transverse directions plus the pitch, roll, and yaw. Because OGS does not change the length of the bone or relative tooth position within the bone, it cannot solve the problem of significant malocclusion from dental crowding.
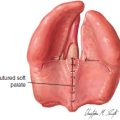
Combining the techniques of multiple-segment osteotomies with rapid orthodontic tooth movement addresses several of these drawbacks. The technique of maxillary interdental distraction osteogenesis was developed in late 1990s.17 The maxilla or dental arch is lengthened through the formation of a new bony segment within the maxilla, between teeth, rather than along the maxillary sinus walls or pterygomaxillary region. This technique can expand the maxillary body and lengthen the alveolus together with the attached gingiva in an anteroposterior dimension, allowing the orthodontist to relieve dental crowding. Through rapid orthodontic tooth movement, dental crowding is quickly resolved as the malaligned teeth are rapidly moved into the regenerate bone. Once these teeth are aligned and occupying the regenerate bone, the risk of relapse is reduced. Theoretically, this approach should not affect the patient’s speech, because the posterior segment remains unmoved; this should eliminate the need for speech therapy or velopharyngeal port management that has sometimes resulted from traditional single segment distraction. Gingivoperiosteoplasty, performed as a second-stage operation (around 2 weeks after narrowing the dental gap), and usually followed by further approximation of the segments (compression osteogenesis of the alveolar cleft), may then achieve bony union across the cleft and thus eliminate a bone grafting procedure (Fig. 73-1).
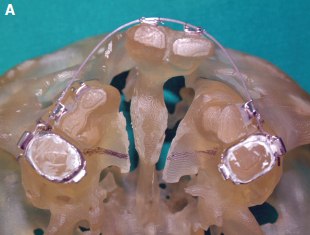
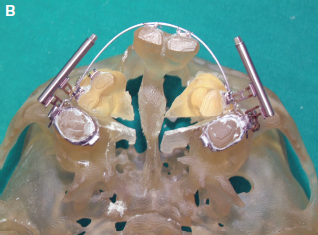
Fig. 73-1 A, An acrylic model of bilateral cleft lip and palate with hypoplasia of both lateral segments and a wide alveolar gap and difficult oronasal fistulas. The lines on the palatal shelf show the line of segmental osteotomy across the palatal shelf. B, After segmental maxillary osteotomy and interdental distraction osteogenesis with the bone-borne distractors, both anterior maxillary segments are moved forward. The alveolar gaps are approximated to facilitate surgical closure. The gaps in the osteotomy sites will be filled with new regenerate bone. The bony movement is controlled by the heavy arch wires. However, the vector of the distractors can further adjust the direction of bony movement (forward movement or convergence).
Background and Reconstructive Principles
This technique combines two of our previously published techniques, multiple segment osteotomies and rapid orthodontic tooth movement.18–22
Multiple-Segment Osteotomies
Multiple-segment osteotomies enable the surgeon to perform fine osteotomies between the teeth safely, either with or without presurgical orthodontic separation of the teeth at the osteotomy site. However, the previous technique was applied in OGS performed after skeletal maturity. The presently described technique is used for the early intervention of cleft skeletal problems at the time of late mixed or early permanent dentition. Some modifications have been made to prevent injury to the tooth roots or developing dental follicles in the alveolar process.
Rapid Orthodontic Tooth Movement
The teeth adjacent to the regenerate bone can be moved orthodontically into the regenerate bone at a faster rate, soon after the distraction process, because the regenerate bone is still soft. Furthermore, this may have a significant influence on the stability and long-term structural preservation of the bone created by distraction osteogenesis within the tooth-bearing segment of the maxilla.
Patient Selection and Evaluation
The technique is best used in patients with a wide alveolar cleft, a difficult anterior palatal oronasal fistula, or a short maxillary segment with dental crowding. It can be used for anterior maxillary advancement. However, if an intraoral device is used, the amount of advancement is limited by the length of the activating screw.
Management Algorithm
The preoperative orthodontic approach includes tooth alignment, selective palatal expansion with a modified quadhelix, and opening a 2 mm space between the teeth at the distraction site to facilitate the interdental osteotomy. The maxillary dentition must be well aligned preoperatively so that a stainless steel arch wire (0.016 by 0.022 or thicker) can be placed. The arch wire also serves as a track that helps guide the osteotomized anterior segments to be distracted in a curved and convergent pathway. The preoperative orthodontic management usually takes 6 to 8 months.
The length of hospital stay after surgery may be as short as 3 nights. The latency period is 5 to 7 days. The distraction rate and rhythm are 1 to 2 mm per day. The anterior segment of the maxilla can be moved to the desired position within 2 to 3 weeks. During interdental distraction, the movement vector of the distracted segment can be adjusted in orthodontic outpatient clinics.
When the surgery is performed for wide alveolar clefts or difficult oronasal fistulas, a gingivoperiosteoplasty is performed when the bony segments are approximated. The buccal gingival and palatal mucoperiosteum are raised minimally and the cleft margins are freshened and closed without tension. The distraction is continued after the gingivoperiosteoplasty until the alveolar segments are in firm contact with each other (compression osteogenesis of the alveolar cleft).
After completion of distraction, the bone-borne distractor remains in place for an additional 3 months of consolidation and maintenance of position. Rapid orthodontic tooth movement is commenced during this period, usually 1 to 2 weeks after completion of the distraction. The tooth (or teeth) to be moved depend on the individual clinical situation of dental crowding. Using the bone-borne distraction device as the anchorage, an orthodontic elastic chain or nickel titanium coil spring is attached between the distractor and the teeth to be moved into the regenerate bone. Patients are evaluated on a monthly schedule until the entire edentulous space has been eliminated. This typically takes 3 to 5 months.
Surgical Technique
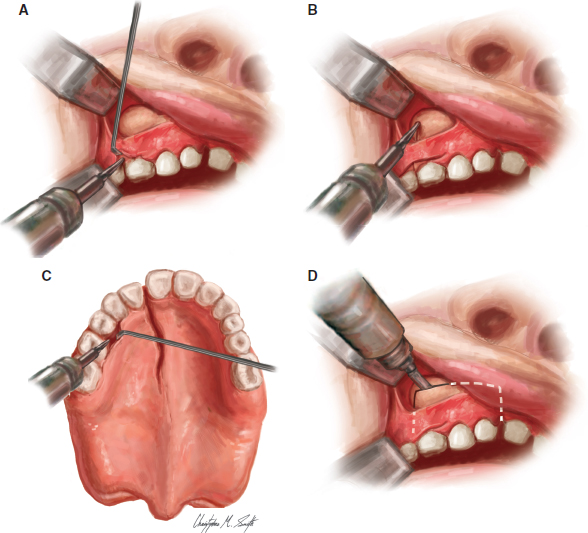
The surgical procedure consists of two components, (1) a horizontal osteotomy, usually at the LeFort I level, and (2) a vertical interdental osteotomy, usually located between the second premolar and the first molar. The posterior segment remains in its original position, and the anterior segments are mobilized and distracted anteriorly to converge. The procedure is performed under general anesthesia with nasotracheal intubation. A horizontal intraoral incision is made along the buccal vestibule of the maxilla. Superior mucoperiosteal flaps are raised, exposing the site for the horizontal maxillary osteotomy on the buccal side. A vertical subgingival tunnel extending superiorly from the interdental attached gingiva to the horizontal incision is made, thus exposing the site of the vertical interdental osteotomy on the buccal side of the anterolateral maxillary wall. A second narrow and parallel tunnel is made on the palatal side of the maxilla without stripping all of the palatal mucosa, which would devascularize the segment. Preoperative radiographs are used to estimate the anatomic position of the dental roots and the location of permanent tooth buds and to plan the sites for interdental and horizontal maxillary osteotomies. These positions are marked on the alveolar bone with surgical marking pencils. The vertical interdental osteotomy is started inferiorly in the subgingival tunnel with corticotomy using a 1 mm round bur (Fig. 73-2, A). The corticotomy line is extended upward and then deepened to become a complete osteotomy on the anterior maxillary wall (Fig. 73-2, B). This is followed by a similar procedure on the palatal shelf through the palatal tunnel (Fig. 73-2, C). The corticotomy on the palatal shelf is performed using the haptic feedback of sensing the burr penetrate through the cortical bone. A complete horizontal osteotomy is performed with a reciprocating saw through the anterior maxillary sinus wall, 3 to 5 mm superior to the dental root apex and tooth buds (Fig. 73-2, D). Next, a 4 mm wide, thin-blade osteotome is used from the vertical osteotomy line on the anterior maxillary sinus wall, passing medially through the medial maxillary sinus wall, to complete the cuts in the coronal plane (Fig. 73-2, E). This thin-blade osteotome is also used to complete the cuts on the palatal shelf and the nasal floor, with careful protection of the nasal mucosa and the nasotracheal tube (Fig. 73-2, F). The nasal septum is cut with a guarded septal osteotome. The last step, which is the most difficult part of the procedure, is the osteotomy of the teeth-bearing alveolar process. A thin-blade osteotome is passed between the teeth, and a green-stick fracture of the alveolar process is created through gentle twisting of the osteotome back and forth (Fig. 73-2, G). This prevents direct impact of the osteotome on the tooth root or tooth buds within the alveolar process. After the horizontal maxillary and interdental osteotomies are performed, the distal segment of the osteotomized dental arch should be completely mobile. The bone-borne distraction devices are mounted on the anterior maxillary sinus wall, across the interdental osteotomies on both sides of the maxilla; this stabilizes the distal segments to the proximal segment of the maxillary dental arch (Fig. 73-2, H). This step can be eliminated if a tooth-borne device is used. A test turn must be performed to check for any hindrance of the bony movement during distraction. The incisions are irrigated and closed with absorbable sutures. The attached gingiva on the buccal and palatal sides of the interdental osteotomy sites must be sutured together to prevent any bony exposure of these regions during the distraction process.