10 Radiologic Studies of the Lower Urinary Tract and Pelvic Floor
Pelvic floor disorders include a broad array of interrelated clinical conditions that include urinary incontinence, pelvic organ prolapse, fecal incontinence, sensory and emptying abnormalities of the lower urinary tract, and defecatory dysfunction. A thorough evaluation, including physical examination, urodynamic and electrophysiologic investigations, and imaging studies of the lower urinary tract and pelvic floor as indicated, is crucial for understanding anatomy and function. Results of this evaluation can then guide the clinician to the appropriate management of bothersome symptoms.
INTRAVENOUS AND RETROGRADE PYELOGRAPHY
Despite the emergence of newer imaging techniques, IVP is still frequently used to evaluate the urinary tract (Fig. 10-1). IVP is safe, inexpensive, and widely available, and it provides information about the anatomy of the collecting system and functional status of the glomerular filtration apparatus. Computed tomographic (CT) IVP is gradually replacing conventional IVP because it gives more precise information about renal anatomy and function. One of the most common indications for performing an IVP in urogynecology is to detect possible ureteral obstruction caused by gynecologic cancer, pelvic mass, pelvic organ prolapse, or after gynecologic surgery. IVP, with delayed films and tomography, is also useful to help diagnose certain uncommon conditions, such as ectopic ureter and ureterovaginal fistula. Although IVP is safe, it is an invasive procedure and exposes patients to injection of iodine dye and to radiation; it is contraindicated in pregnant women or those with allergy to iodinated contrast media, renal insufficiency, and congestive heart failure. Because of these disadvantages, abdominal and Doppler ultrasounds have been used as a noninvasive and less expensive alternative to diagnose ureteral obstruction.
If the pelvicaliceal or ureteric anatomy is not adequately visualized with IVP, or if there is a contraindication to IVP, an alternative approach is to perform a retrograde pyelogram, which is especially useful if there is a coexisting indication for cystoscopy. In retrograde pyelogram, the contrast medium is injected into the upper urinary tract through a cone-tipped catheter placed at cystoscopy under fluoroscopic guidance (Fig. 10-2). This approach is associated with a higher infection rate than antegrade pyelography and may be contraindicated in women with known allergic reaction to contrast media or very recent lower urinary tract trauma or surgery. The large amount of contrast medium injected and the pressure applied during retrograde pyelogram may result in anastomotic leak and extravasation, with systemic absorption of the contrast.
CYSTOGRAPHY
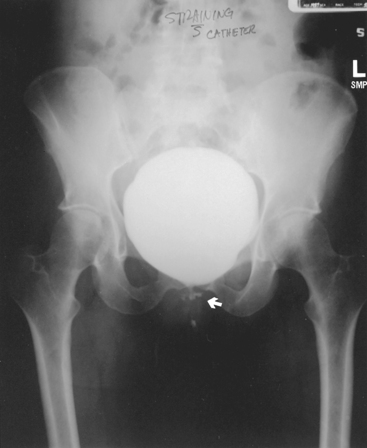
Cystography is frequently performed to detect bladder injury after trauma, to diagnose fistulas between the bladder and the adjacent organs, and to confirm that a cystotomy or bladder fistula has healed after surgical repair. Vesicovaginal, vesicouterine, and vesicoenteric fistulas are diagnosed when contrast material from the bladder enters and opacifies the adjacent viscera (Fig. 10-3). Absence of contrast in the adjacent viscera does not always exclude a fistula because the connecting tract may not be large enough to allow passage of a sufficient quantity of contrast to be seen radiographically.
To determine whether a cystotomy or fistula repair has healed, the bladder is filled slowly with contrast medium and then drained. A postvoid film is obtained to evaluate for extravasated contrast medium. Contrast from extraperitoneal leakage usually forms an irregularly shaped mass around the defect and remains there for a relatively long time. Contrast that has leaked from an intraperitoneal defect diffuses into the abdominal cavity and is rapidly absorbed through the peritoneal cavity.
VOIDING CYSTOURETHROGRAPHY
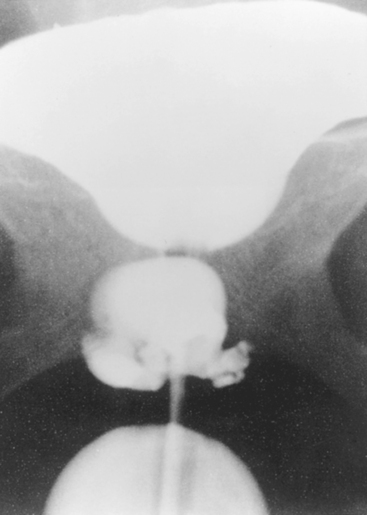
Voiding cystourethrogram (VCUG) is a dynamic radiologic study that is used to diagnose structural bladder and urethral abnormalities with voiding and to evaluate for vesicoureteral reflux. VCUG is also used to investigate suspected bladder fistula or suburethral diverticula (Fig. 10-4) and to evaluate the integrity of the bladder or urethra after fistula or diverticula surgery. Because of recent advances, ultrasound and magnetic resonance imaging (MRI) technology have replaced VCUG as the primary imaging modality in diagnosing many of these conditions.
POSITIVE-PRESSURE URETHROGRAPHY
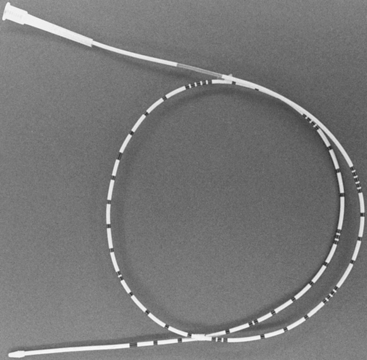
Positive-pressure urethrography was first described and used by Davis and Cian in 1956 to evaluate the female urethra. Today, the primary indication for this diagnostic test is to search for possible suburethral diverticula not visualized on VCUG. The study requires a Tratner catheter, which has two balloons, with an opening in the lumen of the catheter between the two balloons for contrast injections. The distal balloon is placed into the bladder, and the proximal (sliding) balloon is positioned just outside the external urethral meatus. The two inflated balloons create a temporary, closed system and allow the contrast injected into the urethra to opacify the diverticulum (Fig. 10-5). This radiologic test is often performed in conjunction with VCUG to maximize the diagnostic accuracy. It can also be used during surgery to help expand and identify urethral diverticula and to test the integrity of repairs after resection.
ULTRASOUND
Basic Procedure of Perineal Ultrasound
The information that should be obtained during ultrasonographic evaluation of the female lower urinary tract is shown in Box 10-1. Some disagreement exists regarding the optimal orientation of images. Some authors prefer an orientation as in conventional transvaginal ultrasound. However, others recommend showing superior structures above, inferior structures below, anterior structures on the right, and posterior structures on the left.
The examination can be performed in dorsal lithotomy, semireclining, or standing position. No significant differences are present in the dynamic assessment of the bladder neck between the semireclining and the standing positions. The ultrasonographic evaluation of the lower urinary tract begins with the midsagittal plane. This results in an image including the symphysis pubis, urethra, bladder neck, vagina, cervix, rectum, and anal canal (Fig. 10-6). By moving the transducer to the left or to the right, periurethral structures can be assessed. The pressure exerted by the transducer should be kept low but still sufficient to obtain good images with high resolution. The presence of a full rectum may impair diagnostic accuracy and sometimes necessitates a repeat assessment after defecation.
The bladder volume should be fixed on examination: 300 mL for the evaluation of dynamic changes of the bladder neck and less than 50 mL for the assessment of bladder wall thickness. The bladder volume can be estimated by either a transabdominal or transvaginal approach, although the accuracy is not reliable for bladder volumes less than 50 mL. In the transabdominal approach, three parameters, including height (H), depth (D), and width (W), are obtained from two perpendicular planes (sagittal and transverse). In sagittal scanning, height and depth correspond to the greatest superior-inferior measurement and the greatest anterior-posterior measurement, respectively. Thus, the bladder volume can be calculated from the formula: bladder volume (mL) = H × D × W × 0.7. The value of 0.7 is a correction factor for the nonspherical shape of a full bladder. The approximate error rate of the formula is 21%. Transvaginal ultrasound has also been recommended to measure bladder volumes in the range of 20 to 300 mL. Horizontal height and vertical depth are obtained in the sagittal scanning. The bladder volume can be estimated according to the formula: bladder volume (mL) = H × D × 5.9 − 14.6 (95% confidence limits around ± 37 mL).
Normal Images of the Female Lower Urinary Tract
When the scan is deviated a little to the right or left parasagittal plane, two tiny nodules (ureter papilla), located at the junction of the trigone and bladder, can be visualized with peristalsis. The position of the ureteral orifices can be identified by urinary flow from each ureteral orifice (ureter jet phenomenon) displayed on color and power Doppler scanning. The urethra is a tubular structure with a central echolucent area and surrounding echogenic sphincters. Color and power Doppler ultrasonography can reveal blood supply signals within and around the urethra, whereas scant vascular signals are noted in the bladder wall. Less bladder neck hypermobility and funneling are noted in normal continent women than in women with stress urinary incontinence and pelvic organ prolapse. The normal range of bladder neck motion has not been defined, and a wide range of overlap is present between normal and abnormal values. In addition, the measurements of bladder neck position have been reported to be influenced by bladder filling, patient position, and catheterization. By the introital approach, Yang and Huang (2002) reported that in healthy continent women, the angles between bladder neck and midline of symphysis pubis are 81 ± 15 degrees at rest and 113 ± 27 degrees during straining, with the rotational angle of 30 ± 20 degrees; the distances between bladder neck and midline of symphysis pubis are 25.7 ± 4.9 mm at rest and 22.9 ± 3.3 mm during straining. Bader et al. (1995) reported that in women without stress incontinence and prolapse, the posterior urethrovesical angle is 97 degrees at rest and 108 degrees during stress.
Applications in Female Lower Urinary Symptoms and Conditions
ULTRASONOGRAPHIC CHARACTERISTICS OF UROLOGIC AND PELVIC FLOOR DISORDERS (BOX 10-2)
Cystitis.
Calculi.
Sonography can detect some, but not all, distal ureteral calculi or bladder stones. The sonographic characteristics of a distal ureteral calculus include unilateral dilation of the ureter, which is normally invisible, and presence of a hyperechogenic stone within the ureter accompanied by strong acoustic shadow and surrounding edematous tissue. Bladder calculi account for 5% of urolithiasis cases and usually occur as a result of foreign objects, obstruction, or infection. In situations of bladder calculi secondary to a suture from a bladder neck suspension, hyperechoic suture material and bladder stone sometimes can be clearly demonstrated on ultrasonography, whereas radiography and cystoscopy may fail to identify the underlying pathogenesis of the stone.
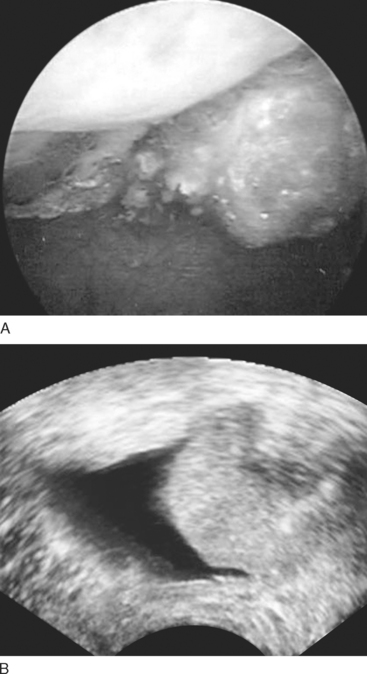
Bladder Wall Thickening or Tumors.
Ultrasonography is also a useful diagnostic modality for screening and detecting bladder tumors. On ultrasonography, the bladder tumors can have polypoid, sessile, or plaque-like shapes, with regular or irregular surface, with or without calcified foci (Fig. 10-7). Color and power Doppler ultrasonography may demonstrate neovascularization within the tumor, with a low resistance index of the tumor vessels.