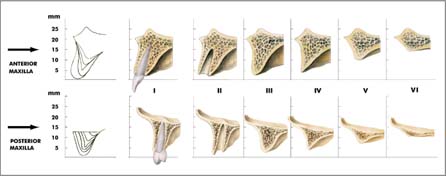
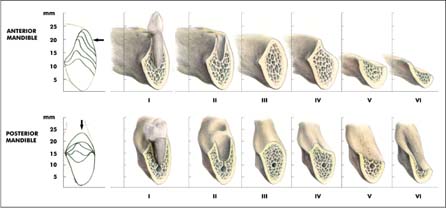
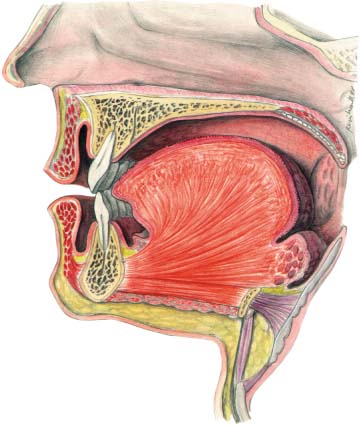
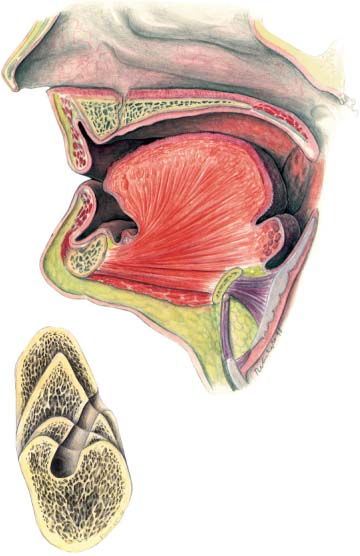
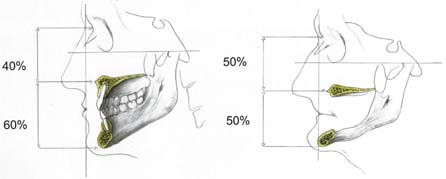
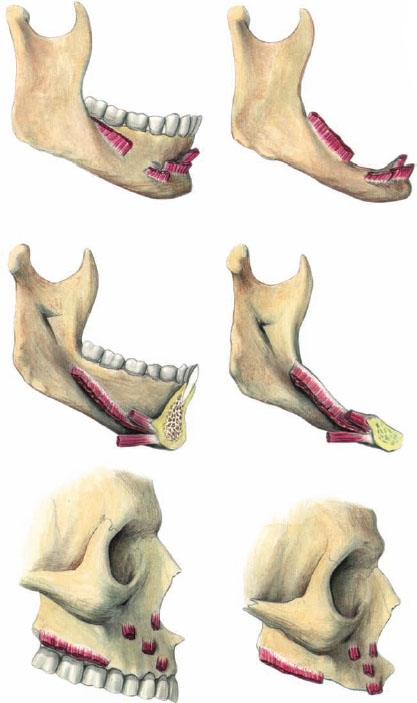
29 Reconstructive Preprosthetic Surgery and Implantology Reconstructive preprosthetic surgery can be defined as the restoration of oral function and facial form, rendered deficient through loss or absence of teeth and related structures, by a combination of surgical and prosthetic means. Nowadays the application of endosteal implants has extended the scope and effectiveness of reconstructive preprosthetic surgery (Cawood and Stoelinga, 1996). Of the many variables that govern the use of such implants the availability of sufficient bulk of bone is the most important. There is a progressive reduction in the residual alveolar ridges, following the loss of teeth, due to alveolar bone resorption, which occurs relatively rapidly in the first year after tooth loss and then continues at a slower rate for many years (Tallgren, 1972). This process occurs to a greater extent in the mandible compared with the maxilla and leads to a quantitative and qualitative reduction of the alveolar bone. Cawood and Howell (1988) analyzed patterns of alveolar resorption and described a pathophysiological classification of alveolar resorption, which is accepted internationally (Figs. 29.1, 29.2). When considering reconstructive preprosthetic surgery of the edentulous jaw, it is important that the clinician fully understands the anatomical consequences of reduction of the residual ridges. Based on a classification of the edentulous jaws, changes in the relationship of the jaws to each other, in muscle relations and function, in the oral mucosa and in facial morphology have been measured relative to the stage of resorption of the edentulous jaws (Cawood and Howell, 1991). With progressive resorption from class I to class VI there are three-dimensional changes in jaw relations. Anteroposteriorly the mandibular and maxillary arches become shorter. Transversely, due to the pattern of resorption, the maxillary arch becomes progressively narrower while the mandibular arch becomes progressively broader. Vertically the interarch distance increases, although this is counteracted to some extent by the vertical shortening of the lower face caused by the autorotation of the mandible producing a more prominent chin and prognathic jaw relationship (Figs. 29.3–29.5). Fig. 29.1 Modified classification of edentulous jaws (maxilla). Class II, post dental extraction; class III, broad alveolar process; class IV, narrow alveolar process; class V, flat ridge (loss of alveolar process); additional class VI, no ridge (total loss of alveolar process). Fig. 29.2 Classification of edentulous jaws (mandible). Class II, post dental extraction; class III, broad alveolar ridge;class IV, knife-edge alveolar ridge; class V, flat ridge (resorption of alveolar process); class VI, submerged ridge (resorption of basal process). Fig. 29.3 Dentate jaw. Normal dental, jaw and soft tissue relationships. Fig. 29.4 Edentulous jaw. Encroachment of lips, tongue, and floor of mouth associated with jaw atrophy. Cross-section of the mandibular body in the foramen mentale region (resorption of alveolar process and change of the position of the mental foramen). Fig. 29.5 Consequences of jaw atrophy. Decreased lower face height, relative prognathism, and collapse of lower facial soft tissue are shown. The attachments of the circumoral musculature and that of the floor of the mouth delineate the extent of the vestibular and lingual sulci. With the continued loss of alveolar bone from class I to class VI these muscles become progressively more superficial (Fig. 29.6). In the edentulous jaw the mucosa covering the residual ridge comprises partly keratinized attached mucosa and partly unattached mucosa. With the resorption of the alveolus, the quantity of both attached and unattached mucosa diminishes significantly. In the mandible, as a result of alveolar bone loss, the inferior alveolar canal becomes relatively superficial (Fig. 29.7). In the dentate mandible the blood supply is principally centrifugal, arising from the inferior alveolar artery and periodontal arcades. However, in the edentulous mandible the blood supply is principally centripetal, arising via the subperiosteal plexus of vessels (Fig. 29.8). Watt and MacGregor (1976) liken the circumoral and facial musculature to a curtain draped between the maxilla and mandible. Loss of the anterior dentition results in loss of the “dental bulge” and causes a shortening of the buccinator muscle and consequent distortion of the facial curtain (see Fig. 29.9). The muscles of facial expression decussate to form the modiolus and also intersect directly with the fibers of the orbicularis oris muscle. With tooth loss and reduction of the residual ridge there is hypotonia of the orbicularis oris muscle and the muscles of facial expression. The position of the modiolus changes, being pulled inward and backward, resulting in contraction of the orbicularis oris muscle and distortion of the muscles of facial expression (Figs. 29.9–29.11). The distortion of these muscle groups culminates in an alteration in facial form causing decreased nasolabial and paranasal support, narrowing of the width of the commissure, decreased show of the vermilion margin, loss of labiomental support, decrease in lower face height, and increased prominence of the chin (Fig. 29.11). Awareness of the pattern of resorption of the edentulous jaws and associated soft-tissue changes enables clinicians to anticipate and possibly avert future problems. The successful application of endosteal implants depends on favorable anatomical form and environment, biocompatibility, and favorable biomechanical conditions. The availability of sufficient bulk of bone and a healthy soft-tissue environment are the most important of the many variables that govern the success of endosteal implants. If such conditions do not exist, adjunctive surgical procedures such as osteotomy, bone grafting, and vestibuloplasty should be undertaken. The object of pre-implant surgery is to restore a favorable interarch relationship, creating a healthy environment to allow placement of endosteal implants of maximal size at optimal axial inclination with optimal load distribution and optimal aesthetics. Pre-implant surgery is indicated where there has been atrophy of the jaws, congenital deformity of the jaws, or after bone loss resulting from traumatic avulsion or as a result of tumor ablation. Fig. 29.6 Consequences of jaw atrophy. The attachment of the circumoral and floor-of-mouth musculature delineates the extent of the vestibular and lingual sulci. With continued loss of alveolar bone from class I to class VI these muscles become progressively more superficial.
Introduction
Anatomical Consequences of Jaw Atrophy
Interarch Changes
Muscle Changes
Mucosal Changes
Facial Changes
Pre-implant Surgery
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree