Radial Forearm Flap for Nasal Lining Reconstruction
Robert L. Walton
Brenton R. Robinson
DEFINITION
Since its initial description by Yang et al. in 1978,1 the radial forearm flap has been considered to be one of the most versatile flaps for nasal defect reconstruction.
It provides for thin, well-vascularized tissue that is easily harvested, with acceptable donor-site morbidity.
Unique to the radial forearm free flap (RFFF) is its ability to be partitioned into separate islands for restoration of specific nasal lining elements such as the nasal vestibule, floor, and columella.2
The free radial forearm flap is properly defined as a fasciocutaneous flap that is primarily based on the radial artery and its venae comitantes (VCs).
One or two of the cutaneous nerve branches of the forearm (ulnar, median, or lateral cutaneous nerves of the forearm) provide for sensibility of the flap if a neurosensory configuration is required.3
The size of the flap can encompass any section of the skin and fascia from the crease of the volar wrist to the antecubital fossa including the circumferential forearm.
ANATOMY
Vascular Anatomy
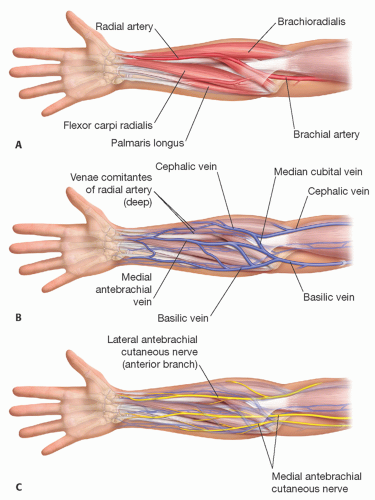
The vascular anatomy of the radial forearm flap has been well elucidated.4 As noted above, circulatory flow is provided by the radial artery and its associated VCs (FIG 1A). The basilic and cephalic veins of the forearm are usually included in large configurations of the flap, although the VCs provide for its primary venous drainage.4 Its long vascular pedicle (8-12 cm) and generally consistent anatomy make the radial forearm flap particularly advantageous for nasal reconstruction.
Radial Artery
The radial artery originates just distal to the bicipital aponeurosis where the brachial artery divides into the radial and ulnar arteries. In the proximal forearm, the radial artery lies beneath the brachioradialis muscle and becomes more superficial as it approaches the hand. The radial artery travels between the heads of the first dorsal interosseous muscle to create the deep palmar arch providing blood to the thumb and thenar side of the index finger. As the radial artery becomes more superficial in the distal forearm, it gives off small fasciocutaneous perforators that course superficially to supply the overlying fascia and skin. These fasciocutaneous perforators constitute the primary perfusion of the radial forearm skin.4 Saint Cyr et al. found an average of 24.6 radial artery perforators in the forearm, with the majority located distally and over 50% of these having a radial orientation.4 The presence of these two main clusters found along the distal and proximal thirds of the radial artery can significantly facilitate flap planning and harvest.4
Although variations in radial artery anatomy are rare, its collateral communications with the ulnar circulation in the hand should be confirmed preoperatively by an Allen test at the wrist. In the most common configuration of the deep palmar arch (Type A), it is formed by the anastomosis between the deep volar branch of the radial artery and the deep inferior branch of the ulnar artery.5 The superficial palmar arch (type A) is formed by anastomosis between the superficial volar branch of the radial artery and the continuation of the ulnar artery.5
The RFFF has two systems of venous drainage: a deep system composed of two VCs accompanying the radial artery and a superficial system composed of the cephalic vein and a series of subcutaneous veins (17). The profunda cubitalis vein serves as the primary connection point between the two systems (FIG 1B).6 The superficial system is based off the cephalic vein and a series of meandering, subcutaneous venules that drain into it.7 The superficial venous drainage is generally considered to have a consistent course and a favorable caliber for subsequent anastomosis ranging from 3 to 6 mm.6 The cephalic vein courses around the radial border of the forearm ascending along the ventral aspect of the forearm toward the antecubital fossa, where it joins the basilic vein. The cephalic vein drains the radial portion of the dorsum of the hand. Deep venous drainage occurs with the paired deep VCs that travel along each side of the radial artery with communicating tributaries. The VCs send off paired branches at each ramification of the radial artery, reproducing a triplicate pattern of vessels.7
Although widely studied, the controversy of one vs two venous anastomoses still exists.8 Even though the published success rates of RFFF approach 95%, a series of complicating factors still can lead to unpredictable venous compromise postoperatively.8 In a retrospective cohort study of 370 radial forearm free flaps, Selber et al. conducted a comparative analysis of the deep vs the superficial drainage systems. They found that problems of inadequate outflow are more commonly encountered when the cephalic vein is used to drain the flap. When of adequate caliber (greater than 1 mm), they advocate using the VCs as the sole venous outflow for the flap.7
As noted by Gottlieb et al., the VCs coalesce into a single vein at the level of the brachial artery bifurcation. The profundus cubitalis vein (vena anastomotica) connects the
coalesced VCs to the cephalic vein at the level of the cubital fossa.9 By dissecting the cephalic vein proximal to this point of coalescence, both the deep and superficial venous systems can be drained via one large anastomosis. Advantages of this technique include improved venous drainage of very large radial forearm flaps, rendering the venous anastomosis technically easier, due to its larger size, and more available versatility in designing the venous portion of the vascular pedicle where the deep and superficial systems join in the proximal forearm allowing for single outflow vessel anastomosis.9 As noted, this configuration is reserved for large flaps that wrap the radial forearm distally and extend the greater length of the forearm to the wrist.
Nerve Supply
The medial and lateral antebrachial cutaneous nerves of the forearm provide for cutaneous sensibility of the radial and volar forearm (FIG 1C). The lateral antebrachial cutaneous nerve is a continuation of the musculocutaneous nerve originating from C5 to C7 nerve roots and the lateral cord of the brachial plexus, and it innervates the greatest surface area of the flap’s three overlapping nerve territories.9 The nerve arises between the biceps brachii and the brachialis muscles. It pierces the fascia radial to the biceps tendon in the cubital fossa, passes posterior to the cephalic vein, and divides into anterior and posterior branches. The larger anterior branch accompanies the cephalic vein into the forearm and supplies the skin of the radial half of the anterior surface as far as the thenar eminence. The smaller posterior branch supplies the skin of the radial border and posterior aspect of the forearm as far as the wrist. The medial antebrachial cutaneous nerve arises from C8 to T1 nerve roots. At the junction of the middle and distal thirds of the forearm, the nerve emerges from the brachial fascia running with the basilic vein and dividing into an anterior and ulnar branch. The anterior branch supplies the anterior medial surface of the forearm to the wrist; the ulnar branch passes anterior to the medial epicondyle and supplies the skin on the forearm on its posteromedial surface.
An important attribute of the RFFF is its ability to provide restoration of sensibility in reconstruction as a neurosensory fasciocutaneous flap. Studies determining the long-term recovery of sensibility in flaps have shown increased sensibility and better functional results with reinnervated flaps compared to noninnervated flaps.10 The lateral antebrachial cutaneous nerve is the dominant nerve of the radial forearm flap, providing sensibility to over 62% of the potential flap area. It is most commonly employed for restoring sensibility in neurosensory configurations of the flap.10
Of special note is the superficial branch of the radial nerve (SBRN), the branches of which are commonly encountered during elevation of the radial edge of the flap (FIG 1C). These branches are highly vulnerable to injury during flap elevation necessitating diligent care during this portion of the dissection. The SBRN courses under the brachioradialis and between the heads of the extensor carpi radialis longus just proximal to the radial styloid process.11 When raising the flap, it is important to note the close relationship between the cephalic vein and SBRN. If harvest of the cephalic vein is undertaken by the surgeon during formation of the flap, an awareness of the precise anatomical location of the SBRN in relationship to both the radial artery and cephalic vein is essential to avoid neurologic injury.11 Flap donor-site morbidity arising from injury to the SBRN has been documented by Grinsell and Thiele (2005) to be between 9% and 18% depending on whether the VCs or cephalic vein were included in the elevation, as raising the cephalic vein doubled the risk of SBRN injury.12
PATIENT HISTORY AND PHYSICAL FINDINGS
If an Allen test is positive but concern still exists on the patency of the radial artery, it is reasonable to obtain upper extremity arteriography for further evaluation.
In a cadaver dissection of 650 cadaver arms, only 3.2% had no communication between the radial and ulnar artery, and 3% had an incomplete deep arch.13
If both of these variations are present, the thumb will be dependent on the radial artery (approximately 1 in 1100).13 Vein graft reconstruction would be necessary in these cases.
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree