Wide awake hand surgery means no sedation, no tourniquet, and no general anesthesia for hand surgery. The only medications given to the patient are lidocaine with epinephrine. Lidocaine is for anesthesia, and epinephrine provides hemostasis, which deletes the need for a tourniquet. The advantages are: (1) the ability of the comfortable unsedated tourniquet-free patient to perform active movement of the reconstructed structures during surgery so the surgeon can make alterations to the reconstruction before the skin is closed to improve the outcome of many surgeries; and (2) the deletion of all risks, costs, and inconveniences of sedation and general anesthesia.
How do most patients react to being awake during the surgery?
Most people prefer wide awake hand surgery to having work done on their teeth. The pain is similar if not less with the hand surgery, there is no one working in their mouth, and they do not have to look or listen if they do not want to. Those who want nothing to do with the surgery can look away, listen to music with earphones, or watch movies. As there is no tourniquet used, the patients are totally comfortable. Many patients, if not the majority, are interested in seeing what is happening, and those who are interested are allowed to wear a mask and observe.
Surgeons who have never used the technique often remark, “My patients need sedation.” Although some patients are better off asleep or sedated, most prefer the wide awake alternative if it is offered to them in a positive light and if they understand it. After all, most dental procedures are now performed using the wide awake approach, and that is with the surgeon working inside their mouth in which there are airway and communication issues that are not present in hand surgery. Despite these problems, most patients do not want sedation or general anesthesia to have a tooth filled. Patients who have had a wide awake carpal tunnel release feel the same way about their hand surgery.
If patients really need sedation or general anesthesia, it is provided to them. This is in the minority of hand surgery patients, as it is in dental surgery.
Why do most patients prefer wide awake hand surgery once they have been exposed to it?
Most patients prefer wide awake hand surgery for the same reasons they prefer being wide awake when they have a tooth filled. It reduces surgeries like carpal tunnel, trigger finger, operative reduction of fractures, and tendon repairs to the simplicity of going to the dentist. After the surgery, they simply sit up, elevate their totally comfortable hand, and walk out to go home. They never get nausea or vomiting. They get no urinary retention or sedation-induced dizziness. They do not need to get anyone to stay with them or look after them or their children the night of the surgery. They do not have to be admitted to hospital overnight.
They have only 1 visit to the hospital because they do not need to have a second preoperative testing visit. This means that they only need to leave work or get a babysitter one time, the day of the surgery.
They do not need to endure or pay for blood tests, electrocardiography, chest radiography, preoperative medical consultations, anesthesiology fees, or postoperative admissions for the interaction of their medical problems with sedation or general anesthesia.
Many patients do not like to leave control of their faculties to sedation or general anesthesia they do not need to have.
They get to speak to their surgeon during the surgery. The surgeon can answer their questions and educate them on good postoperative care and activity as well as return-to-work instructions. They can establish a verbal relationship with the surgeon outside the preoperative consultation.
Why do most patients prefer wide awake hand surgery once they have been exposed to it?
Most patients prefer wide awake hand surgery for the same reasons they prefer being wide awake when they have a tooth filled. It reduces surgeries like carpal tunnel, trigger finger, operative reduction of fractures, and tendon repairs to the simplicity of going to the dentist. After the surgery, they simply sit up, elevate their totally comfortable hand, and walk out to go home. They never get nausea or vomiting. They get no urinary retention or sedation-induced dizziness. They do not need to get anyone to stay with them or look after them or their children the night of the surgery. They do not have to be admitted to hospital overnight.
They have only 1 visit to the hospital because they do not need to have a second preoperative testing visit. This means that they only need to leave work or get a babysitter one time, the day of the surgery.
They do not need to endure or pay for blood tests, electrocardiography, chest radiography, preoperative medical consultations, anesthesiology fees, or postoperative admissions for the interaction of their medical problems with sedation or general anesthesia.
Many patients do not like to leave control of their faculties to sedation or general anesthesia they do not need to have.
They get to speak to their surgeon during the surgery. The surgeon can answer their questions and educate them on good postoperative care and activity as well as return-to-work instructions. They can establish a verbal relationship with the surgeon outside the preoperative consultation.
Why do surgeons who have used this approach like it?
The surgeons no longer have to wait for an anesthesiologist to do a hand surgery case. The surgery no longer has to be done in the main operating room because all the monitoring required for sedation or general anesthesia is not required. The only 2 medications that are given to the patient are lidocaine and epinephrine, which have now been given to millions of patients in dental offices without monitoring with ultimate safety for more than 60 years. Hand surgery in the office or clinic is more efficient and convenient for the surgeon. Efficiency is increased because of minimal turnover time. Surgeons no longer have to admit and look after patients who underwent hand surgery with medical problems aggravated by sedation or general anesthesia postoperatively.
The initial impetus for the widespread use of wide awake hand surgery in Canada was the difficulty surgeons had in getting hand surgery into the main operating room with an anesthesiologist. The approach is now preferred in many surgeries because watching patients actively move reconstructed parts during the surgery has improved outcomes.
Epinephrine in the finger for hemostasis deletes the tourniquet requirement
There was a myth that epinephrine should never be injected into the fingers, nose, ears, and toes. It was based on the theoretical risk that epinephrine caused infarction in body parts with end arteries. The myth originated between 1920 and 1945 and was cemented with the writing of the first American textbook on hand surgery by Stirling Bunnell in 1945. This myth has been clearly shown to be not valid by the following 4 seminal papers and several others.
The first of the 4 papers was published in 2007 and traces the root of the epinephrine myth to its true source, procaine. There are 48 cases of finger infarction with local anesthetics in the world literature; almost all of them were before 1950. Twenty-one of those were with epinephrine mixed almost exclusively with procaine. Twenty-seven of those were with procaine without epinephrine. More fingers died with procaine without epinephrine than with procaine with epinephrine. Procaine was the first synthetic local anesthetic and replaced injected cocaine in 1903. It was the new caine, hence the term Novocaine. It was the only widely used local anesthetic agent until lidocaine became available in 1948. Procaine was quite acidic with a maximum stability pH of 3.6, less than the physiologic pH of 7.4. It became more acidic as it sat on the shelf. Yellowish procaine that had been on the shelf for some time was injected into patients in the 1940s, as the first law requiring expiration dates was passed in 1979 by the US Food and Drug Administration (FDA). In 1948, the US FDA issued a warning about toxic batches of acidic procaine (Novocaine) that had induced tissue necrosis. One batch had a pH as low as 1, which is extremely acidic. Clearly, aged acidic procaine was responsible for tissue death before 1950 and likely was the cause of the death of the fingers attributed to epinephrine. There is not 1 case of finger death caused by lidocaine with epinephrine in the world literature.
The second paper that ended the epinephrine myth was written in 2003. This paper showed that epinephrine-induced vasoconstriction could be reliably reversed in the human finger with the injection of the α-antagonist phentolamine (available since 1957 ). This study was performed by the Dalhousie University alumni plastic hand surgeon volunteers. If 1 mg of phentolamine in 1 cc of saline is injected wherever epinephrine is injected, the vasoconstrictive effect of 1:100,000 epinephrine is reliably reversed in the human finger in an average of 85 minutes.
The third paper was a 2-year prospective consecutive clinical series of 3110 surgeries in the fingers and hand with elective epinephrine injection published in 2005. In this 6-city, 9-surgeon study, there were no cases of digital infarction and phentolamine rescue was never required.
The fourth paper was a review of all 59 cases of accidental high-dose (1:1000) epinephrine injection in the finger in the world literature. There was not 1 case of finger death even though only 13 patients were treated with phentolamine. If 1:1000 epinephrine has yet to be reported to kill a finger, it is unlikely that 1:100,000 ever will, especially with the availability of the phentolamine antidote.
Epinephrine in the fingers and hand deletes the need for tourniquet, which deletes the need for sedation, Bier block, brachial plexus block, or general anesthesia. Patients with sedation, general anesthesia, or motor nerve block are mostly unable to cooperatively, comfortably, and reliably move the reconstructed hand and finger structures during the surgery in most cases.
Contraindications to epinephrine in the finger
If a fingertip is nice and pink before a surgery, it will be nice and pink after the surgery unless the surgeon damages the blood supply to the skin during the surgery. However, if a finger is dusky or blue before the surgery, it may be wise not to use epinephrine.
A surgeon probably should not inject epinephrine in the finger if he does not know about phentolamine, the antidote to epinephrine-induced vasoconstriction. This would be similar to a surgeon who injects morphine when he does not know about naloxone. All that the surgeon needs to know about phentolamine is that 1 mg of the antidote in 1 cc of saline will reliably reverse epinephrine-induced vasoconstriction, as described previously.
How to inject lidocaine and epinephrine for the hand and finger surgery
The tumescent concept is used. The goal is to get the lidocaine and epinephrine molecules wherever there is likely to be any incision or dissection. Injection of low concentration with large volume is preferred to high concentration of anesthetic agents in nerve blocks. To stay less than 7 mg/kg of lidocaine with epinephrine, the dosage shown in Table 1 is used.
| Volume Required to Tumesce the Area of Dissection | Concentration of Lidocaine and Epinephrine |
|---|---|
| Less than 50 cc | 1% lidocaine with 1:100,000 epinephrine |
| Between 50 and 100 cc | 1/2% lidocaine with 1:200,000 epinephrine |
| Between 100 and 200 cc | 1/4% lidocaine with 1:400,000 epinephrine |
The local anesthesia can be injected rapidly (painfully) with a 25-gauge needle, as the author did in the first 22 years of his practice, or slowly with a 27-gauge needle and bicarbonate to provide an almost pain-free experience as described in the hole-in-one local anesthetic technique, which means that all that the patient feels for pain is the first poke of the first injection. The last 2 references clearly explain with text and film how to inject a local anesthetic in an almost pain-free fashion.
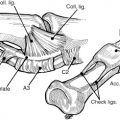
A large volume is injected in the most proximal location that any dissection is likely to take place to block the nerves distally. For example, for a zone 1 flexor tendon repair in the hand in which the dissection may reach into the palm, 10 cc would be injected at the most proximal of likely incisions as shown in Fig. 1 to block the distal nerves (see Fig. 1 ). After waiting 15 to 30 minutes to allow for distal anesthesia to set in, the distal parts of the palm and finger are injected for the epinephrine-induced vasoconstriction effect in a pain-free fashion as described in Fig. 2 . The same technique would be used for the Dupuytren palmar fasciectomy.

Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree