Revision of Nipple Areola Reconstruction
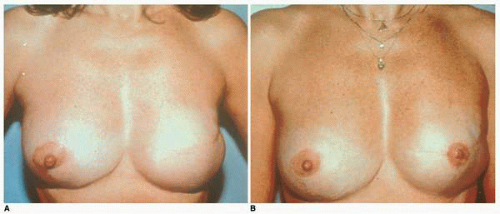
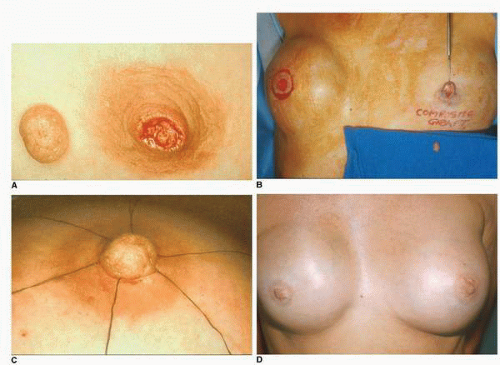
The nipple is a unique structure that in its natural state has an important physiologic function in terms of breast-feeding. It also confers to the breast both an aesthetic and sexual dimension. Reconstruction of the nipple following mastectomy visually transforms the newly created breast mound into a breast, and subsequent areola color patch duplication gives to the reconstructed breast the maximum amount of realism that any breast reconstruction can ever achieve (Fig. 10-1A,B).
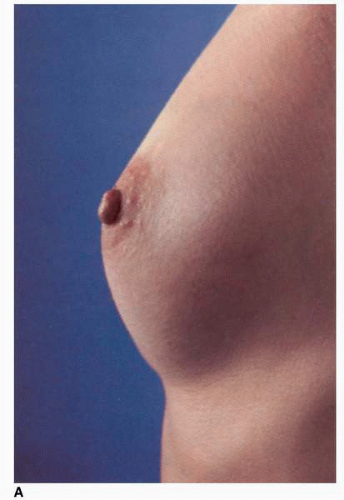
The nipple is an essential aesthetic feature of the breast (Fig. 10-2A) and it is the hub around which the rest of the gland emanates. Anatomically the nipple represents the terminus of the multiple lactiferous ducts1 (usually 20 to 30) that run through the breast (Fig. 10-2B). These ducts are clustered in the nipple and functionally they allow egress of mother’s milk. They contain fibrous tissue and specialized muscle elements. The nipple is surrounded by areola tissue, which is a darkly pigmented epithelium that has a small number of ducts opening into it. In addition, this areola tissue contains Montgomery glands or tubercles and lanugo hairs (Fig. 10-2A). The areola skin is visually darker than the surrounding breast skin but is slightly lighter in pigmentation than the nipple.1 The nipple is most aesthetically positioned at the point of maximal projection on the breast mound.1 It can be located by the transposition of the inframammary (IM) fold (done routinely in planning a breast reduction) or by measurements from fixed points of reference on the anterior chest (done in most nipple reconstructions following a previous breast reconstruction). The distance from the nipple to the suprasternal notch and the IM fold varies from patient to patient (Fig. 10-2C,D). In the absence of previous surgery
or an obvious developmental asymmetry the nipple positions are roughly symmetric.
or an obvious developmental asymmetry the nipple positions are roughly symmetric.
When nipple areola reconstruction is performed the optimal visual appearance of the reconstructed nipple is achieved by simulating the best possible color match with the opposite areola. In the past this was accomplished with the transplantation of a darkly pigmented full-thickness skin graft (vulva or proximal medial thigh skin). Currently, however, this is best done with an intradermal tattoo, which can produce the most predictable symmetry with the opposite areola in a wide variety of colors.1
Symmetrically reproducing the size, shape, and color of the opposite areola must be the surgeon’s goal in every nipple areola reconstruction. In my opinion the most important characteristics of successful nipple areola reconstruction are pigmentation, position, and projection—in that order.
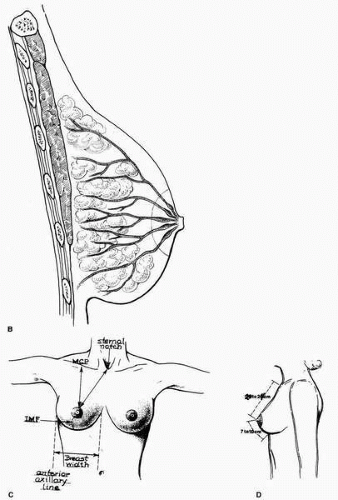
Visual symmetry between the color and location of the nipple areolar complex (NAC) on the opposite breast and its position on the reconstructed breast mound is paramount for the optimal visual appearance of the reconstructed nipple. This symmetry can be most ideally enhanced and most consistently reproduced using an intradermal tattoo, with which the surgeon can best simulate the color patch of areola skin on the opposite breast. As stated, the color of the areola around the reconstructed nipple is more important than either the position or the projection of the areola. Indeed, color patch symmetry can compensate for partial or even significant loss of nipple projection or slight abnormalities in position. This is illustrated in this patient (Fig. 10-3), who sustained a significant loss of nipple projection, marring what was otherwise a good left breast reconstruction with a TRAM flap. This situation was rescued by a well-done intradermal tattoo, which produced an excellent aesthetic outcome. (Fig. 10-3A-D).
In terms of timing, I believe that nipple areola reconstruction is best done at a second stage rather than during the primary breast reconstruction procedure. This allows the breast mound to mature in terms of evolution of shape and gravitational settling. In my practice nipple reconstruction is most often combined with a procedure to revise and reshape the reconstructed breast. In cases where the reconstruction is performed with tissue expansion followed by secondary placement of an implant, I perform the nipple reconstruction as a third stage,
although others2,3 will perform the procedure at the time of subsequent implant placement. Performing a simultaneous nipple reconstruction at the time of exchanging the expander for an implant carries with it a small but definite increased risk of losing the implant due to problems with wound healing and subsequent exposure and/or infection at the site of nipple reconstruction.2,3
although others2,3 will perform the procedure at the time of subsequent implant placement. Performing a simultaneous nipple reconstruction at the time of exchanging the expander for an implant carries with it a small but definite increased risk of losing the implant due to problems with wound healing and subsequent exposure and/or infection at the site of nipple reconstruction.2,3
NIPPLE RECONSTRUCTION OPTIONS
Historically, the options for nipple areola reconstruction have been tattoo alone; the use of composite grafts such as toe pulp,4 earlobe,5 labia minora6; or most commonly a composite graft of a portion of the contralateral nipple7 from the opposite breast (in patients with extremely large nipples). Over the past twenty years pullout skin flaps raised at the desired nipple position have represented the state of the art8, 9, 10, 11 and 12 in nipple reconstruction. The most commonly used flaps are listed in Table 10-1. Reconstruction of the areolar region is then performed using either a full-thickness skin graft with darkly pigmented skin13 or, as noted earlier, an intradermal tattoo,14,15 which is the best way to create symmetry of areola color.
An intradermal tattoo alone for nipple reconstruction may be sufficient in the elderly, high-risk patient who desires a semblance of visual symmetry15 but in whom it may not be wise to have a formal nipple reconstruction due to local tissue conditions (i.e., scarring of skin, atrophy of dermis, and subcutaneous adipose tissue).
TABLE 10-1 Nipple Reconstruction Options | ||||||||||||||||||||||||||||||||||||||||||
|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|
| ||||||||||||||||||||||||||||||||||||||||||
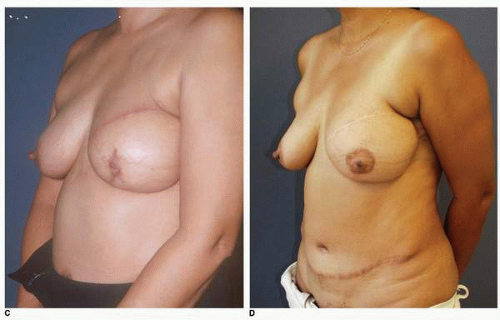
With the exception of nipple sharing,7 composite grafts, which were important in the early days of nipple reconstruction (e.g., earlobe, toe pulp), are largely relegated to the role of historic significance alone. I believe that there is still a place, albeit rarely, for nipple sharing. This technique is applicable in special circumstances of primary reconstruction where there are extremely thin and attenuated tissues or scarring in the desired position of nipple reconstruction in the patient who has a large opposite nipple that might serve as donor tissue for nipple reconstruction (Fig. 10-4A-D). In addition, a composite graft of the nipple is also helpful in a difficult secondary case to treat the complication of loss of nipple projection in selected instances where the option of local flap reconstruction is unavailable. Such a case is illustrated in Figure 10-4.
Nipple sharing involves removal of either the distal or most anterior aspect (Fig. 10-4A) of the nipple or excision of a pie-shaped portion of the nipple on its undersurface (Fig. 10-4B). It obviously decreases the size of the donor nipple, which in some cases may be a benefit. It also results in a scar on the donor nipple. However, when such composite grafts are placed in the appropriate location and surrounded by an intradermal tattoo, they can produce a good simulation of the patient’s opposite nipple (Fig. 10-4D).
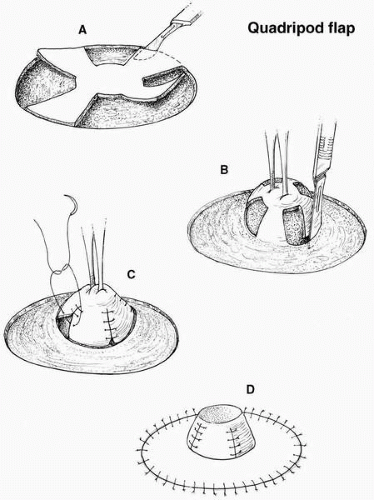
Currently the most popular technique for nipple reconstruction involves the use of a pullout flap8, 9 and 10 of skin and subcutaneous adipose tissue at the ideal site on the reconstructed breast mound with the application of an intradermal tattoo for the areola reconstruction. Many designs are possible and these are outlined in Figure 10-5. Varying degrees of success can be achieved with pullout flap reconstructions based on their design. That is to say, the design of the specific nipple flap may indeed play a role in the ultimate projection. I believe that some flap designs are inherently better than others.
For example, I have found that the quadripod design16 (Fig. 10-6), which employs a direct elevation of the tissue with closure of flaps at the base of the nipple, is unreliable in terms of producing and maintaining long-term nipple
projection. This technique often produces a nipple that looks excellent on the operating table but it loses most of its projection with time (by 1 year postoperatively). To the surgeon who studies this design and analyzes the technique of elevation, this loss of projection would seem to be almost intuitive. The forces of wound contraction would act to directly pull this tissue back down to the plane of the breast surface, thereby predisposing it to and potentiating loss of projection.
projection. This technique often produces a nipple that looks excellent on the operating table but it loses most of its projection with time (by 1 year postoperatively). To the surgeon who studies this design and analyzes the technique of elevation, this loss of projection would seem to be almost intuitive. The forces of wound contraction would act to directly pull this tissue back down to the plane of the breast surface, thereby predisposing it to and potentiating loss of projection.
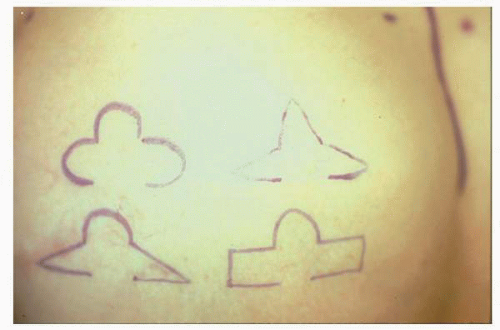 FIGURE 10-5. Pullout flaps. These are the most commonly used skin designs for skin and subcutaneous adipose flaps used for nipple reconstruction. |
In contrast, the flap techniques that elevate skin and adipose tissue off of the reconstructed breast, detaching it at all areas but the base of the flap and then reconfiguring it into the desired nipple shape, are more successful in terms of maintaining their projection.8, 9, 10 and 11, 17, 18, 19 and 20 The elements in the flap responsible for the nipple projection are adipose tissue and the thickness of the dermis. The more reliable designs are those in which the flap tissue used for reconstruction of the new nipple is elevated, or pulled out, to at least a 90-degreen angle from the surface of the breast mound. Such procedures are variations of the skate design originally proposed by Hartrampf,11 which were subsequently modified and refined by Little and Spear (Fig. 10-7).17,18
It has been my observation that the modified star design19 can reliably produce small to moderately projecting nipples (Fig. 10-8; ≤5 mm). For the reconstruction of larger nipples, my choice is the skate design18 (Fig. 10-7). The fishtail flap developed by McCraw20 (Fig. 10-9) also has the ability to produce a nipple with very marked projection. Such designs may allow the maintenance of greater long-term projection. Of particular advantage is a modification of the fishtail flap design that is used when there is a transversely oriented scar slightly above or slightly below the desired nipple position (Fig. 10-10). This design makes it possible to reconstruct the nipple without placing any new scars on the reconstructed breast. It may be based either superiorly or inferiorly, depending on the desired nipple position.