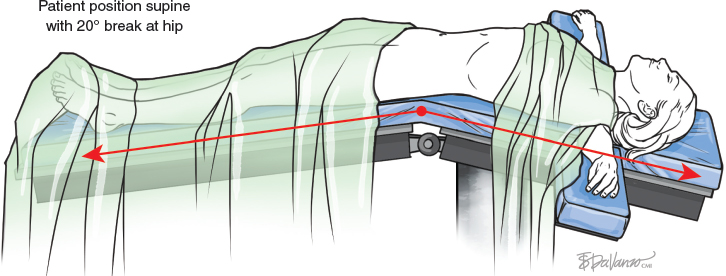
CHAPTER 12 From the patient’s point of view, liposuction offers a very good result with little risk. However, if a severe complication occurs, the patient faces a dramatic situation. In this chapter we will examine the evaluation of risks involved in this procedure and the means for preventing complications. The limits of volume aspirated and the extension of liposuction will also be discussed. Liposuction is essentially used to improve body contouring for aesthetic and reconstructive purposes by removing fatty deposits. The technique has been described for the treatment of localized fat deposits that may not respond to efforts of weight loss, such as exercise and dieting. Therefore it is important to stress that liposuction is not a weight-loss method. Patients for whom liposuction is ideally indicated should have good skin elasticity with little skin laxity so that the skin will adapt to the new postprocedure shape. The primary indications include the treatment of localized fat deposits in the abdomen, flanks, ankles, thighs, calves, buttocks, arms, and neck. With improvements of the technique and the development of less-traumatic cannulas, liposuction is now frequently used as an adjunct to many procedures, with little or no increase in morbidity. The main indications include the following: ■ Liposuction to correct gynecomastia. ■ Liposuction of the jaw and neck area during a facelift. ■ Abdominoplasty with liposuction of the flanks and to reduce dog-ears. ■ Lipoabdominoplasty, in which liposuction of the abdominal flap is performed before excess skin removal. ■ Previous liposuction in thighs and brachioplasty, in which liposuction is performed before skin removal. The advantage of this procedure is to adjust the skin envelope to the new contour promoted by liposuction. Obese patients and those with controlled diabetes who have moderate skin excess present a relative contraindication to liposuction. Liposuction is relatively contraindicated in morbidly obese patients and those with chronic obstructive pulmonary disease or with severe cardiac conditions. Patients with recurrent pulmonary emboli and with severe systemic diseases should not undergo this procedure. There are some controversial indications, such as for liposuction of breast parenchyma during reduction mammaplasty. Besides the presence of calcification in the mammogram after this procedure, it is possible that malignant cells may be spread by the cannula during liposuction. Liposuction of the abdominal flap during abdominoplasty is also controversial because of the potential for vascular damage. The use of liposuction to treat a large lipoma leaves behind its capsule, and thus it may recur. Patients over 60 years of age should be evaluated carefully for adequate skin elasticity before lipoplasty is planned. The surgeon should collect an extensive patient history and perform a careful preoperative physical examination. In discussion with the patient, the surgeon must determine whether the proposed procedure will adequately address the patient’s desired outcome to prevent disappointment and dismay with the result. Postoperative bruising and discomfort should also be fully discussed and an informed patient consent completed. Liposuction can be performed with the use of a local anesthetic, with or without intravenous sedation, or epidural or general anesthesia. Since the initial description of the liposuction technique, there has been a significant evolution regarding the anesthetic infiltration of the area to be aspirated as well as the operative technique and surgical instruments to be used. Patients should quit smoking for at least 15 days before surgery. Those who are taking birth control pills should discontinue their use 15 days before surgery. Blood cell counts, serum glucose, sodium, potassium, urea and creatinine levels, and coagulation tests should be performed preoperatively. In patients over 40 years of age, a cardiac evaluation should also be performed. The most appropriate anesthetic for each case should be analyzed, with consideration of the overall health and habitus of the patient, any comorbidities, the total volume to be aspirated, and the experience of the surgical team. A general anesthetic has the disadvantage of promoting dilation of the peripheral vessels by central stimulation, in addition to the consequent risks associated with intubation and assisted ventilation on the lungs. There is also the allergenic risk of the use of multiple drugs. Local anesthesia with sedation also presents some risks, such as respiratory depression and lidocaine intoxication (described later), besides the possibility of allergic reactions. The infiltration of the area to be aspirated is a very important issue when the risks of liposuction are being discussed, primarily because fluid injection will determine the amount of blood loss during the procedure and possible postoperative complications. Infiltration of the subcutaneous tissue can be done using a fluid containing saline solution (1000 ml) with 1 ml of epinephrine (1:1,000,000). Lidocaine (50 ml of a 1% solution) can be added to this solution when local anesthesia is chosen. There are four methods employed by surgeons for preparation of the area to be aspirated: 1. The liposuction technique in which no hypotonic fluids are injected is called the dry method. This technique has been abandoned by most plastic surgeons. The main disadvantage of the dry method is that there is a greater amount of perioperative blood loss, which could require a postoperative blood transfusion in some cases. Those who still use it believe that whenever infiltration is performed, the amount of fat to be removed is not easily quantified, thus decreasing the level of the surgeon’s accuracy during the procedure. It has been established that when the dry method is used to remove 1500 to 2000 cc of fat, there is no need for a blood transfusion in healthy patients. The estimated blood loss ranges from 20% to 45% of the final aspirated volume when the dry liposuction method is employed. 2. Few surgeons today use the wet technique, in which the amount to be injected in each area varies from 200 to 300 ml. The blood loss ranges from 4% to 30% of total aspirate. 3. In the tumescent technique, for every 2 to 3 ml of fluid injected, only 1 cc is aspirated. The volume of blood loss is about 1% of the final aspirated volume. 4. In the superwet technique, the volume of fluid to be injected is about the same as the expected final volume of fat to be removed (in a 1:1 ratio). The blood loss is about 1% of the final aspirated volume when this technique is used. Despite these four alternative methods of preparing adipose tissue to be aspirated, many surgeons prefer the superwet method because of the low blood loss, better fluid balance, and no fluid overload that could lead to cardiac failure (a complication seen after the use of the tumescent technique). When the superwet technique is used, the epinephrine in the injectate promotes vessel constriction. In addition, the large volume of injected fluid plays an important role by compressing the walls of the vessels. Both of these factors contribute to decreased blood loss. This solution emulsifies the fat, which makes the liposuction technique easier to perform. It is also possible to warm up the solution to avoid a hypothermic state. Infiltrating and aspirating two or three areas at a time is a prudent way to prevent fluid overload. Intravenous volume replacement in the superwet technique is controversial. Some studies advocate the use of saline solution after 5 L of lipoaspirate have been removed, whereas others indicate fluid replacement based on the need for intravascular volume expansion. It is essential to monitor and evaluate the patient’s urinary flow in these cases. It is extremely difficult to evaluate the risks associated with liposuction, because there are many variables involved in every case, such as the volume to be aspirated (and thus the length of the procedure), the use of various techniques of liposuction and infiltration solutions, the surface area over the tissue to be suctioned, the patient’s overall health, and other relevant factors. In 2001 Bruner and de Jong studied 292 cases of patient medical liability claims related to liposuction over a 13-year period. The authors verified that only 2% of these patients had severe morbidity with permanent deformities, and seven patients (2.4%) died. These percentages show that although many patients entered claims for compensation through the judicial system, the rate of permanent deformities and death was rather low in relation to the total number of lawsuits. Some risks may be related to technique during liposuction. Large cannulas may increase the risk of skin irregularities, because they tend to remove more fat in some areas. Therefore cannulas larger than 4 mm in diameter should not be used. Larger cannulas can be used in areas in which skin will be removed. The power of penetration of the cannula depends on the distalmost point of the tip. LAL uses the principles of selective photothermolysis to preferentially lyse adipocytes while leaving surrounding structures unaffected. The disadvantages of LAL include the potential of thermal injury, the high costs of equipment, and prolonged procedural time. Initial studies evaluating first-generation laser devices showed, in randomized trials, no increased cosmetic benefits of LAL when compared with traditional SAL. Cannulas with more triangular tips may have a higher risk of penetration; therefore these cannulas should not be used in the abdominal area. The infiltration cannula has a much smaller diameter (approximately 1 cm) and also has more risk of penetrating the abdominal cavity. Theoretically, if there is an accidental cannula penetration, the risk of visceral perforation is increased if there is a continuous vacuum, such as in PAL or when any suction machine is used. On the other hand, if a syringe is used to produce vacuum during liposuction and the cannula penetrates the abdomen, the vacuum in the syringe will be limited to at most 60 cc (total capacity of the syringe). During liposuction some of the syringe is filled with fat, so it is reasonable to consider that on average, the vacuum will be generated in 30 cc of the remaining volume of the syringe without fat. The most feared situation is bowel perforation, leading to peritonitis. Bowel perforation is produced by the effect of suctioning the intestine wall, combined with the cutting orifice of the cannula. The suction capacity of a syringe is limited, and it will be less likely to cause bowel perforation. However, the use of a syringe will not prevent injury of large vessels and parenchymal organs. Another way to prevent abdominal wall perforation is the use of abdominal hyperextension by folding the bed in the opposite way, as is done during an abdominoplasty. This will change the concave shape of the abdomen to a more convex shape, which may decrease the risk of abdominal wall perforation during liposuction. When death occurs after liposuction, the cause is not always easily identified because of technical difficulties, such as authentication of collected data, patient and surgeon privacy issues, and judicial secrecy in legal cases. Grazer and de Jong in 2000 conducted a census survey with responses from 917 board-certified plastic surgeons between 1994 and 1998. They verified that these surgeons had 95 deaths in 500,000 patients who had undergone liposuction. This is a mortality rate of approximately 1:5000. The most frequent cause of death was pulmonary embolism (23%), followed by abdominal perforation (14.6%). The third most common cause of death was related to the use of anesthetics, sedation, and medication (10%). This last number is probably underestimated, because most deaths in these cases occurred out of the hospital, possibly from lidocaine intoxication. Hemorrhage, which was once the most common cause of death associated with lipoplasty when the dry technique was used, was responsible for only 4.6% of the known causes of death. The number of fatalities from liposuction increased in the 1990s, compared with the previous decade. This is in part because there was a limit of 2 L in the volume to be aspirated when the dry technique was used in the 1980s, when the mortality rate of liposuction was 12.7:100,000. After the use of infiltration, the volume limit has become debated, and more extensive liposuction is performed. The death rate has increased to 20:100,000. There are many other reasons for the increase in the death rate. The most obvious is the length of surgery and the extension of trauma that are related to thromboembolic phenomena. Other factors that may contribute to this increase in fatalities include liposuction being performed as an outpatient procedure; excessive fluid infiltration; excessive fat removal, resulting in the intravascular volume moving to the third space; and multiple surgeries. Besides these factors, lidocaine intoxication and excess of epinephrine also contributed to this increase in the mortality rate (see Lidocaine Toxicity later in this chapter). The risk of thrombosis is related to a decrease in blood flow to the lower limbs, trauma, and hypercoagulability. A decrease in blood flow occurs as a result of the patient’s positioning and immobilization during surgery. Trauma is a common factor of all surgeries and occurs in areas where the liposuction is performed. However, because there has not been a defined safe limit for liposuction, surgeons have progressively increased the volume of liposuction of patients. Hypercoagulability is related to individual factors, clinical conditions, and the use of certain drugs (commonly, birth control pills). To verify whether liposuction could generate a “hypercoagulability state,” Smith and Levine checked the prothrombin time, partial active thromboplastin time, antithrombin III, and the thrombin-antithrombin complex serum levels in patients who underwent liposuction. These authors verified that there were no changes that could influence coagulation during liposuction in these parameters. However, it cannot be verified with certainty whether there are other coagulation factors involved. Prevention of this condition can be achieved with careful patient selection, placing compressive devices on the lower limbs during and after surgery, the use of low-molecular-weight heparin, a short operative time, early ambulation, and having the patient wear compressive stockings in the postoperative period. Surgeons should carefully search for abdominal wall hernias before performing liposuction in the abdomen. Small hernias (1 to 2 mm in diameter) are not diagnosed clinically, by ultrasonography, or by any other imaging methods. Their usual location is in the midline, at the umbilical and supraumbilical area. In addition, the subcostal area in some patients can project, and this condition increases the potential for cannula penetration. Because during a lipoplasty procedure hundreds of penetrating movements of the cannula are made, the surgeon must always be mindful of the risk of visceral perforation. Abdominal perforation may also occur during fluid infiltration, because infiltration cannulas have a smaller caliber than aspiration cannulas, and thus they are more likely to force a penetration in the abdominal wall. The incidence of abdominal wall perforation is higher than one might expect. Although many surgeons do not believe that they can make such a drastic error, they should exercise every precaution to prevent this. When the total number of liposuctions performed in the world is multiplied by the number of movements the surgeon makes with the cannula when performing the procedure, the result is a number in the billions of penetrating movements, each one with the potential risk of penetrating the abdomen. To prevent this complication, it is important to place the incisions in a favorable position, considering the naturally projecting areas that will facilitate cannula penetration into the abdominal cavity, such as the costal margin projection. To avoid deepening the thrust of the cannula, the surgeon’s nondominant hand should always follow the tip of the cannula during the procedure, especially in obese patients. The patient’s position on the operating table is very important. The abdomen should be in hyperextension, which makes the abdomen more convex, compared with the concave shape of the abdomen when the patient is lying supine.
Risks and Limits of Liposuction
Indications and Contraindications
Patient Selection
Anesthesia and Preoperative Care
ANESTHESIA, SEDATION, AND MEDICATIONS
INFILTRATION OF THE AREA TO BE ASPIRATED
Risks Associated With Lipoplasty
SURGICAL TECHNIQUE
CAUSES OF DEATH
Evaluation of the Risk Factors
PULMONARY THROMBOEMBOLISM
ABDOMINAL WALL PERFORATION
Plastic Surgery Key
Fastest Plastic Surgery & Dermatology Insight Engine

 Lydia Masako Ferreira
Lydia Masako Ferreira