Fig. 10.1
Photograph of a patient with a radiation-induced deformity of the tissue expander after immediate breast reconstruction

Fig. 10.2
Photograph taken after completion of radiotherapy showing capsular contracture of the permanent implant of the right breast
The rate of complications and unfavorable aesthetic results ranges from 3 % to 40 % in the absence of RT [39] and might rise to 17–80 % by adding RT [40]. Tallet et al. [27] reported a three times higher complication rate (14 % vs 51 %) and prosthesis loss rate (9 % vs 24 %), when RT was applied, whereas a sixfold higher odds of complications with an odds ratio of 6.4 (95 % confidence interval, 1.6–25.0) was observed in the Michigan Breast Reconstruction Outcomes prospective study [41]. In that series, the use of RT was significantly associated with breast reconstruction failure, and complications occurred in 68 % of the irradiated group compared with 31 % of the nonirradiated group (p = 0.006).
The overall complication rate in the irradiated group was 52.5 %, 32.5% of which were capsular contractures, as compared with 10 % in a nonirradiated control group in a study including 40 patients [14]. Ascherman et al. [15] reported on 27 patients reconstructed with TE/PI, where the irradiated group had a higher overall complication rate compared with a control group (40.7 % vs 16.7 %), requiring a more frequent removal of the implant (18.5 % vs 4.2 %). In the study by Drucker-Zertuche et al. [42], the irradiated group, with a greater complication rate (45.9 % vs 11.6 %), also had a higher percentage (54 %) of major or minor correction surgical procedures as compared with the nonirradiated group (5 %) and had a greater breast reconstruction failure rate (16.2 % vs 0 %).
Despite the fact that RT increases the rate of complications, TE/PI remains for many investigators an acceptable option for reconstruction. The group from the Memorial Sloan–Kettering Cancer Center continues to use immediate breast reconstruction with TE/PI for women who are not ideal candidates for autologous tissue reconstruction [39], despite finding in their series 68 % of patients had capsular contractions after RT, which was significantly higher than for nonirradiated patients (40 %, p = 0.025). Complications aside, the overall success rate for implant breast reconstruction was 90 % among irradiated patients compared with 99 % among nonirradiated patients and 80 % of the irradiated women demonstrated acceptable aesthetic results versus 88 % of the nonirradiated women. Hazard et al. [6] reached the same conclusions in a small retrospective study, with an acceptable rate of capsular contraction and good or excellent cosmetic outcomes in 85 % of cases. Modern RT with the alternate use of customized-bolus RT and intensity-modulated RT (IMRT) in one-third of cases allows the achievement of a very low incidence of complications as observed in the series conducted by Anderson et al. [35], which might be promising for future studies.
The combined use of an autologous flap and an implant did not prevent higher complication rates when breast reconstruction was performed before PMRT (67 %) as compared with PMRT being administered first (30 %), which was of borderline significance (p = 0.093) [16]. However, immediate breast reconstruction with an implant in conjunction with a flap shows a rate of capsular contracture which is threefold lower than that with an implant alone (6.8 % vs 25 %) [25]. With regard to patients who have previously undergone PMRT, breast reconstruction with TE/PI alone is considered a relative contraindication because of the risk of bone deformity and rib fractures [43]. However in a selected group of women who did not develop severe skin changes nor induration with initial PMRT, delayed TE/PI reconstructions have been considered as an option, as shown in one study [44].
10.4.2 Autologous Reconstruction
The two most commonly used autologous tissue flaps for breast reconstruction are the LD and TRAM flaps. Recent studies have reported on the use of the DIEP flap, whereas with regard to the superficial inferior epigastric artery flap and other flaps based on gluteal and thigh regions, the ability to withstand RT is still unknown. The free flap version of the TRAM flap appears to be more resistant to RT changes than a pedicled TRAM flap because of the different blood supply [45]. However, the fewer complications and flap losses after irradiation of free TRAM flaps as compared with pedicled TRAM flaps observed in several studies are not confirmed by others [46].
The commonest complications after autologous breast reconstruction are fat necrosis, flap and mastectomy skin loss, fibrosis, and contracture. Even in the absence of RT, complication rates range from 5 % to 41 % [11, 47]. The addition of RT increases this incidence and current literature reports complication rates in the range from 7 % to 87.5 % [18, 48, 49]. Complications occur irrespective of whether an immediate or delayed breast reconstruction is performed [50], but a trend toward an increase in complications (overall aesthetic appearance, symmetry, flap contracture and hyperpigmentation) was evident for immediate breast reconstruction and PMRT [51].
The TRAM flap is one of the most commonly studied flaps in the literature for breast reconstruction. When the need for PMRT is unknown at the time of surgery, the TRAM flap [52] is a good option to provide good tolerance and aesthetically acceptable results (Fig. 10.3). Apart from fat necrosis, a recent study from Emory University did not find any difference either in the complication rate or in the need for revision surgery among patients with immediate breast reconstruction alone as compared with patients receiving PMRT, although cosmesis was worse [49]. On the other hand, studies from the MD Anderson Cancer Center [24, 59] indicate that RT after autologous breast reconstruction clearly increased morbidity and worsened the cosmetic results, supporting the delay of breast reconstruction until after RT. No flap loss was reported, but fat necrosis was observed in 34 % of cases, atrophy and loss of symmetry in 78 % of cases, and hyperpigmentation in 37 % of cases. These changes required multiple revisions and additional flaps to correct deformities. Williams et al. [22] compared the outcomes of patients who had preoperative RT and then TRAM flap breast reconstruction with those of patients who did not undergo preoperative RT. Overall complication rates were comparable between the two groups, with the exception of fat necrosis, which was seen in 17 % of the irradiated group versus 10 % of the nonirradiated patients. Jacobsen et al. [53] reported on a series from the Mayo Clinic and confirmed no increase in complication rates in patients who received preoperative RT compared with patients who received breast reconstruction alone.


Fig. 10.3
Cosmetic results after postmastectomy radiotherapy to the right side and delayed breast reconstruction with a transverse rectus abdominis myocutaneous flap
In the study conducted by Albino et al. [54] among 76 women who underwent autologous breast reconstruction, complications occurred in 70 % of cases after RT and 47 % of these required surgery for postoperative RT effects. Fat necrosis or fibrosis was noted in 19.7 % of patients, skin complications (retraction or hypertrophic scarring) were recorded in 30.3 % of patients, and 27.6 % of patients were generally dissatisfied.
Previous published series of LD flap breast reconstruction have shown capsular contracture affecting between 0 and 56 % of patients [25, 55, 56]. This great variability is attributable to the variation in sample size, follow-up, technique, and population involved.
The LD muscle is considered a useful flap in the previously irradiated chest, and no increase in flap loss has been documented, although prior RT negatively affects the aesthetic results [57]. Nevertheless, patient satisfaction was similar between patients who underwent immediate breast reconstruction with PMRT and patients who underwent delayed breast reconstruction [58]. Apffelstaedt et al. [59] found no significant difference in the complication rate between preoperative irradiated and nonirradiated women.
More recently, some studies have focused on DIEP flap breast reconstruction. The general recommendation remains that of delaying breast reconstruction until after the completion of PMRT. A case–control study from the Memorial Medical Center in New Orleans comparing a small series of patients receiving PMRT after breast reconstruction with patients having DIEP flap breast reconstruction alone found substantially higher rates of fat necrosis (23 % vs 0 %), fibrosis or shrinkage (57 % vs 0 %), and contracture (17 % vs 0 %) in the irradiated patients, but no difference in the rate of flap revisions or dehiscence [60]. However, a recent study by Chatterjee et al. [61] found that postoperative RT did not significantly affect breast volume after immediate DIEP flap breast reconstruction and that there was no difference in the rates of other complications between irradiated and nonirradiated patients.
10.4.3 Impact of Reconstruction on Delivery and Quality of PMRT
Conventional RT doses reported in the literature are around 50 Gy in 1.8–2 Gy daily (five times a week) fractions using tangential beams, with a variable proportion of patients receiving boost doses to the scar of typically around 10–16 Gy. Altered fractionated schemes are less used owing to concern they may be associated with a higher risk of late side effects. However, Whitfield et al. [62] reported that the rates of severe capsular contracture in patients receiving the common UK fractionation of 40 Gy in 15 fractions over 3 weeks appeared comparable to those for patients receiving the conventional 5 week schedule, achieving a crude rate of 19.5 %.
Modern RT modalities using an immobilization device and computed tomography to plan RT delivery are bound to minimize the risk of complications [63, 64]. In older series in which the RT technique was not optimal, patients experienced higher complication rates [65]. An important issue in breast reconstruction is whether the immediate reconstruction impairs the delivery of PMRT. In fact, the reconstructed breast is different in size, shape, and firmness compared with the natural one and may cause technical problems related to the design of the radiation fields. The thickness of the chest wall in a reconstructed breast may not be nonuniform, causing dosimetric inhomogeneities of dose within the treatment field, which might translate into higher risk of complications [66]. Because of the steep contour caused by the TE or prosthesis, the junction between the radiation fields can be less precise, leading to regions of underdosage and overdosage (Fig. 10.4).
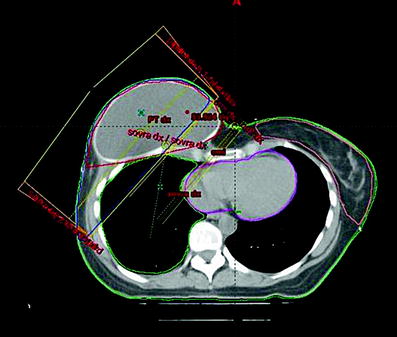
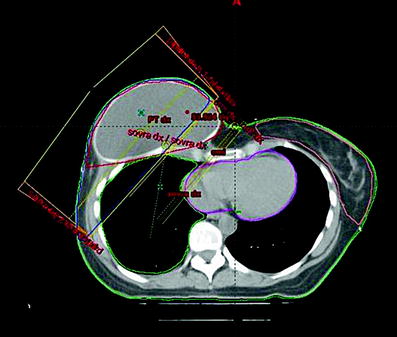
Fig. 10.4
Axial computed tomography slice showing the geometrical match between the medial electron beam field and the lateral photon tangential fields occurring over the steeply sloping contour of the reconstructed breast with a permanent implant
In two follow-up studies from the MD Anderson Cancer Center, the authors examined the impact of an immediate breast reconstruction on optimal coverage of the targeted areas including the chest wall and internal mammary nodes and avoidance of the lung and heart. In the first report published in 2005, only four of the 18 plans met the criteria for optimal treatment [67]. In 2006, a further report on 110 patients with immediate breast reconstruction who were compared with a group of 108 patients without breast reconstruction was published. The treatment plan was compromised in 52 % of the patients with immediate breast reconstruction compared with just 7 % of the control group, 20 % of them having a major compromise [10]. The largest compromises were observed in those with left-sided cancers. Delaying breast reconstruction makes it easy to deliver RT and to spare the organs at risk, allowing the use of electrons [68]. By use of the more sophisticated approach of IMRT, patients with immediate breast reconstruction can achieve excellent local control with acceptable heart and lung doses, even when internal mammary nodes are being treated, although doses to the heart and lung will be higher (Fig. 10.5). IMRT allows one to adequately cover the target volume in almost three quarters of patients [69]. The overall complication rate was extremely low in a group of patients where IMRT was used in one-third of the cases, owing to the improved dose homogeneity [35].
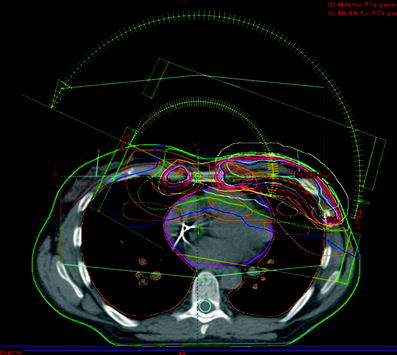
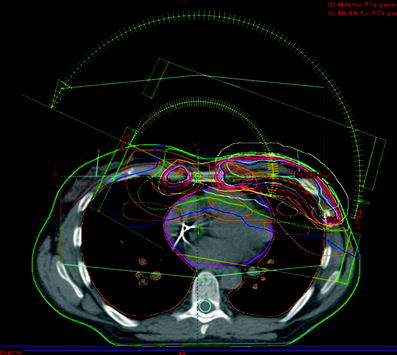
Fig. 10.5
Intensity-modulated radiotherapy plan on an axial computed tomography image using the inverse-planned multisegmental technique to treat the left chest wall and bilateral internal mammary nodes
Regarding the compatibility of radiation and TE/PI reconstructions, prostheses do not interfere with dosimetric distribution as they are essentially tissue-equivalent [70]. Similarly, no dosimetric effects of saline filling in the TEs with consecutively relevant changes in the prescribed dose were seen in dedicated studies [65, 71]. The TE should be kept at a constant volume during RT to avoid treatment setup changes and deviation from the prescribed radiation dose. With repeated dosimetric evaluations during the course of treatment, the TEs appear to go through minimal anatomical changes without any interference with the prescribed dose distribution [72]. The quantification of the radiation dose distribution in the vicinity of the metallic port of the TE and the determination of its potential contribution of the high complication rate is controversial and debated (Fig. 10.6). Two studies measuring the dosimetric changes around the metallic port showed an increased dose in the immediate vicinity of the metallic port owing to the scattering of secondary electrons. As this increased dose does not reach the surface of the TE, it can hardly contribute to increasing the complication rate [73, 74]. On the other hand, the metallic port can attenuate the radiation beam and decrease the dose to the tissue which lies in its direct shadow. However in clinical situations, both the small size of the metallic port and the use of tangential opposed beams make the chance of underdosage quite small and acceptable [75].
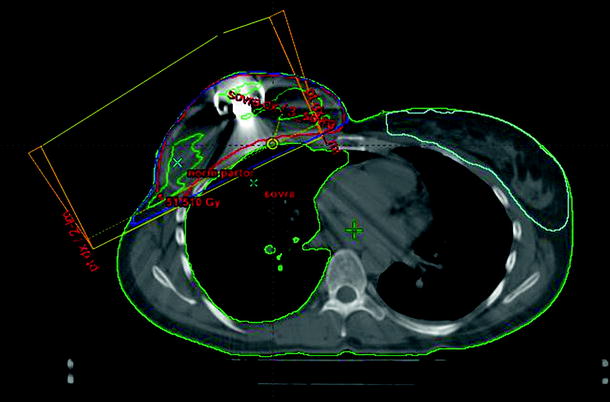
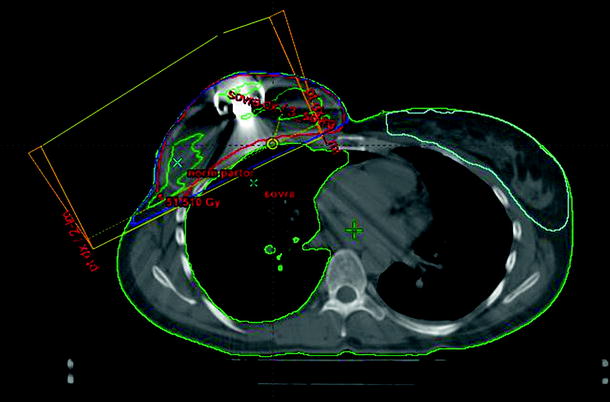
Fig. 10.6
Axial computed tomography slice showing the interference of a high-Z metallic port with photon tangent beams of radiation fields in the tissue expander reconstruction
Risk factors for increased complications related to radiation treatment have been identified throughout the studies.
The use of a bolus is associated with severer intensity of acute side effects and impaired cosmesis [76]. The choice of a customized bolus rather than a standard one may lead to a significantly better outcome [35].
The subpectoral placement of the implant may be preferable over a subcutaneous placement because of the lower propensity for capsular contracture due to RT [36, 77]. Textured implants are less likely to develop capsular contracture than smooth ones, since they allow minimal abnormal collagen deposition on their surface [78].
10.5 Reconstruction in Previously Irradiated Fields
Breast reconstruction in the case of salvage mastectomy for local recurrence after breast conservative surgery and RT (QUART) faces the difficulty of being performed on previously irradiated and manipulated tissue. Prior RT to the chest may have a negative impact on the recipient vessels and predispose to vascular complications. In a study reviewing the outcome of flaps placed in an irradiated field, there was a significantly higher rate of intraoperative vascular complications (7.6 % vs 14.2 %, p = 0.003) in the irradiated group (9.5 % vs 17.3 %, p = 0.001) and a trend toward higher anastomotic revision rates [79].
More recent studies show that the combination of flaps alongside a breast prosthesis offers greater advantages in previously irradiated patients [30, 55]. In fact, several studies demonstrated that when an autologous flap is used with an implant for reconstruction of previously irradiated breast, the flap may protect the implant from the negative effects of RT [56].
An interesting study by Michy et al. [80] reported a series of patients treated with neoadjuvant RT in which immediate breast reconstruction accomplished by a LD flap with a prosthesis showed a lower complication rate and fewer additional surgical revisions than either a TRAM flap alone or a simple prosthetic implant. Similar results were recorded in small series of patients undergoing salvage mastectomy plus LD-flap-based immediate breast reconstruction, where the incidence of capsular contracture was acceptable, being as high as 12–17 % [81].
The use of TE alone is generally considered a contraindication in the case where RT has previously been administered. Few reports of abnormal concave and painful deformity of the chest wall were reported using a TE after QUART [82]. Conversely, the feasibility of implant reconstruction after QUART was described by Persichetti et al. [83]. No significant difference in the total number of capsular contractures was observed between previously irradiated patients undergoing immediate breast reconstruction with two-stage TE/PI and the nonirradiated group, but major complications occurred more frequently if RT had been delivered.
10.6 Aesthetic and Satisfaction Considerations
The cosmetic outcome of all breast reconstructions deteriorates over time even though RT is not performed [84]. In fact, the irradiated reconstructed breasts show the worst aesthetic outcome, which can be evident even after a long time. A worsened aesthetic result is observed with increasing tumor stage, bolus application, and earlier delivery of RT after the reconstructive procedure [85]. Several authors agree that the sequencing of PMRT did not affect the level of satisfaction [16, 49], whereas others observed a trend toward improved cosmetic outcomes when breast reconstruction is delayed [19, 58]. Recent evidence demonstrated that autologous tissue flaps provide greater levels of aesthetic satisfaction relative to TE/PI reconstruction. Excellent/good cosmetic outcome is generally reported in more than 80 % of patients undergoing PMRT and autologous breast reconstruction [45, 52], although aesthetic appearance and satisfaction were generally worse than in nonirradiated patients [18, 22, 51].
References
1.
2.
3.
4.
Rudolph R (1982) Complications of surgery for radiotherapy skin damage. Plast Reconstr Surg 70:179–185PubMed




Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree








