Preparation of the Patient
Preoperative Consultation
The average number of surgical procedures and length of time required to complete all stages of the reconstruction are discussed with the patient (Table 5-1). In cases of repair of the nose, when an interpolated covering flap is planned, the reconstructive sequence includes initial flap transfer, pedicle division 3 weeks later, a contouring procedure 2 or 3 months after pedicle division, and possibly dermabrasion in the office 2 months after contouring of the flap. We therefore advise patients that up to 6 months may be necessary for the restoration to be completed.
TABLE 5-1
Estimated Number of Surgical Procedures and Recovery Periods
| Type of Procedure | Number of Procedures | Initial Recovery |
| Local flap | 1-2 | 1-2 weeks |
| Skin graft | 2 | 1-2 weeks |
| Interpolated flap | 2-4 | 4 weeks |
From Naficy S: Preparation of the patient. In Baker SR, editor: Principles of nasal reconstruction, 2nd ed, New York, Springer, 2011.
Preoperative consultation with the patient is ideally scheduled 4 to 6 weeks before surgery, allowing adequate time for the patient to stop anticoagulant agents. Medications to be avoided beginning up to 3 weeks before surgery include all nonsteroidal anti-inflammatory drugs and vitamin E supplements (Table 5-2). Coumadin should be discontinued 3 to 5 days before surgery. A number of herbal supplements also possess anticoagulant properties and should be avoided.
TABLE 5-2
List of Medications to Avoid Before Surgery
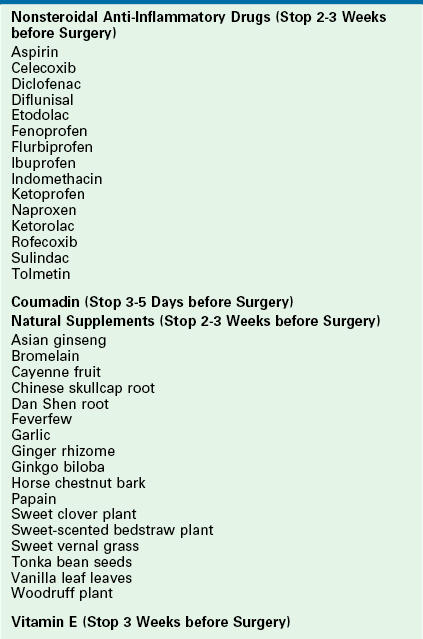
From Naficy S: Preparation of the patient. In Baker SR, editor: Principles of nasal reconstruction, 2nd ed, New York, Springer, 2011.
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree








