Scalp Reconstruction With Tissue Expansion
Finny George
Evan Matros
DEFINITION
Tissue expansion is the process by which an external force is applied to recruit the viscoelastic properties of the scalp to increase the size of the available healthy tissue.1,2
Restoration of the scalp to its prealopecia state is the primary goal of tissue expansion of the scalp. It is a crucial tool in the restoration of hair-bearing scalp.3
By expanding normal, healthy, hair-bearing scalp tissue, defects up to 50% of the total surface area of the scalp can be resurfaced.
There are three commonly used tissue expander shapes: round, crescent, and rectangular. The tissue expander shape used is not critical.
For large defects, multiple tissue expanders can be used simultaneously.
The base diameter of the expander should be approximately 2 to 2.5 times the size of the defect.
ANATOMY
The layers of the scalp are the skin, subcutaneous network (contains blood vessels, lymphatics, and nerves), galea aponeurotica, areolar plane, and pericranium.4
The galea is a fibromuscular central tendinous confluence of the occipitalis and frontalis muscles.
The loose areolar plane, deep to the galea, is the layer in which natural plane of separation of the scalp from the cranium occurs.
The parietal scalp has the greatest mobility and so can be helpful in local tissue recruitment. This quality can be used in tissue expansion.
The epidermis thickens, dermis thins, muscle thins, quantity of myofibroblasts increases, 30% to 50% of fat is permanently lost, high density of blood vessels grow, and a collagen/fibroblast capsule forms around the expander.
This increased angiogenesis that occurs in expanded flaps allows for improved survival and reliability.
Expanders are placed in the subgaleal plane, superficial to the pericranium.
PATHOGENESIS
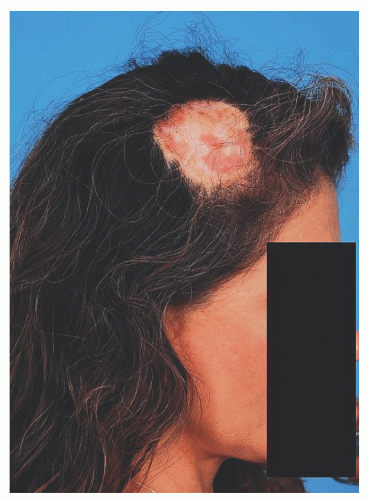
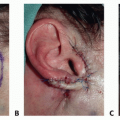
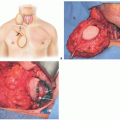
Alopecia of the scalp often results from trauma, burns, radiation, malignancy, or congenital disease (FIG 1).
Irradiated scalp may not expand well or may be associated with higher complication rates.
PATIENT HISTORY AND PHYSICAL FINDINGS
Pertinent history must be gathered from the patient and will include information on:
Circumstances surrounding development of scalp alopecia
Prior treatment or operations that were done, including failed treatments
Prior use of hardware or implants
History of radiation or chemotherapy
History of smoking, alcohol abuse, weight loss, diabetes, or bleeding disorders
Physical examination should gather enough knowledge to prepare an accurate preoperative plan.
Look for prior incisions.
Examine the skin quality and laxity.
Note unusual hair growth patterns including cowlicks.
SURGICAL MANAGEMENT
Preoperative Planning
Prior operative dictations should be reviewed to ensure that vascularity to the proposed area of expansion has not been disrupted or the area has not been irradiated.
The patient must be aware that he or she will have an abnormal appearance during the expansion process and that they will have multiple office visits to undergo the expansion.
They must be informed that at least two operations will be needed for this type of procedure.
Tissue expander placement
Tissue expander removal, scalp flap elevation, and closure with removal of alopecia areas
Risks specific to this operation should be discussed with the patient. They include alopecia along areas of new incisions, exposed tissue expander or inflation port, dog ears, partial or complete scalp flap loss, asymmetry, abnormal hair growth pattern, and the need for further surgery.
Preoperative antibiotics are administered.
Temporary markings should be placed on the patient in the preoperative area where there is ideal lighting and exposure, areas of laxity can be assessed, and hair growth patterns can be noted.