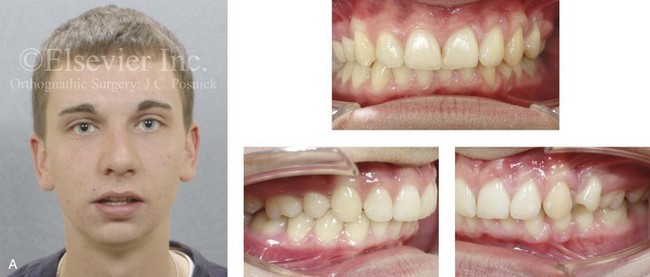
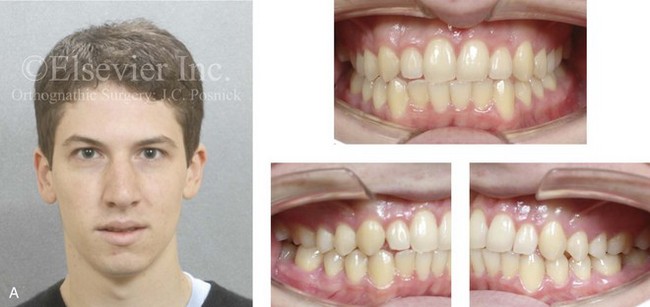
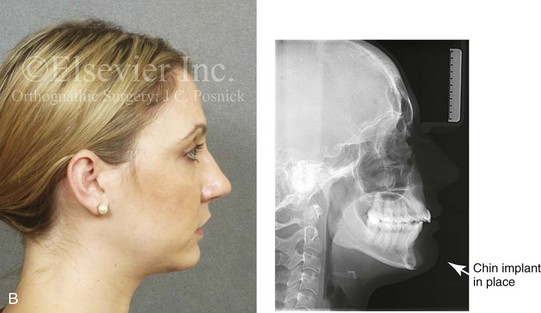
19 • Treatment Indications and Objectives • The Role of Growth Modification in the Preadolescent Child • Orthodontic Camouflage Approach • Postsurgical Orthodontic Maintenance and Detailing • Complications, Informed Consent, and Patient Education • Temporomandibular Disorders: The Effects of Orthodontics and Orthognathic Surgery The surgical correction of the underdeveloped mandible was first reported in the American literature by Vilray P. Blair in the Journal of the American Medical Association in July 1909.7 Dr. Blair presented two cases of retrognathia in which a horizontal ramus osteotomy was performed on each side of the mandible. The operative technique was carried out through a preauricular stab incision; an aneurysm needle was introduced posteriorly to the neck of the condyle and directed medially around to the ascending ramus, where it then exited through the cheek in front of the anterior border of the ramus. A Gigli saw was then put in place and blindly used to complete an osteotomy. The same procedure was completed on the opposite side of the jaw, and then the mandible was advanced into the desired occlusion. Intermaxillary fixation was applied until a callus formed. As a result of the limited bone contact across the osteotomy sites, a strong relapse tendency required persistent counterforces with continued intermaxillary elastics. Extrusion of the incisors with periodontal sequelae and recurrent malocclusion was a frequent observation. Mandibular deficiency is the most prevalent form of dentofacial deformity.2,30,32,39,43 It is more common among Caucasians than Africans or Asians, which suggests that a hereditary component is a predominant part of the etiology. During the mid 1970s, the public health service of the U.S. Department of Health, Education, and Welfare conducted an assessment of the occlusions of children who were 6 to 11 years old and 12 to 17 years old. These collected data indicated that approximately 20% of the sample populations had an Angle Class II malocclusion. Unfortunately, no other means of evaluation were performed to separate those children with a Class II jaw disharmony from those with a more straightforward dental Class II malocclusion. According to a National Health and Nutrition Examination Survey, severe mandibular deficiency (defined as >7 mm of positive overjet) in the U.S. Caucasian population has a prevalence of approximately 10%.43 This pattern of Class II excess overjet is less frequent among African-American and Mexican-American groups. It can be assumed that more than 7 mm of overjet indicates a jaw discrepancy of such magnitude that orthognathic surgery would be the preferred way to manage the problem. The majority of these patients will have dentofacial deformities that fall into the categories of a long face growth pattern, maxillomandibular deficiency, or primary mandibular deficiency with or without arch-width discrepancy. • Articulation errors during speech and swallowing difficulties that result from the Class II malocclusion are expected (see Chapter 8). • Difficulties with chewing and with lateral and protrusive mandibular movements as a result of the Class II malocclusion are also expected. • Upper airway obstruction during sleep often exists as a result of the retropositioned tongue. Obstructive sleep apnea should be ruled out (see Chapter 26). • Detrimental long-term effects on the dentition and the periodontium as a result of the crowding of the mandibular teeth in limited alveolar housing or from previous camouflage orthodontic treatments are often seen (see Chapters 5 and 6). • A higher incidence of temporomandibular disorders that result from mandibular deficiency Class II malocclusion have been reported (see Chapters 9 and 36). • The lower lip is curled and everted, and it is often wedged behind the incisors with an accentuated labiomental fold. The shorter the lower anterior facial height, the greater the tendency for an accentuated labiomental fold. • The gonial angles of the mandible tend to be relatively square. The shorter the face and the deeper the bite, the more acute the angles. • There is a retruded and weak chin with a convex profile. • There is a deficient mandible with the illusion of a large nose. • There is a short chin-to-neck length and an obtuse angle, often with a double chin (even in a thin individual). • There are varied degrees of increased overjet with a Class II molar and canine relationship. • The crowding of the teeth within the lower arch (i.e., the smaller the mandible, the greater the crowding) needs to be evaluated, and so does lower incisor flaring. Mandibular dental compensations often mask the true skeletal discrepancy. • There are varied degrees of dental compensation in the upper jaw with either procumbency (i.e., “buck teeth”) or maxillary incisors that are retroclined. • The anterior deep bite (i.e., excessive overbite) may involve impingement of the anterior maxillary palatal tissues by the mandibular incisors. • There is an excessive curve of Spee in the mandible (i.e., the deeper the anterior bite, the greater the excess curve). • A reduced or negative curve of Spee is found in the maxillary arch. • Dental crowding may also be seen in the maxilla (i.e., the more constricted the maxilla, the greater the crowding). • Excessive wear facets, cusp fractures, and significant restorations in the posterior dentition are frequent findings in adults. • Accelerated loss of the periodontium associated with the maxillary incisors (due to traumatic occlusion or previous orthodontics); the maxillary molars (due to arch constriction or previous orthodontics); and the mandibular incisors (due to supraeruption and anterior flaring from previous orthodontics) may be seen in adults. • Horizontal retrusion is measurable at the B-point of the mandible. • The A-point–nasion–B-point angle is generally increased as a result of the retrusive lower jaw. • Excessive procumbency of the mandibular incisors is frequently measurable. • A vertically short and retrusive chin is generally measurable. • The maxillary incisors are often procumbent, but they may be retropositioned as a result of previous extractions and camouflage orthodontics. The individual’s immediate aesthetic concerns often center on 1) unfavorable lower-lip contours (e.g., a curled and everted lower lip with an accentuated labiomental fold) 2) a lack of prominence of the chin (e.g., a weak profile) and 3) an unattractive neck (e.g., a soft-tissue double-chin tendency).27,38,39,42,48,47,50,59 Functional issues are also to be expected. For example, when the anterior bite is “deep,” it will cause irritation of the gingival tissues of the palate just behind the maxillary incisors. Partial obstruction of the upper airway as a result of a retropositioned tongue is also common (i.e., heavy snoring, restless sleep, daytime fatigue, and documented or undiagnosed sleep apnea; see Chapter 26).11,62 Complaints of an uncomfortable “dual” bite, chewing difficulties, masticatory muscle discomfort, and audible speech articulation errors are frequent. The individual with a Class II deep bite may have a greater tendency toward clicking (i.e., anterior disc displacement) in each temporomandibular joint.25,51 Interestingly, there is little scientific evidence to support the notion that the signs of clicking will into more significant temporomandibular joint pathology (see Chapter 9). When the preadolescent child with mandibular deficiency is identified, a growth modification approach to treatment is frequently considered by the evaluating orthodontist.13,33,32 Cozza and colleagues completed a systematic review of the literature to assess the efficacy of functional appliance use for enhancing mandibular growth in subjects with Class II malocclusions.14 With the use of the Medline database, the survey covered the period from January 1966 to January 2005. A review of 704 articles confirmed only 22 that qualified for the final analysis. Of these 22 articles, only four randomized clinical trials were retrieved and found to be worthy of inclusion. Interestingly, none of these four trials reported a clinically significant change in mandibular length to be induced by functional appliances in the patients with Class II deformities. According to Proffit, the only concrete indications for the treatment of the preadolescent mixed dentition child with a mandibular deficiency who presents without an anterior open bite are the following44: • Significant trauma to the palatal tissue (i.e., the lower incisors are injuring the palatal mucosa) or other indications of potential irreversible tissue damage • Special concerns about the effects of the condition on the child’s psychological well-being and the strong belief that the recommended treatment will alter this in a positive way • Skeletal maturation that is well ahead of dental development so that the adolescent growth spurt occurs before the mixed dentition ends 1. The alignment of the upper incisors (i.e., the correction of lingual tipping with a Class II, Division 2 malocclusion) to prevent any interference with the forward movement of the mandible. 2. Attempts to impede the biologic programmed forward growth of the maxilla and to facilitate the forward growth of the mandible. Extraoral (posterior vectored) compressive forces are typically applied to the maxilla through a headgear device. 3. Attempts to stimulate the mandibular posterior teeth to hypererupt while preventing the incisors from doing so. During this process, it is hoped that the deep overbite will improve. An intra-oral functional appliance is often designed to facilitate these events. When the orthodontist proceeds with growth modification maneuvers and a less than favorable biologic response is realized, it is apparently tempting to proceed with a camouflage (dental compensation) approach (Figs. 19-1 through 19-5).34,35,37,36,42 This would be carried out to “neutralize” the occlusion rather than to position the teeth solidly into the alveolar process in combination with orthognathic surgery. Current evidence-based medical standards recommend that the treating orthodontist have a “timeout” (i.e., a sit-down discussion and reassessment with the parents and the patient) that includes a review of the records (e.g., photos, models, radiographs) and a discussion of the biologic effects on the airway, the facial aesthetics, the occlusal stability, and the periodontium that may result from the various treatment options. A referral to an experienced orthognathic surgeon for the discussion of possible future surgical aspects is highly recommended. Figure 19-1 A 20-year-old man with a primary mandibular deficiency growth pattern requested a surgical consultation for a weak chin. During his early teenage years, the patient underwent growth modification in an attempt to stimulate the forward projection of the mandible. This was followed by an orthodontic camouflage approach that included maxillary first bicuspid extractions to retract the anterior teeth. In addition, the mandibular anterior dentition was flared forward. His history was significant for heavy snoring, restless sleeping, and a degree of daytime fatigue, all of which are suggestive of obstructive sleep apnea. Examination confirmed a retrognathic mandible with a molar Class II deep-bite malocclusion. The mandibular incisors were crowded and procumbent. The family had hoped that a chin implant would be effective to manage the aesthetic effects. A sleep study was recommended, and an orthognathic approach with redo orthodontic treatment including lower bicuspid extractions was suggested as the preferred method to improve the airway, to achieve long-term dental health, and to enhance facial aesthetics. A, Frontal facial and occlusal views. B, Profile facial view and lateral cephalometric radiograph. Figure 19-2 A 21-year-old woman with a primary mandibular deficiency growth pattern requested a surgical consultation for a weak chin. During her early teenage years, the patient underwent growth modification in an attempt to stimulate the forward projection of the mandible. This was followed by an orthodontic camouflage approach. The mandibular anterior dentition was flared forward. Her history was significant for restless sleeping and a degree of daytime fatigue, which are suggestive of obstructive sleep apnea. Examination confirmed a retrognathic mandible with a Class II malocclusion. The mandibular incisors were crowded and procumbent. The family had hoped that a chin implant would be effective to manage the aesthetic effects. A sleep study confirmed obstructive sleep apnea (respiratory disturbance index = 18/hour). An orthognathic approach with redo orthodontic treatment including lower bicuspid extractions was recommended as the preferred method to improve the airway, to achieve long-term dental health, and to enhance facial aesthetics. A, Frontal facial and occlusal views. B, Profile facial view and lateral cephalometric radiograph. Figure 19-3 A 20-year-old man with a primary mandibular deficiency growth pattern requested a surgical consultation for a weak chin. During his the early teenage years, the patient underwent growth modification in an attempt to stimulate the forward projection of the mandible. This was followed by an orthodontic camouflage approach. The mandibular anterior dentition was flared forward. The patient’s history was significant for heavy snoring, restless sleeping, and a degree of daytime fatigue, all of which are suggestive of obstructive sleep apnea. Examination confirmed a retrognathic mandible with clockwise rotation of the maxillomandibular complex. The mandibular incisors were crowded and procumbent. He had hoped that a chin implant would be effective to manage the aesthetic effects. An orthognathic approach with redo orthodontic treatment including lower bicuspid extractions was recommended as the preferred method to improve the airway, to achieve long-term dental health, and to enhance facial aesthetics. A, Frontal facial and occlusal views. B, Profile facial view and lateral cephalometric radiograph. Figure 19-4 A 29-year-old women arrived to discuss chin aesthetics. During the mixed dentition, she was recognized as having mandibular deficiency and a constricted maxillary arch width. At that time, she underwent growth modification techniques that included headgear. She also underwent rapid palatal expansion followed by compensatory orthodontic mechanics to neutralize the occlusion, but this also involved proclination of the incisors. A retrusive profile and a dual bite remained. The patient had recently undergone the placement of a chin implant without fixation. Aesthetic modification of the anterior maxillary dentition was also completed. The patient was displeased with the cosmetic results of a deepened labiomental fold, a mobile chin implant, and a “button” appearance during lip closure. There is a dual bite with Class II malocclusion when the teeth are in centric relation. A, Oblique and frontal facial views. B, Profile facial view and lateral cephalometric radiograph 6 months after chin implant placement. Figure 19-5 A 43-year-old woman arrived to discuss the aesthetics of her weak chin and premature facial aging. During her late mixed dentition, she was recognized as having mandibular deficiency with a Class II malocclusion. At that time, she underwent growth modification techniques followed by compensatory orthodontic mechanics. This included upper first bicuspid extractions, the retraction of the anterior maxillary teeth, and the proclination of the mandibular incisors, all in an attempt to neutralize the occlusion. A retrusive profile and a dual bite remained. The weak profile of her adolescence had progressed into premature facial aging. She also had a lifelong history of obstructed nasal breathing, restless sleeping, and excessive daytime fatigue, all of which are suggestive of obstructive sleep apnea. An orthognathic approach with redo orthodontic treatment including lower bicuspid extractions was recommended as the preferred method to improve the airway, to achieve long-term dental health, and to enhance facial aesthetics. A, Frontal facial and occlusal views. B, Profile facial view and lateral cephalometric radiograph. An orthodontic camouflage approach for the individual with mandibular deficiency may take the form of maxillary premolar extractions so that the upper incisors can be retracted. This is generally combined with the flaring of the mandibular incisors. When this is carried out in the individual with a mandibular deficiency, the short-term objective of a neutralized occlusion may be achieved, but the following are potential sequelae: 1) unfavorable long-term facial aging 2) the risk for obstructive sleep apnea later in life 3) long-term periodontal deterioration 4) lower anterior crowding with recurrent malocclusion and 5) an inconsistent occlusion (i.e., a dual bite) (see Figs. 19-1 through 19-5). The orthodontist may feel favorable toward a camouflage approach on the basis of the belief that the patient can always have a “chin implant” to improve his or her facial aesthetics. Unfortunately, this approach will rarely achieve a pleasing aesthetic outcome. A chin implant tends to result in 1) an accentuated labiomental fold 2) an overly prominent pogonion and 3) a residual obtuse neck–jaw angle (Fig. 19-4). Furthermore, it does nothing for any baseline masticatory and airway dysfunction (see Chapter 37). Stahl and colleagues carried out a longitudinal study to compare the biologic jaw growth changes of untreated subjects with Class II, Division 1 malocclusions as compared with those subjects with a normal Class I occlusion.55
Primary Mandibular Deficiency Growth Patterns with or without Maxillary Arch Constriction
Functional Aspects
Clinical Characteristics
Dental Findings
Radiographic Findings
Treatment Indications and Objectives
The Role of Growth Modification in the Preadolescent Child
Orthodontic Camouflage Approach







Definitive Reconstruction
Timing of Orthognathic Surgery
![]()
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree


Primary Mandibular Deficiency Growth Patterns with or without Maxillary Arch Constriction





