The recent resurgence of preservation rhinoplasty has been driven by theoretic esthetic and functional advantages of keystone preservation, as well as development of modified techniques that have expanded surgical indications. Current literature is limited but supports superior or equivalent patient-reported esthetic and functional outcomes for dorsal preservation when compared with conventional resection techniques. However, residual hump or recurrence of dorsal convexity remains a challenge. A variety of descriptive studies have reported excellent outcomes for modified preservation methods of bony vault and septal management. Robust comparative studies are needed to further evaluate the benefits and indications for each approach.
Key points
- •
In dorsal preservation surgery, the osseocartilaginous vault is mobilized as a single unit to minimize disruption of the nasal keystone.
- •
There are various preservation approaches to management of the bony vault and septum and a growing body of literature suggests acceptable functional and esthetic outcomes for classic preservation methods, as well as newer modifications.
- •
The most common reported complications of dorsal preservation surgery include recurrent hump and dorsal axis deviation.
- •
Comparative and long-term objective studies are still needed to further delineate differences in described approaches.
Background
There are 2 distinct approaches for reducing the osseocartilaginous nasal dorsum. In the traditional structural approach, first described by Joseph in 1898, the midvault is opened and the dorsal nasal bones and cartilages are resected. While this has been the primary approach used by most modern rhinoplasty surgeons, resection of this area by nature violates the structural integrity of the keystone junction, which necessitates midvault reconstruction and may lead to a variety of undesirable consequences.
In recent years, there has been a global resurgence of interest in the dorsal preservation approach. These methods were first described by Goodale and Lothrop in the early nineteenth century and further promoted by Cottle in 1946. The cornerstone of dorsal preservation rhinoplasty (DPR), in contrast with conventional hump resection (CHR), is preservation of the osseocartilaginous bony vault. In theory, preserving this architecture has several advantages including maintenance of the structural integrity of the keystone area, patency of the internal nasal valves (INV), and natural dorsal esthetic lines. ,
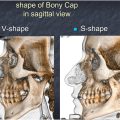
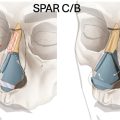
A primary surgical consideration in DPR is the approach to the osseocartilaginous vault. Two classic foundation techniques exist: Push Down (PD) and Let Down (LD). Goodale is credited with development of the PD, in which lateral and root osteotomies are performed to mobilize the nasal vault en bloc into the nasal cavity, with the lateral walls sitting medial to the maxilla in the final position. , Lothrop pioneered the LD, in which wedge excisions of the bony sidewalls are performed to mobilize the nasal pyramid down onto the maxilla, rather than within it. Deviated or crooked noses may be managed with asymmetric bony techniques. Surface techniques modulate the hump superficially, without impaction osteotomies. These techniques include Ishida and Ferriera’s Spare Roof A and B. Some have combined surface modifications and foundational methods. For example, undesirable S-shaped nasal bones may be converted to ideal V-shaped nasal bones, allowing for the use of preservation methods. Indeed, examination of old notes from Cottle reveal that he often rasped the dorsum prior to impaction.
Furthermore, several partial preservation techniques, including surface techniques, have been forwarded. These techniques incorporate surface modifications and some separate treatment of the bony dorsum from the cartilaginous midvault. For example, Ferreira detailed the Spare Roof Technique (SRT) in which the bony vault is treated with ostectomy and osteotomies while the cartilaginous midvault is preserved. Ishida and Ozturk described surface modifications following disarticulation of the upper lateral cartilages (ULC) from the nasal bones. , Robotti’s Modified Dorsal Split (MDS) involves separation of the ULC from the septum but preservation of the flared edges at the septum, followed by PD/LD for the bone. The Dorsal Roof Technique (DRT) described by Tas incorporates similar ULC separation with dorsal lowering permitted by medial osteotomies and a radix osteotomy. These modifications have expanded indications of DPR.
Septal resection is another important consideration in DPR and is a requisite for lowering of the nasal vault. Original descriptions primarily detail a high subdorsal strip resection. , , A variety of modifications have been described and can generally be classified by region of resection into high (eg, subdorsal strip), intermediate (eg, modified subdorsal strip method [MSSM], Tetris, subdorsal-Z flap), and low septal (eg, Cottle) methods.
Discussion of outcomes
Comparison of Conventional Hump Resection and Dorsal Preservation Rhinoplasty
There have been a number of studies comparing CHR and DPR approaches, many of which incorporate patient-reported outcome measures (PROMs). These are summarized in Table 1 .
| Author (Year) | Design | Population (n) | Outcome Measures | Results | Other |
|---|---|---|---|---|---|
| Tas et al, 2020 | Prospective cohort | 50: Dorsal preservation rhinoplasty (DPR) with let down (LD) (26), open conventional hump resection (CHR) (24) | Functional patient-reported outcome measures (PROMs) (Nasal Symptom Obstruction Evaluation [NOSE], Sinonasal Outcome Test-22 [SNOT-22], Visual Analog Scale [VAS]). | Improvement for both groups at least 6 mo after surgery, no difference between groups. | Two patients in each group underwent revision surgery. |
| Patel et al, 2023 | Retrospective matched cohort | 163: DPR with LD/modified subdorsal strip method (MSSM) (81), CHR (82) | Functional (Standardized Cosmesis and Health Nasal Outcomes Survey-Obstruction [SCHNOS-O], VAS-Function [VAS-F]) and cosmetic (SCHNOS-Cosmesis [SCHNOS-C], VAS-Cosmesis [VAS-C]) PROMs. | Improvement for both groups at least 6 mo after surgery, no difference between groups. | Short-term VAS-C better in DPR group. Radix grafting more common in DPR group, dorsal only grafting and midvault reconstruction more common in CHR group. |
| Zarei et al, 2024 | Prospective randomized cohort | 85: DPR with LD/MSSM (35), CHR (50) | Functional (SCHNOS-O, VAS-O) and cosmetic (SCHNOS-C, VAS-C) PROMs. Nasal tip projection and rotation, nasal width, hump height. | Improvement for both groups 1 y after surgery, no difference between groups. | One patient from each group underwent revision surgery. |
| Alan et al, 2023 | Prospective randomized cohort | 34: DPR with Push Down (PD) (15), CHR (19) | Functional (SCHNOS-O, NOSE) and cosmetic (SCHNOS-C) PROMs. Rhinomanometry. | Improvement for both groups 3 and 12 mo after surgery, no difference between groups. | Only included dorsal hump <4 mm. |
| Alsakaa et al , 2024 | Prospective randomized cohort | 50: DPR with PD/subdorsal strip (25), CHR (25) | Functional and cosmetic PROMs (SCHNOS). Surgeon evaluation questionnaire (SREQ). Computed tomography (CT) measurements of internal nasal valves (INV) and cross-sectional area (CSA). | Improvement for both groups 6 mo after surgery, no difference between groups. | |
| Abdelwahab et al, 2020 | Cadaveric cohort | 12: DPR with PD then LD (6), CHR (6) | INV and CSA measured from CT radiographs. | Preserved measurements following CHR and LD, and reduced measurements following PD . | |
| Ozuker et al, 2020 | Prospective cohort | 22: LD/PD asymmetric DPR (10), CHR (12) | Angle of deviation measured from frontal photographs. | Improvement for both groups after surgery, no difference between groups. | Only I-shaped crooked nose deformity. Operative time was shorter with DPR technique. |
| Verkest et al, 2023 | Retrospective matched cohort | 172: T-bar hybrid preservation (110), CHR (62) | Functional (NOSE) and cosmetic (FACE-Q, Utrecht Questionnaire [UQ]) PROMs. | Improvement for both groups 6 mo after surgery, no difference between groups. | Less frequent need for middle third INV grafting in T-bar preservation group. |
| Ferreira et al, 2021 | Prospective randomized cohort | 250: Spare Roof Technique [SRT] (125), CHR (125) | Functional (nasal patency VAS) and cosmetic (UQ VAS) PROMs. | Improvement for both groups. However, SRT group had greater esthetic improvement at 3 and 12 mo, and greater functional improvement at 12 mo. |
Tas and colleagues conducted a 50-patient study comparing functional results between LD and open CHR. Both groups showed significant improvement across functional PROMs (Sinonasal Outcome Test-22[SNOT-22], Nasal Symptom Obstruction Evaluation [NOSE], nasal congestion Visual Analog Scale [VAS]) at least 6 months following surgery, with no significant difference observed between the groups. In a matched cohort study (n = 62), Patel and colleagues demonstrated similar findings when comparing structural preservation (LD, MSSM) with CHR. Patients were matched by several parameters including hump size. There were again no differences in functional (Standardized Cosmesis and Health Nasal Outcomes Survey-Obstruction [SCHNOS-O], /VAS-Function [VAS-F]) PROMs between the groups at long-term follow-up. This study additionally evaluated cosmetic outcomes (SCHNOS-Cosmesis [SCHNOS-C], VAS-Cosmesis [VAS-C]) and found equivalent results. Zarei and colleagues conducted a randomized study with 84 patients comparing CHR with DPR (LD, MSSM). Similar to prior studies, they found no significant difference in functional or cosmetic PROMs between the groups at 1 year. They additionally evaluated nasal tip projection and rotation, nasal width, and residual hump and again found no difference between the cohorts.
An article by Alan and colleagues built on these findings with the addition of rhinomanometry data. In this randomized study, 34 patients with dorsal hump less than 4 mm underwent either open CHR or closed DPR (PD). There was no significant difference between the groups in functional or cosmetic PROMs (NOSE, SCHNOS-O, SCHNOS-C). Additionally, rhinomanometry measures of total nasal volume and airway resistance were similar between the groups. Alsakaa and colleagues compared PROMs, Surgeon Rhinoplasty Evaluation Questionnaires, and INV angle and cross-sectional area (CSA) measurements between patients undergoing DPR (PD, subdorsal strip, n = 25) and CHR (n = 25). All measures improved for both groups after surgery, but there was no difference between the groups. In a cadaveric study by Abdelwahab and colleagues, 6 heads underwent either CHR or DPR (PD and LD). INV angle and CSA were measured from preoperative and postoperative radiographs. These measurements did not change following CHR or LD but were both significantly reduced following PD. This finding may support that pushing the nasal walls medially into the maxilla narrows the INV and nasal airway. However, with other studies showing no significant difference in functional outcomes, the clinical importance of this is unclear.
Verkest and colleagues compared DPR with a modified T-bar hybrid preservation technique (n = 110) to a matched cohort undergoing dorsal split component reduction (n = 62). They showed similar improvement in esthetic and functional PROM scores (NOSE, FACE-Q, Utrecht Questionnaire [UQ]) between the groups at 6 months, with less frequent need for INV grafting in modified DPR patients. A study by Ferreira and colleagues is unique in suggesting some possible long-term differences between techniques. In a randomized prospective study, 250 patients underwent either CHR or SRT. Only primary surgeries were included and there were no limitations in hump size. They found significant esthetic and functional improvement in both groups following surgery as measured by the UQ VAS and a nasal patency VAS, respectively. However, the SRT group had significantly greater esthetic improvement than the structural group at 3 and 12 months, as well as greater functional improvement at 12 months. These findings suggest that SRT may yield superior long-term outcomes compared to traditional CHR.
Overall, studies comparing CHR and DPR outcomes are limited. However, most existing literature supports that both approaches yield similar outcomes. As with any procedure, careful patient selection is critical to optimize outcomes. In a case series by Saban and colleagues, 57.2% of primary rhinoplasty candidates were found to have appropriate anatomy for DPR with the remainder being better suited for conventional rhinoplasty. Traditional DPR candidates are those with existing well-shaped dorsal esthetics. Patients with a severely kyphotic bony dorsum or S-shaped nasal bones are considered poor candidates due to increased risk of residual hump. Those with a wide midvault or irregularly shaped bony pyramid are likely to have persistent and unsatisfactory dorsal lines. Patients with a deep nasofrontal angle may have further undesirable drop of the radix with preservation techniques. The positive outcomes published in the presented literature are likely a product of both appropriate patient selection and technical execution, and highlight the value of different techniques in the appropriate clinical context. Fig. 1 demonstrates outcomes of 2 patients, one undergoing DPR and another CHR for correction of a dorsal hump.

Outcomes in Crooked Noses
Regarding the crooked nose, Ozucer and colleagues published a study evaluating a mixed DPR technique. This article compares results between CHR and asymmetric DPR (PD for deviated and LD for nondeviated side) in a 22-patient group with I-shaped crooked nose deformity (CND). Preoperative and postoperative photographs were evaluated by a blinded reviewer for angle of deviation and both groups were found to have similar improvement after surgery. Of note, the authors state that anectodatly, operative time was significantly shorter with DPR even despite a technical learning curve.
Several other studies have reported positive outcomes for DPR in CND, but these are not compared to CHR. Alan and colleagues published on the above asymmetric DPR, using PD on the shorter and LD on the longer nasal bone to correct I-shaped deviations. SCHNOS and rhinomanometry data improved at 12 months in 23 patients. Jasso-Ramirez et al. described an LD modification for C-shaped or I-shaped twisted noses with unilateral or asymmetric bony wedge resections. Deviation angle improved by 81% for C-shaped and 79% for I-shaped noses, suggesting that this modification may also be effective for C-type deviations. Ozturk described improved outcomes following both the mix-down and hybrid preservation techniques for hump reduction in the deviated nose. , Rodrigues and colleagues reported on outcomes of 54 patients with CND, and found functional (nasal patency VAS) and esthetic (UQ) outcome measures improved significantly after SRT.
Comparison of the Push Down and Let Down Foundational Techniques
Very few studies compare results between PD and LD. Wells and colleagues published a systematic review assessing the indications for and complications of the classic techniques. Across 30 studies, they identified 307 who underwent PD and 529 patients who underwent LD. They found a significantly lower rate of dorsal hump recurrence (1.3% vs 4.6%, P = .02) and revision surgery (0% vs 5%, P <.001) in the PD compared to the LD cohort, possibly suggesting superior results with PD surgery. However, the authors note that PD is generally indicated only for patients with smaller dorsal humps (<4 mm), which may have confounded the results. ,
A proposed benefit of LD over PD is a lesser degree of nasal airway obstruction, as the bony pyramid is released to rest on the maxilla rather than medially into it. As previously discussed, Abdelwahab and colleagues performed a cadaveric experiment showing INV angle and CSA to be significantly reduced following PD but not LD, possibly confirming this theory. However, the significance of this has yet to be confirmed in the clinical setting. Stergiou and colleagues performed a similar radiographic study with 30 DPR patients measuring radiographic change in INV angle following surgery. They found overall widening of the average INV (20.77 ± 3.2° preoperatively to 21.82 ± 5.7° postoperatively), but did not stratify results by surgical method.
Modified or Hybrid Preservation Outcomes (including Surface Techniques)
As previously mentioned, classic methods of bony vault management include the LD and PD. However, several modifications in the treatment of the osseo-cartilaginous vault exist. These methods have been detailed in the literature with overall positive outcomes. Most reports are case series studies with limited objective outcomes data. Key publications are highlighted here and summarized in Table 2 .
| Author (Year) | Technique | Design | Population (n) | Results |
|---|---|---|---|---|
| Santos et al, 2019 | Spare Roof Technique | Prospective case series | 100 | Significant improvement in esthetic (Visual Analog Scale [VAS] and Likert) and functional (VAS) outcomes at 3 mo and 12mo after surgery. |
| Ferreira et al, 2021 | Spare Roof Technique | Prospective randomized cohort | 125 | Significant improvement in esthetic and functional outcomes (VAS) at 3 mo and 12 mo after surgery. Compared against SR, esthetic improvement was significantly greater in the SRT group at both 3 and 12 mo. Functional improvement was also better in the SRT group, but not significant. |
| Rodrigues et al, 2022 | Spare Roof Technique | Prospective case series | 54, all with crooked nose | Significant improvement in esthetic (UQ) and functional (VAS) at 12 mo after surgery. |
| Tas et al, 2020 | Dorsal Roof Technique | Retrospective case series | 44 | 90% of patients satisfied with form and function after surgery (Rhinoplasty Outcome Evaluation [ROE] questionnaire). Average of 85% of surgeries were successful and 15% were acceptable (surgeon assessment of post-operative images). No cases of revision surgery, post-operative nasal obstruction, or residual hump. |
| Robotti et al, 2019 | Modified Dorsal Split | Case series | 41 | All patients had favorable outcomes (surgeon assessment), with progressive improvement in results over time . There were no surgical complications. |
| Robotti et al, 2023 | Modified Dorsal Split | Retrospective case series | 100 | Significant improvement in esthetic (SCHNOS-C) and functional (SCHNOS-O) scores at 6 mo, with even further reductions in esthetic outcomes at 12 mo. |
| Ozturk et al, 2020 | Modified PD without osteotomy | Retrospective case series | 62 | Significant improvement in patient satisfaction (ROE) 1 year after surgery, with 90% of patients having high postoperative satisfaction. No surgical complications and no cases of revision surgery. |
| Ishida et al, 2020 | Cartilaginous PD with bony cap preservation | Case series | 48 | High surgical success rate , with 95.8% of patients having adequate hump reduction. |
| Azizli et al, 2023 | Cartilaginous PD with bony cap rasping | Case series | 300 | Very high satisfaction ratings among both patients and their surgeons. |
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree