To properly treat a patient with a secondary cleft lip or palate deformity, one must make an accurate diagnosis of the underlying problem. Recognition of specific recurring patterns and common deformities will help facilitate the surgical planning process and assist the surgeon during future procedures. Through a combination of accurate analysis, clinical patience, and technical precision, successful correction of secondary cleft lip and palate deformities can be delivered.
Key points
- •
Secondary deformities of unilateral cleft lip repair present a unique set of challenges to the cleft surgeon.
- •
Some deformities are amenable to correction, whereas some may be difficult to address and reverse completely.
- •
In general, if more than one conspicuous deformity is present, it is best to consider performing a full lip revision by complete takedown of the previous repair and rerepair.
- •
A cleft surgeon who performs a large number of lip revisions learns first-hand the critical value of a well-executed, meticulous primary cleft lip repair.
- •
Historically, there has always been some level of acceptance for revisionary surgery of the lip and nose. In the current era, the need for major revision is generally avoidable and should be viewed with greater scrutiny.
Introduction
Secondary cleft deformities are common and require thorough workup and evaluation by the treating cleft surgeon. Timing and sequence of surgical correction of secondary deformities are contingent on the type and severity of the problem. Cleft lip revision is typically performed before a child enters a social setting where stigmatization and/or isolation from peers may take place. By contrast, closure of oronasal fistulae is undertaken whenever the fistula is deemed “symptomatic,” manifested as speech dysfunction or oronasal reflux. This article reviews surgical strategies to address secondary deformities following unilateral and bilateral cleft lip repair, as well as management of oronasal fistulae following cleft palate repair.
Secondary Cleft Lip Deformities Following a Unilateral Cleft Lip Repair
On initial evaluation of a patient who presents with persistent or iatrogenic stigmata of cleft following repair of a unilateral cleft lip deformity, it is necessary to deduce the type of repair that was initially performed. Each different repair type can be associated with specific, consistent, potential problems, the patterns of which can be addressed with a reliable corrective action. Close inspection of the patient’s lip repair will provide a good sense of the type of previous repair. It is helpful to review previous operative reports and to discuss the circumstances of initial cleft lip repair. Questions regarding any complications following the initial repair (infection, dehiscence, suture reaction); what type of suture material was used; whether post-operative nasal stents were used; and whether primary rhinoplasty was performed may all help to identify contributing factors that can then help guide subsequent decisions.
Patients can present at any age for evaluation of a prior cleft lip repair. In some cases, the parents may seek additional opinion to correct residual deformity; in other cases, families may be establishing team care following a move or adoption. In the former setting, the surgeon’s opinion is specifically sought to answer the question as to whether additional surgery has a likelihood of improving on the result. In the latter, the family may not specifically be dissatisfied with the result; therefore, the surgeon must carefully bring the matter to discussion if he/she feels that revision would provide significant benefit now or in the future. Cleft lip revision is most typically entertained before a child enters school or earlier if persistent deformity is highly disfiguring. Although the goal of primary surgery is to avoid the need for revision, parents should be counseled early that lip revision may be beneficial before starting first grade.
Common deformities that are seen following a unilateral cleft lip repair include:
- •
Vermilion discontinuity with medial notching
- •
Poor cutaneous roll continuity or obliteration of cutaneous roll by prominent scar
- •
Vertically short (more common) or a vertically long cleft-side (lateral) lip element
- •
Wide and prominent cutaneous scar
- •
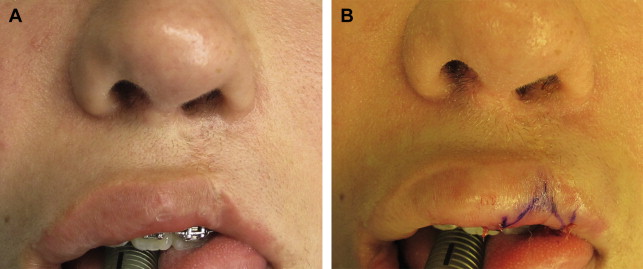
Conspicuous transverse hatch marks from sutures that were tied too tightly or left in place too long ( Fig. 1 )

Fig. 1
Distinct unilateral deformities. Note the asymmetric vertically short lateral lip, cutaneous roll discontinuity, vermilion asymmetry, and prominent suture hatch-marks. In addition, the cleft-side alar base position is inferiorly displaced and the nostrils asymmetric.
Associated nasal deformity, resulting from either incomplete correction at time of primary cleft lip repair or from overzealous primary rhinoplasty, may also include:
- •
Alar base malposition
- •
Nostril asymmetry
- •
Effacement of nostril sill
- •
Micronostril deformity
- •
Persistent, uncorrected deviation of caudal septum to the noncleft side
- •
Excessive scarring (see Fig. 1 )
In rare instances, especially with an improperly executed primary rotation-advancement lip repair, one can observe a complete shift of the Cupid’s bow to the cleft side with a high point of noncleft Cupid’s bow peak found in the midline. This finding may also be observed in patients who have had multiple previous revisions with vertical scar excision and rerepair in whom normal Cupid’s bow and philtrum landmarks have been virtually obliterated.
Failure to completely release and approximate orbicularis oris can also result in common deformities. Abnormal upper lip animation may be evident if continuity of the orbicularis oris muscle was not achieved. Asymmetric fullness (muscle bulge) on the superior aspect of the cleft-side upper lip subjacent to subalare may reflect inadequate initial dissection between the muscle and the overlying skin envelope. Problems related to muscle discontinuity most often require takedown, rerelease, and rerepair of skin and muscle, even when the skin repair itself is nonproblematic. This underscores the need for proper muscle alignment and repair at the initial surgery because it reintroduces the risk of cutaneous scarring, which is greater among older children than it was during infancy.
Surgical correction of secondary cleft lip deformities following unilateral cleft lip repair
The approach to surgical correction depends on the degree and severity of the presenting deformity. In general, if sufficient residual lip tissue is present and more than one deformity (problem) is present, the authors recommend complete takedown of previous repair and rerepair via either a rotation-advancement (Millard) cleft lip repair (LM) or a conversion to a Fisher repair (DK, EB). More minor or isolated problems may be amenable to simpler approaches: fat graft augmentation of medial (central) vermilion deficiency ( Fig. 2 ); an asymmetric Z-plasty at vermilion-mucosal junction ( Fig. 3 ); transverse wedge excision at the vermilion-cutaneous junction for lateral lip element vermilion fullness; deepening of the upper sulcus; or simple linear scar excision and closure. Secondary nasal deformities should also be addressed; these are covered in detail in the article “Correction of the Cleft Nasal Deformity: From Infancy to Maturity” by Mark D. Fisher, David M. Fisher, and Jeffrey R. Marcus elsewhere in this issue of the Clinics.
Challenging Deformities
Some deformities are extremely difficult, if not impossible, to correct. One example is an excessively wide cutaneous scar, particularly in the setting of a deficiency in transverse lip length. In this setting, complete excision of the scar would further tighten the upper lip and negatively affect animation.
Another example is a concentration of scar tissue at the lip-columella junction following an improperly inset C-flap in a rotation-advancement repair. In such cases, the extent of scarring present may preclude complete excision, as it would yield a significant soft tissue deficiency vertically. Revisionary surgery is elective, and as such, one must judge the likelihood and potential extent of improvement to help the family build appropriate expectations as they make a decision whether to have their child undergo another surgical procedure (and anesthetic). The discussion should include timing of the procedure and consideration of future or concurrent needs.
When revising a wide or prominent vertical cutaneous scar from previous repair, it is key to recognize that subsequent straight-line closure may asymmetrically lengthen the upper lip on the cleft side. A concomitant single or double wedge excision either just above the cutaneous roll and/or immediately medial to subalare may be required to balance out the lip height. These wedge excisions have a transverse orientation with their base medially. Alternatively, the vertical scar excision may be extended bidirectionally into the nasal sill or caudally past the vermilion-mucosal junction as a “dog-ear” where the excess length may be camouflaged intranasally or corrected via a transverse wedge excision, respectively. A vertically short lip may benefit from length augmentation with an appropriately sized lateral cutaneous triangle immediately above the white roll that is inset into a back-cut on the medial lip element, as a form of an asymmetric Z-plasty. Reducing scar burden and proper reorientation and realignment of key landmarks may make the residual, now narrowed scar, appear more camouflaged.
Secondary Cleft Lip Deformities Following a Bilateral Cleft Lip Repair
Some inherent characteristics in the secondary bilateral cleft lip and nose deformity must be taken into consideration. These include paucity of tissue of the central lip, an inadequate or diminutive columella, and a limited blood supply to the prolabium. Each of these affects treatment management and outcomes.
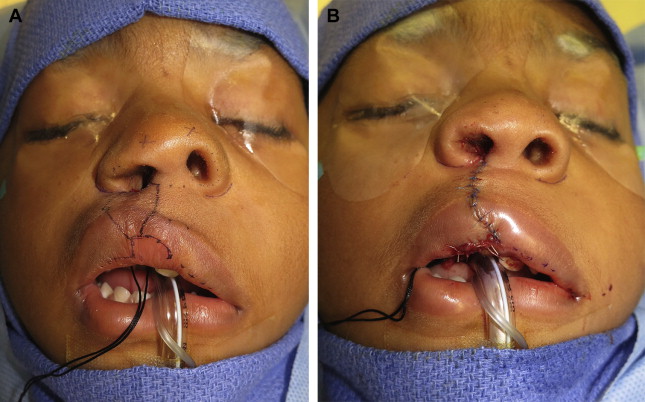
“Whistle” Deformity
The most common secondary deformity seen in the vermilion of the bilateral cleft lip is a relative deficiency. The deformity can be caused by both the lack of normal musculature and mucosa in all dimensions, as well as an inappropriate primary repair. Some state that this “whistle deformity” can be adequately corrected by reapproximation of the orbicularis oris muscle. In mild cases, various local tissue rearrangements may compensate or camouflage the central vermilion deficiency. Fat augmentation can also be used for correction of mild to moderate central vermilion deficiency. These grafts can be injected micrografts or full-thickness dermal fat grafts. For more substantial defects, the main issue is usually an inadequate primary repair, and the vermilion deficiency will be accompanied by a widened philtrum, deficient columella, and widened nasal base ( Fig. 4 ). The proper correction will involve a complete takedown and rerepair. The approach to correcting central vermilion deficiency is thus predicated on the extent of the deformity. For the severe whistle deformity or transversely deficient (tight) lip an Abbe flap may be required. This approach is particularly helpful when local measures of tissue rearrangement have been exhausted. It is the only available procedure that can reconstruct a natural-looking philtrum, Cupid’s bow, and central tubercle while augmenting the transverse dimension, thereby alleviating tightness. When designing the flap dimensions, emphasis should be placed on reconstructing the entire philtral unit, which will release the abnormal tightness and provide a balanced profile. It is also advisable to harvest the flap from the center of the lower lip and place it in the aesthetic center of the upper lip. This facilitates the appearance of a central vermilion tubercle and cupid’s bow. It should be designed slightly smaller than the intended neophiltrum; this facilitates closure of the lower lip donor site and allows for stretching of the flap once in position. Finally, the authors recommend dividing the flap on post-operative day 10 to day 14. To assure viability, one can compress the native labial artery pedicle and check capillary refill of the inset flap.
The Manchester repair, which is now used by far fewer surgeons, merits specific mention. In the Manchester repair, central vermilion is retained from the prolabial segment with the prolabial shield, rather than being derived from the lateral lip elements and meeting in the midline. The vermilion height of the prolabial segment is significantly different than that of the lateral elements and therefore is consistently conspicuous as a mismatch with unsightly, dry and flaky vermilion from the original prolabium. When the patient has had this type of initial repair, there will likely also be orbicularis oris discontinuity, an absence of white roll within Cupid’s bow, and a shallow sulcus. The only option in this setting is to perform a total lip revision according to more contemporary methods (refer to article on “Modern Tenets for Repair of Bilateral Cleft Lip” elsewhere in this issue by Alexander C. Allori and Jeffrey R. Marcus). Total revision involves removal of the abnormal vermilion from the prolabium, replacement with the fuller, muscle-containing vermilion of the lateral lip elements, and deepening of the sulcus by bringing lateral mucosa to the midline.
Excessive Scarring
Often, the most noticeable and striking stigmata of a repaired bilateral cleft lip is an unsightly scar. A poor scar is one that even after 18 months remains hyperpigmented, raised, or foreshortened. Contributing factors at the time of cleft repair include inadequate orbicularis oris muscle release and repair, a protruding premaxilla, and excessive cleft width. All these conditions result in a tight lip closure. This leads to tension and subsequent widening of the lip scar over time. Permanent sutures used at the time of primary repair, taken with excessively wide bites and left in for more than a few days, will result in a scar with cross-hatching as well. Although some feel that the cutaneous lip should never be reopened for revision, the authors advocate full-thickness scar excision, from the prolabial side of the repair, and muscle reapproximation if continuity is lacking. An adequate muscle repair is the basis for successful, permanent correction of widened and prominent scars.
Goals of Reconstruction
The goal of primarily reconstructing the orbicularis oris sphincter and obtaining lip muscle continuity cannot be overemphasized. The literature is replete with examples documenting its importance. With regard to the soft tissues, a discontinuous orbicularis oris has been implicated in widened lip scars, wide and convex philtra, and whistle deformities. Furthermore, failure to fully dissect, release, reorient, and unite the muscle fibers from the alar bases will contribute to persistent bulging of the discontinuous lateral lip musculature with attempted animation. If evaluation reveals functional abnormality of the orbicularis oris and a telltale “muscle bulge” on animation, it should be released from all of its abnormal attachments and repaired.
The philtrum truly is the keystone of the upper lip. In the bilateral cleft lip, the philtrum has a tendency to become progressively wide and convex in shape over time. The action of the orbicularis oris, combined with the persistent presence of tension from the primary repair, leads to a horizontal widening of the prolabial soft tissue and further loss of convexity of an already abnormal philtrum. Excision of the excess philtral tissue, with reapproximation of the orbicularis to the newly redesigned philtrum, is the surgical optimum. When considering the subtleties of the philtral subunit, one must include Cupid’s bow. Although there is a tremendous anatomic variety in individuals, the presence of a Cupid’s bow is an essential feature of a “normal-appearing” upper lip. The bilateral cleft lip often has a shallow or absent buccal sulcus and a tethering of the upper lip to the anterior aspect of the alveolus. An adequate sulcus, although often underemphasized, is essential for cleft lip reconstruction, and it can be created by adequate elevation of the prolabium from the premaxilla during primary repair and coverage of the resultant raw premaxilla with an inferiorly based mucosal flap. The creation of an adequate sulcus and normal anatomy enhances proper lip function and facilitates appropriate fitting of orthodontic appliances. Several surgical techniques have been described for the treatment of the shallow buccal sulcus and fall primarily into 2 categories: mucosal grafts and local flaps. Although mucosal grafts are not ideal and have been associated with contraction, readhesion, and sulcus obliteration, these complications can be minimized with the use of a dental amalgam stents.
Palatal Fistulas
For all cleft surgeons, palatal fistulas remain a considerable challenge whether they are encountered in the authors’ own patients, as referrals from other surgeons, or on mission trips. Many small, early post-operative fistulas can be managed conservatively. They may eventually close without intervention. Fistulas may be clinically significant when they lead to nasal air escape, speech distortion, or regurgitation of liquids and solids. Larger fistulas may also lead to velopharyngeal insufficiency, thereby complicating speech management.
The published rate of post-operative fistulas varies widely, from 0% to 70%. This in part is because of the lack of a standard classification scheme, which hinders both communication and research efforts. At the authors’ institution, the authors use the Pittsburgh Fistula Classification System, described by Losee and colleagues, due to its ease of use. The Pittsburgh Fistula Classification System includes 7 fistula types: those at the uvula or bifid uvulae (type I); in the soft palate (type II); at the junction of the soft and hard palates (type III); within the hard palate (type IV); at the incisive foramen or junction of the primary and secondary palates (type V; this designation is reserved for use with Veau type IV clefts); lingual-alveolar (type VI); and labial-alveolar (type VII). Fistulas are then further classified into functional or nonfunctional depending on their impact on speech and the presence of nasal regurgitation.
Fistulas are difficult to repair definitively; the recurrence rate after repair reportedly approaches 65%. Many strategies to repair and decrease the incidence of post-operative palatal fistulas have been reported over the years that have ascended the reconstructive ladder. From direct cauterization by Obermeyer in 1967, to an appliance/obturator by Berkman, to the myriad of local flap designs by von Langenbeck to Gabka in 1964, and to free conchal grafts by Ohsumi and colleagues, the options put forth for closure of palatal fistulas have been numerous. Guerrero-Santos and Altamirano popularized the tongue flap in the 1960s and 1970s, which has remained a mainstay at some centers for closure of larger anterior fistulas. Multiple pedicle flaps, including the facial artery myomucosal flap, have been described to treat those most difficult large anterior fistulas as well. Even free tissue transfer has been described for when all other modalities have been exhausted. As with many situations in plastic surgery, when there are numerous procedures described, it is often because no one option works reliably in all cases. The most recent innovations in fistula treatment have been the use of acellular dermal matrix as described by Kirschner and colleagues and the use of the buccal fat pad flap.
In general, the larger the fistula, the larger the surgery required to address it. Small local flaps have the inherent problem of using already scarred, stiff tissue that is often friable and difficult to work with due to the constant exposure of regurgitating nasal and oral contents. The well-described procedures such as the FAMM flap and tongue flap have the benefit of bringing in vascularized, unscarred tissue, but at the expense of considerable donor site morbidity, technical difficulty, considerable postoperative care, and need for a second surgery.
The preferred method at the authors’ institution for fistulas of the soft palate only is a direct excision and repair, often in conjunction with a conversion Furlow palatoplasty if the fistula occurs in the presence of velopharyngeal insufficiency.
Fistulas of the hard palate, including those at the junction of the hard and soft palate, require considerably more than direct excision and closure due to their nature and paucity of malleable local tissue. The local transposition flaps described in various textbooks are often inadequate for complete closure, as the arc of rotation often falls short. In the authors’ experience, it is the rare hard palate fistula that does not require complete re-elevation of either unipedicled or bipedicled flaps for adequate oral mucosal closure.
Nasal lining closure is often the more difficult of the 2 layers to achieve watertight repair for. This is because of the inherent friability of the tissues that have been exposed to constant reflux of fluids through the fistula. If local nasal tissue proves to be inadequate, palatally based hinge flaps or nasal septal flaps may be used. Another option, based on the work of Kirschner and colleagues, is the use of acellular dermal matrix as an adjunct when local soft tissue options prove inadequate for a watertight closure. They advocate for use of a thin piece of acellular dermal matrix for augmentation of nasal closure and have data to support its use in all fistula types, except those of the soft palate only, with a recurrent fistulas rate of 3.6%.
Another option, when local tissue is insufficient for closure of either the nasal or the oral lining, is use of the buccal fat pad flap. This flap has been widely described for closure of palatal defects both in the head and neck literature and in the cleft palate literature. It has several advantages over other options and has become the preferred method for closure of larger fistulas of the hard palate at the authors’ institution. It is a simple flap to raise, is reliable, and has minimal donor morbidity. The flap does not require tunneling, a second operation, or use of a bite block. The flap can easily reach the midline or the lingual central incisors. Additionally, it is well-vascularized, autologous tissue that epithelializes readily and can be used for either nasal or oral closure.
In the care of fistulas, as in most secondary cleft surgery, prevention of complications is key. A well-executed primary palatoplasty is the best defense against later fistula formation. A tension-free closure and careful post-operative care are crucial in prevention. To achieve tension-free closure, the surgeon should use relaxing incisions as necessary, perform a complete intravelar veloplasty, completely release the neurovascular bundle with optional osteotomy of the bony foramen, and use meticulous surgical precision to avoid unnecessary handling or crushing of the mucosal edges. The cleft palate surgeon will be rewarded more from preventing palatal fistulas than from correcting them.
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree