Fig. 22.1
General algorithm for revisional bariatric surgery for other reasons than surgical complications. VBG means vertical banded gastroplasty, SG means sleeve gastrectomy, GERD means gastro-esophageal reflux disease, DS duodenal switch
Anatomical situation of the stomach: We mentioned above the two typical complications after LAGB, i.e., the band erosion and the band slippage. The anatomical changes induced by these complications may preclude safe accomplishment of some procedures. Thus, many surgeons will be reluctant to perform LSG after band erosion because of the significant danger for leaks in an area that is already at stake because of poor vascular supply [23].
Presence of GERD: Patients who experienced significant GERD after LAGB should probably not be converted to LSG because of documented concerns that LSG aggravates GERD on midterm follow-up [24].
22.3 Technical Aspects of Conversion Procedures After LAGB Failure
Band erosion (also known as intragastric migration of the band) constitutes a specific and peculiar situation. Symptoms of this condition may include frank septic symptoms, but more subtle signs may be present, such as vague abdominal discomfort and loss of restriction experienced by the patient [25]. Once the condition has been diagnosed, band retrieval by endoscopic approach is to be preferred [26]. Alternatively, laparoscopic gastrotomy performed at a distance from the band may be carried out, allowing for band removal through the opening in the stomach [27]. This approach avoids the phlegmonous area surrounding the erosion site and deals with the risk of persisting gastric fistula.
Except for the specific case of band erosion that precludes immediate conversion, once the decision has been made to proceed with band ablation for other indications, the question remains if the band removal should be complemented by another bariatric procedure at the same stage, versus after a lag time. Staged conversion to RYGB reportedly is characterized by a reduced incidence of anastomotic stricture [28]. Other sources, however, favor the completion of the corrective procedure concomitantly with the band removal [29]. In our department, we prefer to perform band ablation and conversion to a new bariatric construction in one stage. We believe that the band constitutes a highly visible landmark as well as a handy retraction tool. In fact, we usually leave the band in place until full dissection of the upper pole of the stomach has been performed. Conversely, when one decides to proceed with the delayed approach, it is important to anticipate on possible problems during the revisional procedure. Hence, the gastrogastric stitches overlying the band should be severed; to avoid the risk of stapling across a double layer of tissues should one decide to perform a gastric bypass or LSG as revisional procedure. It is probably preferable as well to incise or even to remove the pseudo-capsule under the band, because this may reduce the risk of stenosis after the final procedure, as described some 20 years ago [30].
22.3.1 Dissection of the Adjustable Band
In this paragraph, we will try to highlight the essential steps of band removal and conversion to another procedure, as we usually perform it, i.e., in one stage.
Unlike some, we believe that the conversion procedure should imply a complete dissection of the upper pole of the stomach and of the hiatus. Dissection of the hiatus will possibly unveil a sliding or para-esophageal hernia that must be cured. It may also reveal a diastasis of the crurae, a condition that may favor the development of an intramediastinal migration of the remnant, as experienced by two of our patients who underwent band ablation and conversion to RYGB (unpublished data). One should, however, be aware of the possible hazards involved with the dissection around the hiatus, especially in the presence of substantial deformations caused by scar tissue around the band. One of the most dangerous steps of the dissection pertains to the freeing of the right crus. The vena cava is located in this very area and may be obscured by the scar tissue. The essential landmark in the area is the caudate lobe of the liver. After severance of the anterior adhesions of the liver to the upper part of the stomach, the bare surface of the stomach, obscuring the band to a certain degree, as well as the phreno-esophageal ligament become visible. Lateral traction of the band tubing allows for dissection of the lateral edge of the caudate lobe (Fig. 22.2).
Fig. 22.2
The upper pole of the stomach is usually plastered with the liver. After freeing the anterior adhesions, dissection should be oriented towards the edge of the caudate lobe. Opening the space at the edge of the caudate lobe opens the way to the right crus
The thick peritoneal layer overlying the edge of the lobe should be incised sharply, hereby opening the angle between the liver and the right crus. This angle should not be dissected any further to avoid lacerating the vena cava. Rather, the right crus should be adequately located and, again aided by forceful retraction of the band tubing in a lateral direction, the peritoneal layer overlying the crus should be incised. This latter maneuver readily reveals the distal esophagus (Fig. 22.3), which, in turn, will allow safe dissection of the adhesions overlying the buckle of the band and the right side of the band. Care must be taken not to damage the left gastric pedicle in this vicinity, and in case of doubt, this step should be delayed until later. Dissection should now be directed towards the apex of the hiatus and the left crus should be dissected from anterior going dorsally, but staying short of the angle of His (Fig. 22.4). Once the right side of the band has been freed, the lateral aspect of the band should be dissected. Starting at the previously dissected area of the band and going to the left, the gastro-gastric bridge overlying the band can now be dealt with, usually by following the several stitches that had been placed to fix the band (Fig. 22.5). Whenever the plane between the proximal and the distal part of the gastro-gastric bridge is not readily visible, one should rather err towards the distal side, because distal accidental opening of the gastric lumen is less of an issue than a proximal perforation. Severance of the gastro-gastric stitches must be complete, but sometimes the most lateral portion is difficult to reach from the right side and this step should be deferred until later. Dissection thus closes in on the angle of His, which quite often is the most difficult step. One should be aware that in an effort to provide additional stability when inserting the band, some surgeons place a stitch from the stomach distal to the band to the root of the left crus, which obviously obscures the field during a revision. We believe it is advantageous at this stage to halt the dissection in the vicinity of the His angle and to resume dissection at the interface between spleen and upper fundus. The first few short vessels may now be ligated, which will create a distance between the lateral edge of the fundus and the spleen and give access to the lesser sac (Fig. 22.6). By retracting the freed edge of the fundus anteriorly and from left to right, the usually untouched posterior aspect of the stomach becomes readily visible. The thus created space posterior to the stomach has the shape of a pyramid, with the edge of the fundus anteriorly as base, the pancreas posteriorly and the and spleen edge laterally, while the apex is constituted by the adhesions overlying the posterior aspect of the band, with, to the right of this area, the left gastric pedicle (Fig. 22.7). The posterior adhesions overlying the band, including the ones at the extreme left side may now be safely transected. The final dissection of the angle of His, substantially facilitated by the complete freeing of the tissues all around the area, concludes the preparation for the removal of the band. The fully dissected hiatus should be thoroughly inspected and the surgeon should not hesitate to perform adequate closure of the crurae. The band should still be present at this stage because it significantly helps in a safe and correct hiatoplasty. We usually perform a posterior closure and use one or more figure of 8 stitches of polypropylene material, buttressed by cellulose pledgets (Surgicel, Johnson & Johnson) to avoid cutting through the tissues when the sutures are tied (Fig. 22.8). After completion of the hiatoplasty, the repair should fit snugly around a 34-French orogastric tube. With the band completely free, and the hiatal repair performed, transection or opening of the band can now be carried out. The pseudo-capsule caused by the impression of the band should be incised at this time (Fig. 22.9).
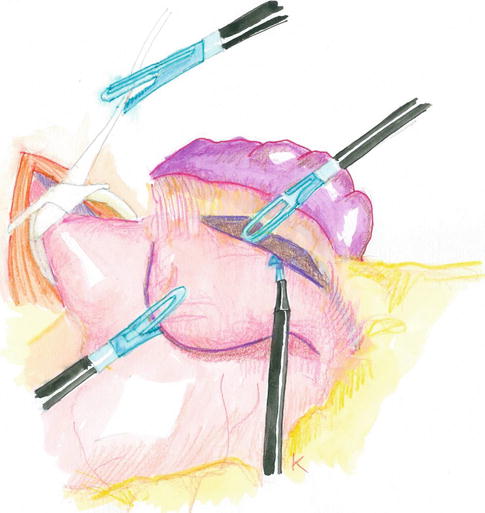
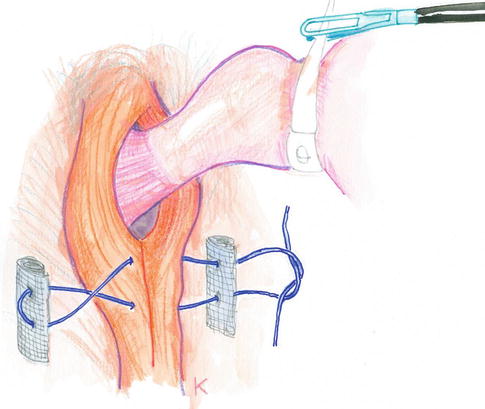
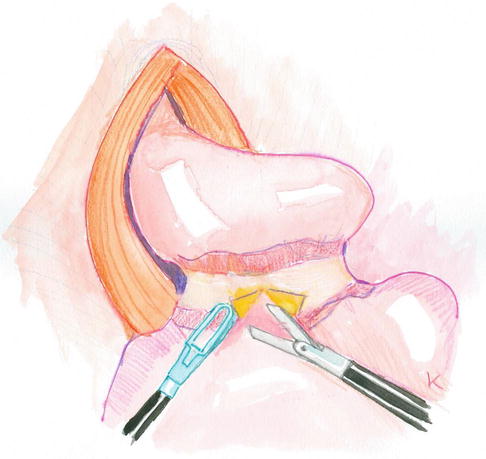
Fig. 22.3
The peritoneum overlying the right crus is incised which allows for exposing the esophagus. The presence of the band is advantageous for forceful retraction of the upper pole of the stomach
Fig. 22.4
Forceful retraction of the band to the right side of the patient helps with dissecting the left crus, while the esophagus is well visible and out of harm’s way
Fig. 22.5
Before attempting to dissect the angle of His, the stomach bridge overlying the band should be incised to reveal the ventral face of the band, lateral to the buckle. The stitches unting the gastrogastric bridge constitute an excellent landmark
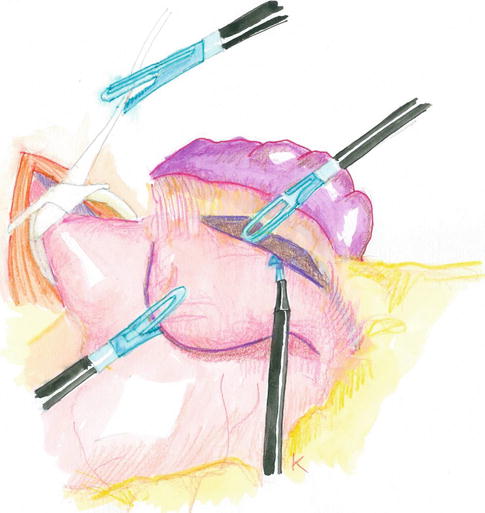
Fig. 22.6
A good strategy in preparing the dissection of the His angle is to open the space between the fundus of the stomach and the spleen, which is achieved by severance of the uppermost short gastric vessels. This maneuver widely opens the lesser sac. Subsequent ventral retraction of the fundus reveals the adhesions between band and angle of His, that can now safely be dealt with
Fig. 22.7
The dissection of the upper pole of the stomach, including the hiatal crurae, is now complete. Now is the right time to perform the hiatal closure, which is carried out by at least one posterior figure of 8 stitches, buttressed by resorbable pledgets
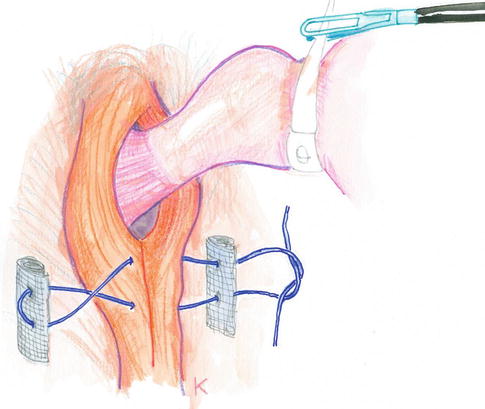
Fig. 22.8
By lifting the fundus from left to right, the posterior aspect of the band is well visible and can be freed from its last attachments. The main trunk of the left gastric artery (arrows) can be spotted at the superior edge of the pancreas, more often than not in very close vicinity of the band
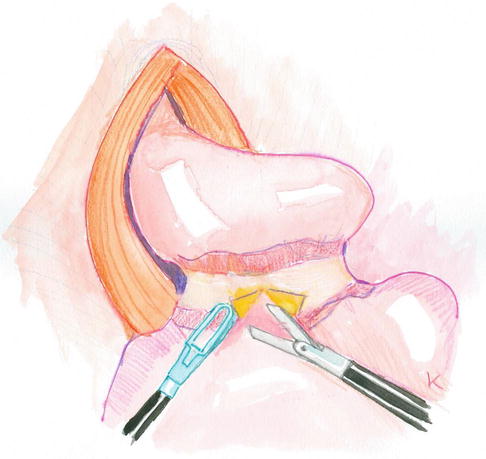
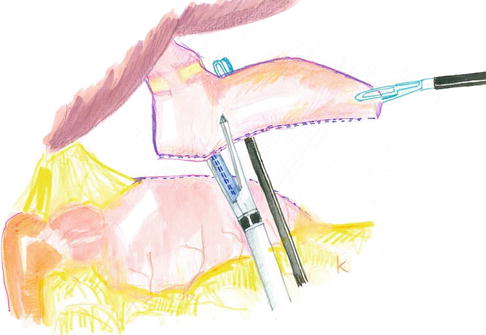
Fig. 22.9
The band has been removed. The underlying pseudo-capsule should be resected or transected (as shown here) to avoid subsequent stenosis
After removal of the band, the surgeon should inspect the freshly dissected upper portion of the stomach and evaluate the possibilities. Significant damage to the tissues may thus preclude safe stapling or suturing and may lead the surgeon to perform a gastric bypass with eso-enteral anastomosis. Conversely, if local conditions did not allow thorough dissection of the band before removing it, it may be wise to abandon the efforts to obtain a small pouch and to prefer the option of performing a BPD. Usually, however, integrity of the tissues is satisfactory and will permit the planned procedure, i.e., either a gastric bypass or (seldom) an LSG. For either technique, we are concerned about possible damage to the main trunk of the left gastric artery. This is why during the preparation of a gastric bypass or a LSG, we limit the dissection at the lesser curvature to a strict minimum and will focus on the greater curvature.
22.3.2 Transection of the Stomach
Over the years, we have gathered experience with over 500 band removals and conversions to RYGB (or, seldom, OLGB and LSG). We have tried to standardize the technique and to develop a strategy that would be similar for whatever construction. The strategy implies the resection of the upper part of the fundus, even in case of gastric bypass. This maneuver has the advantage of diminishing the risk of gastro-gastric fistula formation in revisional procedures [31] and to interfere with the production of Ghrelin, which in turn may improve weight loss [32].
We previously described that the uppermost short gastric vessels are routinely sacrificed during the freeing of the band. With this technique, the lesser sac is widely opened, which gives free access to the posterior surface of the stomach.
When the foreseen procedure is a gastric bypass, the lesser curvature can now be approached posteriorly. The level of dissection will depend on the type of bypass, i.e., RYGB versus OLGB, and be performed rather close to the band impression for the former and more distally for the latter. In all cases, however, the dissection of the lesser curvature is initiated posteriorly, distally to the previous band placement, where tissues are supple and tissue distortion minimal. By lifting the stomach anteriorly, the tissues at the lesser curvature are placed under traction and the space between the vessels and the stomach itself can safely be dissected by the coagulating hook or by the harmonic scissors, until the tip of the dissecting tool emerges on the ventral aspect of the edge of the lesser curvature. The thus created opening in the peritoneal sheet constitutes the aim for the linear stapler when it transversally transects the stomach. Transection is performed from left to right, approximately at a right angle with the long axis of the stomach (Fig. 22.10). Thanks to the dissection performed at the lesser curvature, lesion to the main arterial trunk should be avoided and bleeding kept minimal.
Fig. 22.10
The stomach is now transected from left to right, hereby avoiding dissection of the lesser curvature, that may be distorted by adhesions. The vessels at the lesser curvature are dissected from posterior, in the lesser sac that usually has remained untouched
After complete transverse transection of the stomach, the entire lateral proximal part of the stomach (i.e., the fundus) is forcefully pulled laterally and a 34-French orogastric tube is advanced by the anesthesiologist and is maneuvered close to the lesser curvature until it hits the transverse staple line. This maneuver is essential to obtain a narrow gastric tube, and may prove difficult, especially in the presence of a dilated pouch. However, because of the thoroughness of dissection prior to removal of the band, it should be possible to place a grasper from the left upper quadrant trocar posterior to the stomach, and, keeping it close to the lesser curvature, advance it to the root of the left crus, which will facilitate the correct placement of the large bore tube. With the 34-French tube in place, vertical stapling can be carried out, again while exerting adequate outward traction on the fundus to avoid making the gastric pouch too wide (Fig. 22.11). After complete transection of the stomach, as described, the fundic part has been entirely isolated and should now be removed, care being taken to sever all possible remaining attachments. After extraction of the isolated fundus, the proximal gastric pouch should be inspected. If it is deemed too long (as for RYGB) it can now safely be trimmed to an appropriate size before performing a gastro-enterostomy.