CHAPTER 2 Radiologic Evaluation of Hip Arthroplasty
ARTHROPLASTY
The high prevalence of hip pathology and the broad success of hip replacement surgery have resulted in hip arthroplasty becoming a routine procedure, with an estimated 170,000 primary hip arthroplasties performed annually in the United States and approximately 35,000 revision surgeries performed as revision surgery.1 Although the types of prostheses continuously evolve, hip prostheses may be divided simply into unipolar, bipolar, and total arthroplasties, with the last divided further by bearing surface (metal on polyethylene, metal on metal, ceramic on ceramic, and ceramic on polyethylene). The specific type of prosthesis, surgical technique, and surgeon-related and patient-related factors play a role in the relative frequency with which complications occur.
LOOSENING
Aseptic (or mechanical) loosening is the most common cause for revision arthroplasty2 above osteolysis (“particle disease”) and infection (septic loosening). Aseptic loosening is often a diagnosis of exclusion, when studies for the cause of loosening are notably negative for infection, and the radiologic findings are not typical for osteolysis.
With respect to loosening, it is unrealistic to rely on simple radiographic observation to have the desired precision of detecting submillimeter motion. This is of significance particularly within the first 2 years after replacement when early motion is associated with a generally poor outcome. Precise measurement is now possible with the use of template matching algorithms3; this is improved further with the use of bone marking and stereometry.4 Despite these advanced methods, knowledge of the more familiar radiographic manifestations of loosening as assessed on observation is important because the above-mentioned technology is not universally available.
An alteration in the position of components compared with prior radiographs is unequivocally diagnostic of loosening. Motion noted on stress views is also diagnostic. On stress views obtained with CT, a difference in femoral component version of greater than 2 degrees is diagnostic compared with views obtained with maximal external and internal rotation.5
Criteria for the diagnosis of prosthetic loosening largely depend on whether cement has been used to secure the prosthesis. In the cemented prosthesis, simply measuring the size of the cement-bone interface provides a reproducible and standard method of assessing whether loosening has occurred. Regardless of the etiology, loosening of a cemented prosthesis manifests as an increase in periprosthetic lucency at the bone-cement interface of 2 mm or more. Progression of lucency (even if <2 mm), fracture of cement, and migration of components also are consistent with loosening.6 In the setting of revision arthroplasty, lucency greater than 2 mm is permissible; however, in this instance, reference should be made to the early postrevision radiographs.
The flange of the femoral stem ideally should sit flush with the cut surface of the femoral shaft. Movement occurring inferior to this level, or subsidence, is consistent with femoral prosthesis loosening. Lucency adjacent to the femoral stem should be described with reference made to the standardized Gruen zones (Fig. 2-1).7
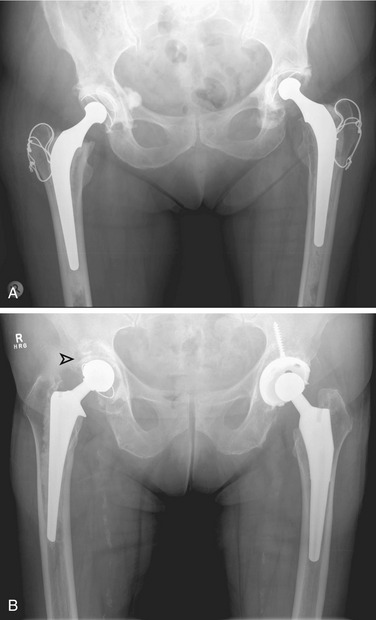
Insertion of a femoral component results in the well-known localized form of disuse osteopenia known as “stress shielding,” a phenomenon occurring secondary to the bypassing of mechanical forces. When this phenomenon is linked to the part of the prosthesis that is porous coated, in most instances, only proximal loss occurs8; however, in a proportion of cases, loss of periprosthetic bone density along the entire femoral stem may result in loosening (Fig. 2-2). In these circumstances, the osteopenia is typically more prominent laterally along the femoral stem (Fig. 2-3) and in the retroacetabular region, the latter best appreciated with CT.9 Stress shielding may predispose to periprosthetic fracture, usually at the tip of the femoral stem (Fig. 2-4), and more rarely to component fracture. A distal femoral cement restrictor plug may be used in order to form a seal that prevents distal cement migration so that adequate contact with the prosthesis may be optimized. Often, a small focus of entrapped gas can be visualized; this finding should not be a consequence of infection.
