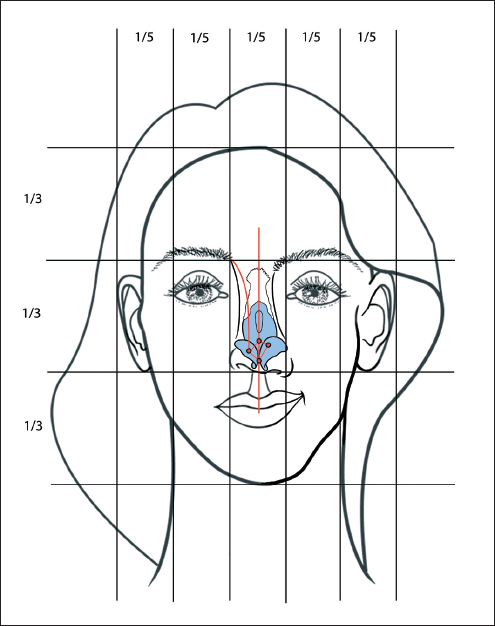
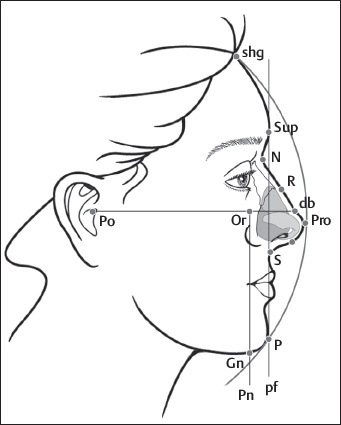
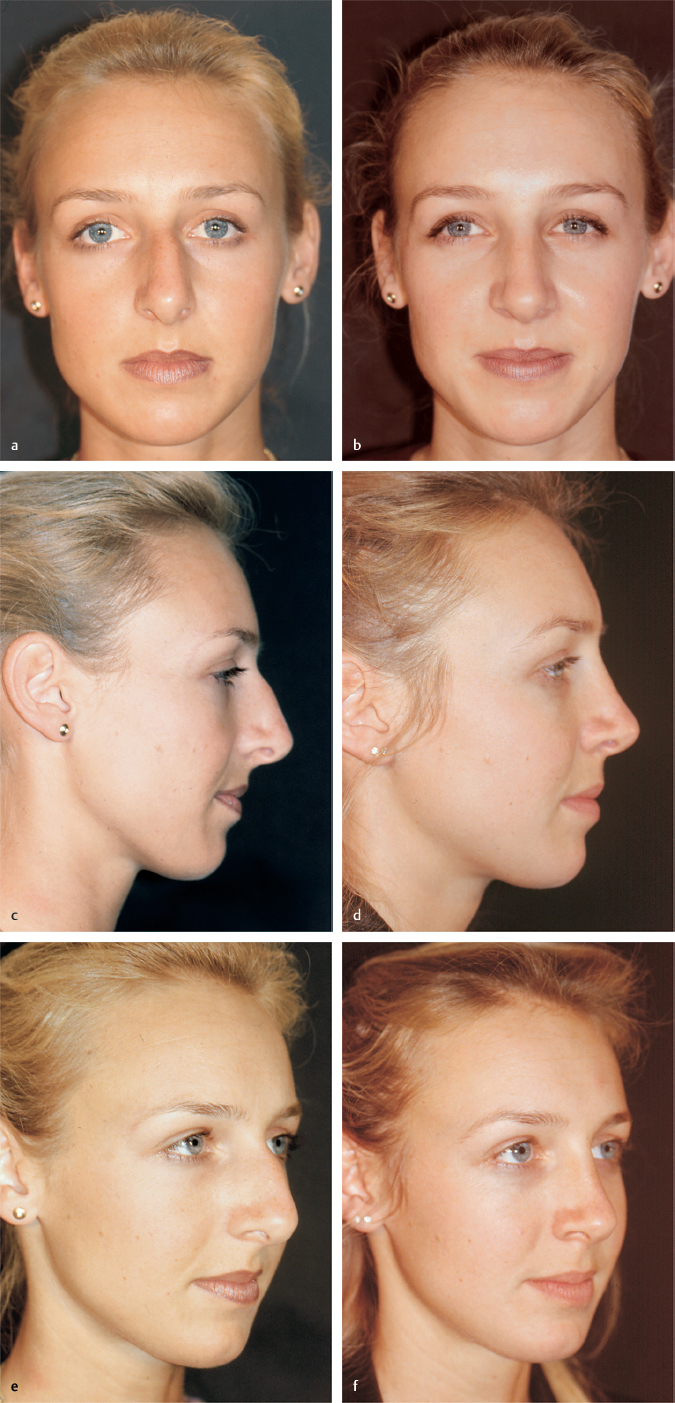
Chapter 5 5.1 Evaluation of the Face and External Nose 5.2 Analysis, Clinical Geometry 5.5 Tips on Photographing Parts of the Body 5.7 Psychological Issues in Rhinoplasty 5.9 Immediate Preoperative Preparations Analyzing the features of the patient’s face and nose starts with something that is difficult to put into words: the first impression. Although the first impression takes but a moment, it conveys a variety of information on the rhinoplasty candidate, which the physician perceives mostly intuitively but interprets very quickly. This includes personality, warmth or antipathy, and the patient’s “manner,” which may be amiable or reserved. The physician notices how the patient presents his/her desire for corrective surgery. It may be expressed clearly and emphatically, or the patient may be less communicative and withdrawn, and the physician has to “probe” to learn whether the patient is introverted or extroverted. The first impression will inevitably include the patient’s body posture (erect or slumped) and body language, handshake (firm or limp), the patient’s voice (loud or soft, hoarse, clear, or dysphonic), and language (expression, grammar, vocabulary, humor). Socrates once said to one of his pupils, “Speak so that I can see you.” Besides the general inspection and clinical examination, the physician should glean as much information about the candidate as possible. He should listen and observe attentively, because the key question—“Should I operate on this patient?”—can be answered in some cases before the facial anatomy is even analyzed. By talking with the patient, the physician can tell whether he/she has an optimistic or pessimistic nature. It is important for the physician to learn what is motivating the patient to seek nasal surgery and find out what expectations the rhinoplasty candidate has for the proposed operation. Openness and willingness to cooperate with the treatment are expressed by firm eye contact, while fleeting looks and lack of concentration in the interview signify communication problems. Besides all of this general information, the physician also looks for evidence of underlying diseases that may or may not relate to the reason for the consultation. Signs of illness are often reflected in the patient’s face. These may include cyanosis of the lips due to ischemic heart disease, jaundice due to liver disease, xanthelasmas due to hypercholesterolemia, the flushed complexion of the hypertensive, and palsies, spasms, or tics of the facial musculature. The consultation, or initial interview, should take place in a quiet, stress-free environment with no time pressure. A full waiting room creates a pressured atmosphere that hampers open communication between the physician and the patient. The best way to do this in a busy practice is to schedule patients for a special appointment before and after rhinoplasties. A surgical office visit in a general hospital otorhinolaryngology department may lead the patient to conclude that “The doctor has other problems; he obviously doesn’t have time for my nose.” In our experience, it is best not to have a telephone in the consultation room, because being interrupted by phone calls during the consultation would serve to reinforce that fear. A computer in the office can also be problematical. By remaining riveted to a data screen, the physician may miss the chance to glean as much information on the patient as possible. The basis for doctor–patient communication in aesthetic surgery must be openness and honesty on both sides. Surgeons must know what the patient really wants. They must honestly convey to the patient what can be done and what is unrealistic or impossible. This is the best way to correct false expectations and preconceptions and avoid failures. The basis for trust is that the physician has time for the patient. He should explain the proposed operation in nontechnical language and address any problems that may arise. If a trusting relationship can be established between the physician and the patient before the surgery, it may be easier for the patient to tolerate any touch-ups that may be needed after the primary operation. The patient must go into the operation with the knowledge that the surgeon has addressed his/her problem with time and dedication and will do everything necessary to carry out the jointly discussed plan of operation. The interview should be conducted with open-ended questions, which invite patients to express themselves more fully. Examples of open-ended questions are as follows: “What brings you to me?” and “What bothers you about your nose?” Yes-or-no questions make it more difficult to sustain a dialogue. By conducting the interview in this way and listening attentively, the surgeon will learn why the patient desires a rhinoplasty. At the same time, he will gain an impression of the motivation and psychological makeup of the patient. The goal of every rhinoplasty is a satisfied patient. A successful operation will do much toward achieving this goal. A good result, however, does not necessarily mean a happy patient because the surgeon and patient may evaluate the result differently. Ultimately, the preoperative consultation is designed to answer two questions: • Can I solve the problem of the nose? • Will the operation solve the patient’s problem? While the first question can usually be answered after a detailed interview and examination, the second question is more difficult. It requires psychological insights and sensitivity on the part of the surgeon. Unlike a psychologist, he has only a short time in which to make his judgment. He need not make a precise psychological evaluation of the candidate, but he must be able to answer the two key questions as a basis for deciding, “Should I operate on this patient, or are his/her complaints ‘inoperable’?” The physician should explain the effects of the desired changes on the face. A simple hump removal can result in a long nasal dorsum and may even worsen the overall appearance and “personality” of the face. Some patients require extra help in understanding the complex effects of rhinoplasty. Many patients also lack appreciation for small morphological variants such as a bifid tip, minor tip asymmetries, or an indistinct nasolabial angle. A smaller percentage has a very finely developed sense for all of the details in their own face. Starting from these very diverse wishes and demands for the outcome of an aesthetic rhinoplasty, the physician can counsel and work with the patient to plan an individualized or even perfect result. Ultimately, however, the plan of operation is determined by the patient’s own desires. During the preoperative consultation, the surgeon has already had a good opportunity to inspect the patient’s facial features. The nose should be assessed in relation to the overall appearance. A long nose is appropriate for a tall stature. A high nasal dorsum emphasizes individual characteristics more than miniaturized forms. The nose is evaluated within the context of the facial features from the front, from the sides, and from below. Polycleitus (ca. 450–410 BC) was the most important Greek sculptor next to Phidias. Many of his bronze statues, preserved as marble copies, are major works from the Classical era of Greek art.1 Doryphoros is perhaps his best-known statue and embodies the principles set forth in his treatise The Canon (preserved only in fragments) on the proportions of the human body. The Canon begins with a detailed system defining the ideal relative proportions of the various parts of the body, known in classical antiquity as symmetry. This symmetry of the human body became a guiding principle for painting, sculpture, and architecture, and a hallmark of aesthetics. The classical teachings on body proportions received renewed attention during the Renaissance. The monk Fra Pacioli di Borgo worked extensively with proportions and aesthetics in medieval Venice. In 1509, he published a book in which he announced the discovery of the golden section: If we are asked to divide a line asymmetrically, we can do so at any number of points, but there is one section that is most aesthetically pleasing to the eye. This section divides the line into two segments called a and b. The ratio of the shorter segment to the longer segment (a/b) is the same as the ratio of the longer segment to the whole line: a/b = b/a + b This principle is reflected in the branches of trees, for example, and in the ratio of the longitudinal and transverse axes of an egg. It demonstrates that proportionality and aesthetics follow geometric laws.2 The practice of dividing the face into equal thirds was introduced by Leonardo da Vinci (1452–1519) and was later modified by Powell and Humphreys.3 Defining ideal proportions for the human face is an important aid for the facial surgeon (see Chapter 3). A much more common goal in any given case, however, is to restore or preserve the harmony of the face with due regard for personal as well as ethnic characteristics.4–6 As Naumann7 put it, “The face must be viewed as a unit, and the nose should have a good structural relationship to the overall balance of the face.” There is a certain hierarchy of facial features. The personality radiates chiefly from the eyes. The nose should be “subordinate” to the eyes, i.e., it should form a smoothly curved line from the medial point of the eyebrow to the tip-defining point. This line should highlight the eyes and not distract from them.8 The nasal tip is defined by a roughly equilateral rhomboid. It is formed by the tip-defining points and by the supratip and infratip areas. The basal contour of the alae should form a gently curved line (“gull in flight”) (Fig. 5.1). Every face has two slightly different halves and shows some degree of physiological asymmetry. This becomes clear when photos of the right and left halves of the same face are assembled in a montage. Marked facial asymmetry, facial scoliosis, or unilateral hypoplasia may affect individual or multiple portions of the midface, for example, or may affect the maxilla or mandible. Fig. 5.1 Facial proportions and symmetry. (a) The face is divided horizontally into fifths (Leonardo da Vinci). (b) The face is divided vertically into thirds (Powell and Humphreys).3 Right half of the face. Symmetry is defined by the eyebrow-tip line, the facial midline, and the rhomboid shape of the nasal tip. Left half of the face. Asymmetry is often due to an asymmetrical eyebrow-tip line (pseudo-deviated nose), maxillary, midfacial, or mandibular hypoplasia (usually with a crooked mouth), an oblique nasal base (cleft lip and palate), or asymmetry of individual structural elements (upper lateral or alar cartilages). Midfacial asymmetries often result in dysgnathia and are associated with axial deformity of the nose. The correction of combined facial deformities and asymmetries requires particularly careful planning (Fig. 5.2a, b). Axial deformities of the nose may affect the bony or cartilaginous part of the nose or may affect both parts simultaneously, producing an S-shaped twisted nose. Two different eyebrow-tip lines create the impression of a pseudo-deviated nose. Saddle nose is marked by typical deformities that adversely affect facial symmetry. The dorsum and supratip areas are broad and depressed. The nasal base is broadened. The columella is low, and the nostrils have a transverse oval shape. The skin and connective-tissue type has an important bearing on the anticipated tissue reaction and wound healing, making it an important factor in preoperative planning. Thick, seborrheic skin is advantageous in that it can cover small irregularities in the osseocartilaginous supporting structures of the nose. Onlay grafts, tip grafts, and shield grafts can be used. Suture techniques are also available. Thick skin is more susceptible to wound healing problems than thin skin. An example is the postoperative pollybeak deformity, which is most common in patients with a thick skin type. Thick skin and thin cartilage are an unfavorable combination for rhinoplasty. Thin skin is advantageous for wound healing. Graft techniques should not be used on the nasal tip. In the cases where a bifid tip is present due to prominent alar cartilages, perichondrium or small fascial flaps can be placed beneath the skin of the nasal tip. The ideal skin type for septorhinoplasty is moderately thick skin. Besides interindividual differences, the thickness of the skin varies from the glabella to the tip. It measures 2 to 5 mm at the level of the paranasion, approximately 3.2 mm over the bony dorsum, and 2 to 2.2 mm over the rhinion. Lang reports a thickness of 7 mm over the alae and 5 mm over the tip.6 The skin is thinnest, then, over the rhinion. It is thickest and most glandular over the nasal tip, especially in persons with seborrheic skin. The connective-tissue type is indicated by skin wrinkling, tissue tension, and elasticity and mobility of the skin. A less firm connective-tissue type is often associated with an increased tendency for hematoma formation. The skin is loose and mobile. Any cutaneous scars from previous operations (e.g., goiter surgery) should be inspected to gain information on individual scar formation and possible keloid formation. Preexisting scars would be a reason to avoid an open approach. Numerous geometric points and lines can be used to assess the facial profile. They are used to evaluate the relative positions or displacements of specific structures, depending on the points that are emphasized in a given specialty. For example, an orthognathic surgeon will use completely different reference planes than an otorhinolaryngologist or facial surgeon. We are always dealing with one profile, however, and therefore we shall focus on several interdisciplinary landmarks.9 The nasion corresponds to the nasofrontal suture and should be located at the approximate level of the supratarsal fold. The paranasion is located at the deepest point of the sella nasi. The nasofrontal angle between the glabella, nasal root, and nasal tip should be between 125 and 135 degrees. The nasal dorsum consists of the bony dorsum and cartilaginous dorsum. The rhinion is located at the junction of the nasal bones and upper lateral cartilages. This region is called the keystone area because of its key importance in stabilizing the nasal dorsum. It marks the cranial point of attachment of the cartilaginous nose at the center of the face. The nasal dorsum should be high and straight, or perhaps slightly convex, with the rhinion as its point of maximum prominence. From there the nasal profile descends straight to the pronasale in males, while in females it should form a slight depression at the level of the anterior septal angle, called the supratip break. From the pronasale, or tip-defining point, the profile curves smoothly to the subnasale, interrupted by a small break at the level of the columella–lobule junction. Thus, a double break exists in the nasal profile between the pronasale and subnasale. The size of the nasolabial angle determines the cranial or caudal position of the nasal tip and thus the length of the nose from the paranasion to the pronasale. The nasofrontal angle should be > 95 degrees.10 The length of the upper lip should equal the length of the columella. Ideally, the columella describes a slightly convex line several millimeters below the slightly concave alar margin. We use our own modification of the “facial circle” described by Baud to define the three most important points for general profile analysis and evaluate their relationship in the facial profile. Instead of the external auditory canal, we use the upper border of the tragus (corresponding to the porion) for measuring the radius to the pronasale. This point corresponds to the reference point for the Frankfurt horizontal (canthomeatal plane) in the Krönlein system (Fig. 5.3). The line from the porion to the pronasale forms the radius of a circular arc about the face. Ideally, the trichion and pogonion are located on the periphery of that circle. Overprojection of the nose is characterized by a posterior displacement of the chin (soft-tissue pogonion) and the frontal hairline. A relative retrusion of the chin or forehead can also be recognized. This type of analysis provides guidelines for the best way to achieve a harmonious profile. The goal of a septorhinoplasty is not just to alter the nose but to match the nose to the chin and forehead in a way that produces an aesthetically pleasing profile. The aesthetic impact of a sloping forehead or receding chin, for example, can be improved by nasal surgery alone (Fig. 5.4a–f). The nasal dorsum consists of a bony and cartilaginous portion. The relationship of these two components influences preoperative planning. Long nasal bones will adequately stabilize the nose. Short nasal bones are an indication for spreader grafts. These grafts will prevent stenosis of the nasal valve and pinching of the alae (Fig. 5.5a–d). Besides nasal shape, the profile is critically influenced by the position of the maxilla and mandible and by the typical deviations that occur with gnathic anomalies. Schwarz has identified nine different profile types in orthognathic surgery. The following reference lines are used11: • Canthomeatal plane (Frankfurt horizontal). • Nasal perpendicular of Dreyfuss. • Orbital perpendicular of Simon. Three typical variants are distinguished based on the relationship of the subnasale to the nasal perpendicular: • Average face: subnasale is anterior to a vertical line through the nasion. • Protruded face: subnasale is posterior to a vertical line through the nasion. • With a straight or retruded face, the pogonion shows the same degree of displacement as the subnasale. Anterior or posterior sloping facial types are distinguished according to the displacement of the soft-tissue pogonion. Two facial reference lines are used in distinguishing between straight, convex, or concave profile types: • A straight line from the forehead to the margin of the upper lip. • A straight line from the margin of the upper lip to the soft-tissue pogonion. Straight profile: Both reference lines form a straight line. Convex profile: Relative retroposition of the pogonion. Concave profile: Relative anteroposition of the pogonion (Fig. 5.6). The classic Angle classification of sagittal malocclusions was introduced in 1907.12 A concave soft-tissue profile signifies an Angle class II malocclusion, while a concave profile indicates an Angle class III relationship (Fig. 5.7). There are several reasons why these concepts from orthognathic surgery are important for the rhinosurgeon: • With regard to the timing of profile-correcting rhinoplasty in adolescence, it should be borne in mind that jaw growth continues until about 16 years of age in girls and until about 18 years in boys. • Gnathic abnormalities lead to typical profile changes: • The position of the nasal tip is influenced by the position of the jaws and midface. For example, an anterior sloping face can cause overprojection of the tip. The shape of the nasal base is determined by the height ratio of the lobule to the columella, which is normally 1:3. The nares have an elliptical shape. The shape of the tip can be accurately assessed by viewing the nose from below. A boxy tip has a squared-off shape. A long-presumed interdomal ligament does not exist.13 The width of the nasal tip is determined by the shape of the alar cartilages, the skin, and the interdomal fat. The critical anatomical structures that define nasal shape are the nasal septum and the lateral and medial crura and footplates of the alar cartilages. Bossing occurs when the transition from the dome area to the lateral alar cartilages is not harmonious. Often it takes several years for bossing to develop after rhinoplasty. Visual inspection of the nose is followed by palpation. Before palpating the nose, the examiner should inform the patient that it is the only way to obtain essential information on the resilience and tension of critical nasal structures. Cartilages can be reoriented and preserved only if the surgeon has been able to assess the cartilage tension by palpation. Visual examination and finger palpation are equally important in the nasal evaluation (Tardy10). 1. Palpate the junction of the cartilage and bony nasal dorsum in the keystone area. Rough spots, appositional bone growth following previous surgery, or an open roof can be appreciated in this way. 2a. Assess the tip recoil by pressing the nasal tip toward the anterior nasal spine with the index finger. 2b. Palpate over the anterior septal angle to assess the height and tension of the septal cartilage, especially in relation to the tip recoil. 3. The relationship of the bony nasal pyramid to the cartilaginous pyramid will affect surgical planning. Evaluate this by palpating over the nasal flank. Short nasal bones may be an indication for spreader grafts. 4. Palpate the structures of the nasal inlet to assess the shape and tension of the anterior septum, the size of the nasal spine, and the prominences of the premaxilla. 5. Bimanual palpation of the alar cartilage yields information on the shape, size, and consistency of the cartilage (Fig. 5.8).
Preoperative Management
5 Preoperative Management
5.1 Evaluation of the Face and External Nose
5.1.1 The First Impression
5.1.2 The Preoperative Consultation
5.1.3 Conducting the Consultation
5.2 Analysis, Clinical Geometry
5.2.1 Proportions and Symmetry
5.2.2 The Face from the Front
5.2.3 Skin and Connective-Tissue Type
5.2.4 Profile Analysis
5.2.5 Dentition and Profile
 Mandibular prognathism: protrusion of the pogonion.
Mandibular prognathism: protrusion of the pogonion.
 Retrognathia: retrusion of the pogonion.
Retrognathia: retrusion of the pogonion.
 Maxillary prognathism: protrusion of the subnasale and upper lip.
Maxillary prognathism: protrusion of the subnasale and upper lip.
5.2.6 The Nasal Base
5.3 Palpation
5.3.1 Manual Examination Techniques
Palpation
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree