There are many treatment options for AKs, including watchful waiting with careful sun-safety measures. Consideration must be given to patient selection, efficacy, risks, side effects, psychosocial
variables, cosmesis, compliance, cost, and duration of therapy in selecting the best treatment option for a given patient. Competent primary care providers often provide effective treatment for patients with a few, well-defined AKs using FDA-approved immunotherapy and cryosurgery (
Table 8-1). However, off-label treatment with immunotherapy and more advanced procedures should be referred to experienced dermatology specialists to avoid the risk of misdiagnosis, inadequate treatment, and complications.
Local therapy
When there are a few clearly identified AKs, localized therapy can provide prompt and effective treatment. The knowledge and experience of the clinician providing treatment will impact the patient’s experience and treatment outcomes.
Cryotherapy is the most widely used modality to treat AKs. It is a quick, effective, and generally well-tolerated in-office procedure. The lesions are destroyed by freezing with liquid nitrogen (-196.5°C), which crystallizes the tumor cells, producing necrosis and tissue destruction. Blisters often form and dry into crusts, usually healing within 1 to 2 weeks. Potential adverse effects include pain, hypopigmentation, or scarring, which may be of concern in cosmetically sensitive areas. The advantage is that it requires one visit for treatment, and
has been traditionally covered by insurers compared to prescription immunotherapies which can be more costly.
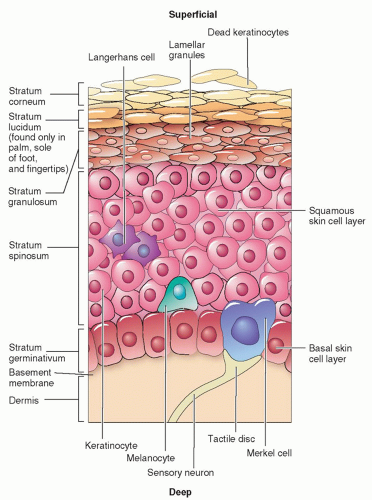
Curettage can be used to debulk hypertrophic AKs immediately following a shave biopsy, which is sent for histology to exclude invasive SCC. The provider uses a curette to scrape off the friable, damaged keratinocytes until normal, firm dermal tissue is reached. Electrocautery is used to control any bleeding. The procedure should only be performed by clinicians trained and experienced with this technique. Disadvantages of curettage include risk of hypopigmented, atrophic and/or hypertrophic scarring.
Field therapy
Patients can present with clinically well-defined AKs, as well as subclinical lesions in moderately and severely photodamaged skin. There are medical and procedural options that can provide field treatment to larger areas, treating both types of lesions.
Immunotherapy may be considered for both local and field therapy. There are several FDA-approved topical agents outlined in
Table 8-2 with varied mechanism of action, dosages, contraindications, side effects, and duration of therapy. In general, patients receiving topical therapy are advised to avoid application to the
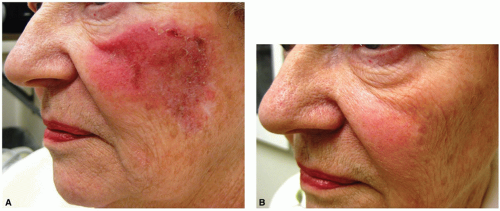
mucous membranes and UVR exposure during and immediately after therapy. Use of shade, full-brimmed hat, and sun screen are suggested if patients will be outdoors. Common side effects for almost all topical therapies include allergic contact dermatitis, burning, crusting, dryness, edema, erosion, erythema, hyperpigmentation, irritation, pain, soreness, and ulceration (
Figure 8-6A). Patients may struggle with the red, crusted appearance during treatment, but are usually pleased with the final cosmetic results. On the other hand, the advantages of topical immunotherapy are treatment of subclinical lesions and cosmetic outcomes (
Figure 8-6B).
Photodynamic therapy (PDT) is a form of phototherapy which utilizes a photosensitizing agent which is activated by a timed exposure to a light source. This process selectively causes destruction of the damaged cells. Many patients compare the experience to that of a severe sunburn. PDT has a better cosmetic result than cryotherapy and 5-FU; however, the treatment causes significant discomfort and burning. Patients must avoid all sun exposure for at least 3 days posttreatment. PDT is performed in dermatology offices.
Dermabrasion is an in-office procedure used occasionally for treatment of AKs. It physically removes the surface of the epidermis using a surgical sanding tool or laser therapy. The skin is red and abraded initially, but then heals with healthy keratinocytes.
Chemical peels (medium depth), using trichloroacetic acid or glycolic acid, exfoliate the stratum corneum and can be effective. The skin can become very red and irritated initially, but then skin heals with a soft, smooth texture. Deep chemical peels are rarely used due to risk of systemic and cutaneous complications.
Laser resurfacing with carbon dioxide or erbium: YAG lasers are used for the treatment of extensive actinic damage and epithelial dysplasia implicated in the development of aggressive skin cancer. Sustained efficacy with laser resurfacing has not been established.