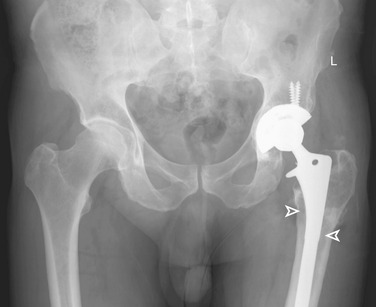
Although loosening of the femoral component may be simply evaluated on the standard AP and lateral views of a hip radiographic series, radiographic assessment of the acetabulum is more difficult because of its shape. Criteria for diagnosis of loosening in an uncemented acetabular component are different than for cemented components; the most predictive radiographic findings for early diagnosis of loosening of a hemispheric porous-coated cup are progression of radiolucent lines more than 2 years after the operation and any new radiolucent line of 1 mm or wider that appears more than 2 years postoperatively. Radiolucent lines in all three zones (even if they are not continuous), radiolucent lines 2 mm or wider in any zone, and migration are also considered to be criteria for the diagnosis of loosening (Fig. 2-5). Sequential AP and lateral radiographs are necessary to assess the time of onset and progression of radiolucent lines in order to identify loose hemispheric porous-coated cups accurately.10 The sensitivity and specificity of these findings are 94% and 100%. Often, the subtle findings of lucency are not detected early and so the radiographic diagnosis of loosening is only made when component malalignment or migration has occurred, typically medially or superiorly or both.11,12
The inclination of the acetabulum is an important and simple measurement; inclination is the angle of tilt that the acetabular component makes with the horizontal. Despite patient positioning, a horizontal line forms a standard reference and is drawn connecting the inferior-most aspect of both ischial tuberosities (the bi-ischial line) or both tear drops (the bi–tear drop line). Ideally, this angle should approximate 45 degrees (range 35 to 55 degrees), with an alteration in the inclination angle of greater than 4 degrees or movement greater than 4 mm compatible with loosening.13 A line drawn from the Köhler line (ilioischial line) to either the acetabular margin or the femoral head is used to exclude medial migration on subsequent evaluation. Any form of protrusion or intrapelvic migration also is consistent with acetabular component loosening.14
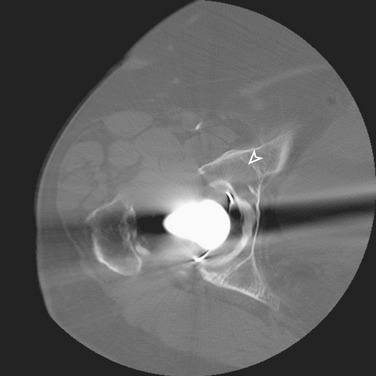
Multidetector CT, with its ability to reduce beam hardening artifacts (a significant limitation of conventional helical CT) has a higher sensitivity for the detection of periacetabular lucency (Fig. 2-6) and a higher rate for diagnosing early component loosening.15 Although the expense and high radiation dose limit the utility of CT as a routine investigation to detect acetabular loosening, this modality may be used when radiographic assessment is equivocal, or clinical suspicion for loosening is high when the radiographs are negative.15
CT allows for highly accurate measurement of cup orientation despite the degree of patient pelvic tilt and rotation.16,17 Although acetabular anteversion may be roughly estimated on a lateral radiograph, this technique has poor reliability and lacks the high degree of precision required to assess component migration accurately. Lateral radiographs in particular are affected by variation in patient positioning and are too imprecise when an exact measurement is required.18 Anteversion may be measured with great accuracy on CT by drawing a line tangential to the opening of the acetabulum and then measuring it compared with the AP plane. Anatomic derivation of the AP plane is made by accurately drawing a true horizontal line, which may vary depending on patient positioning. A line drawn along the posterior aspect of the posterior columns serves as the basis from which a line in the AP plane is drawn perpendicular. The intersection made with the line drawn tangential to the acetabulum defines the degree of acetabular version.19
CT has the additional advantage of accurately assessing further parameters of acetabular geometry, specifically, the acetabular depth, and degree of anterior and posterior wall cover.20,21 These measurements are of particular use in preoperative planning for revision arthroplasty.22 The quality of screw fixation23 and the degree and quality of osseointegration of bone substitutes24 also can be assessed. The quality and degree of bone stock25 may be assessed on CT; dual-energy x-ray absorptiometry scanning26 is an alternative imaging modality. Finally, CT-guided obturator nerve block may be used for control of chronic, recalcitrant hip pain. It is an optional treatment modality especially for patients unsuitable for surgery.27,28
Several arthrographic techniques have been described in the diagnosis of prosthetic loosening. After successful needle placement into the prosthetic hip, these techniques rely on the principle of showing the presence of contrast material below the level of the intertrochanteric line interposed between the bone-cement interfaces. In its simplest form, standard fluoroscopic demonstration of contrast material may be used; however, digital subtraction techniques are superior.29,30 Contrast material insinuating between the bone-cement interfaces when diagnosing loosening may be more apparent after ambulation.31 High-pressure techniques have decreased the false-positive rate of this technique; however, a false negative result may occur when adhesions or fibrous tissue formations limit the spread of contrast material. A negative result still may be obtained despite the presence of loosening because of the inability to achieve adequate high pressures and distention in a patient with a lax pseudocapsule or communicating bursae. The sensitivity and specificity of the test may reach 100% with the addition of the less viscous radiotracer sulfur colloid.32–34 Overall, arthrography tends to have a lower accuracy for acetabular component loosening.35
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree