Secondary Superficial Temporal Artery-Neck Flap for Orbital Reconstruction
H. P. LABANDTER
B. GUYURON
EDITORIAL COMMENT
Eye socket reconstruction using skin or mucosal grafts and flaps has been notoriously difficult because of scarring, contracture, and donor deformities (1, 2). The ideal reconstruction should be done with hairless tissue, cause minimal donor-site deformity, and provide sufficient tissue for adequate prosthetic reconstitution.
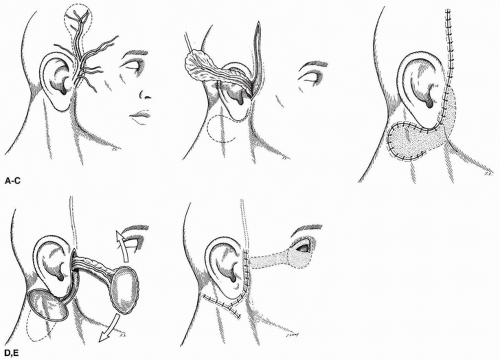
Experimental work has demonstrated the possibility of vascularizing tissue such as skin flaps and even composite flaps by the introduction of known axial vessels using omentum (3, 4). Experimental and clinical work has shown that a random-pattern flap can be converted into a “secondary” axial-pattern skin flap on a known vascular supply (5). The superficial temporal artery can be placed beneath the hairless skin below the ear. Once vascular connections have been established, the flap can be transferred to cover various areas of the face within the arc of flap rotation.
INDICATIONS
Advantages of the procedure not only include the use of a known axial-pattern flap of hairless skin, but there is also no flap contracture, donor-site deformity is minimal, and a deep reliable sulcus for prosthetic placement can be established.
ANATOMY
The area to be used as lining for the eye socket is situated below and posterior to the tragus of the ear and is a patch of hairless skin. A site is selected where the donor area scars can be hidden, if possible, by hairstyling. In the adult male, the area of skin is limited to the space between the beard and the hairline, approximately 3.5 × 4 cm in width. Vertically, the distance can be extended as needed.
The superficial temporal artery, which is a terminal branch of the external carotid, begins in the parotid gland behind the neck of the mandible and crosses over the posterior root of the zygomatic arch. About 5 cm above the arch, it divides into an anterior and posterior branch. The frontal anterior branch runs upward and forward in a tortuous fashion, supplying muscle, skin, and pericranium in that area. The posterior parietal branch is larger than the anterior branch, curving upward and backward on the side of the head, lying superficial to the temporal fascia, and anastomosing with the opposite artery and the posterior auricular and occipital arteries. Variations in the superficial temporal arteries include differences in the relative sizes of the frontal and parietal branches. Either of these may be absent. The maximum length of the posterior parietal branch will be used as “donor” vessels for this flap.
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree